Mouth cancer
Here we discuss in slightly more detail various issues to be considered in the choice and extent of treatment modalities, focusing on surgery and radiotherapy.
Issues to consider in the choice of treatment modality
Patient factors
The general health of a patient can have a major bearing on the choice of treatment modality to adopt. A large proportion of patients tend to smoke tobacco, drink alcohol and have significant related co-morbidities. Pre-existing medical problems such as heart and chest disease are common in patients with mouth cancer. In addition to fitness to survive general anaesthesia and surgery, complications are more likely to arise following surgery in such circumstances.
However, radiotherapy should not be considered an ‘easy option’ as an alternative. In medically compromised individuals it has substantial associated morbidity, including a mortality quoted in the literature for radical chemoradiation higher than that of surgery.
Patients should clearly be involved in the decision if they are competent to make decisions. Some patients rely on their carers, friends and family and it can be helpful to include them in the process. It has also been shown that patients with good family and social support tend to do better.
Tumour factors
In some instances, for example small tumours (stage 1 or 2) both surgery and radiotherapy are equally effective in terms of loco-regional control and survival. Then, other issues such as functional outcome, quality of life and morbidity as well as patient preference will help to decide on the most appropriate treatment modality. It is always worth remembering that while the other modalities can be repeated, radical radiotherapy is a one-off technique.
The proximity of certain structures to a tumour will influence the treatment modality. For example, where there is bone involvement, surgery is preferred to radiotherapy (better control and less side effects). Tumours involving the carotid artery or base of skull can mean not being able to achieve a clear margin in surgical removal (termed ‘not resectable’).
It is worth noting that what may be a ‘non-resectable’ (or non-reconstructable) tumour in one surgeon’s mind is entirely treatable in another’s. This variation is universal, the use of multidisciplinary teams (UK), tumour boards (USA) and other forms of multidisciplinary experts working together aim to reduce this but the variation will never reduce to zero. In practice, a small proportion of tumour margins are positive. Adjuvant radiotherapy (given after surgery) is indicated in such cases to improve control but is never as good as achieving histologically clear surgical margins (variously defined as 2 - 5 mm tumour-free margin histologically).
The presence or high risk of neck disease (lymph nodes in the neck affected by malignancy) is usually addressed by surgery. Certain tumour features such as large tumours, thicker lesions, tongue site and histological features (such as poor differentiation or perineural (direct) spread) may sway the decision towards neck dissection. There have been attempts at predicting the likelihood of lymph nodal metastases accurately but to date it remains an inexact science (for example, ca. 30% of clinical and imaging T2N0 tongue cancers will have at least micro-metastases in the neck).
More advanced tumours are better controlled with surgery, followed by adjuvant radiotherapy. Chemoradiation (combination of chemo- and radiotherapy) may have a role to play in poorly differentiated tumours, those with extracapsular spread of tumour from lymph nodes, or positive margins after surgery – all signs of a ‘high risk’ squamous cell oral cancer.
Clinician factors
Local expertise, resources and better outcome associated with a preferred modality within each team are practical considerations which often influence the treatment choice and can render national guidelines ineffective, even when apparent international ‘gold standards’ of care exist.
Metastatic disease in the neck
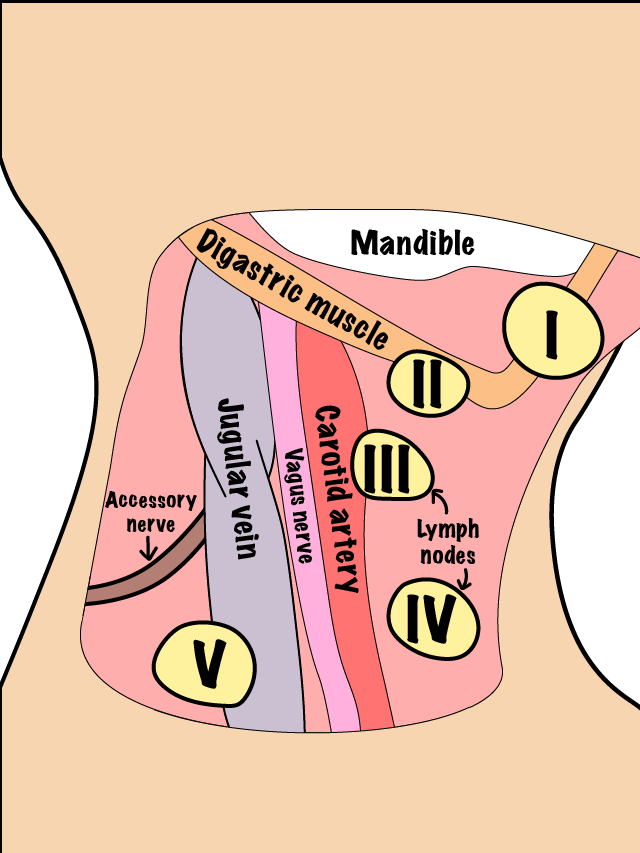
The lymphatic drainage of the oral cavity is generally an orderly and sequential flow into the submental, submandibular and upper jugular chain (spaces below the floor of the mouth). Malignant disease usually spreads in a similar orderly fashion. Exceptions are after previous treatment (either surgical or non-surgical, both change the pattern of lymphatic drainage) and the ‘skip metastases’ phenomenon (local lymph nodes are bypassed in this type of spread) for tongue lesions to the lower jugular chain (area of lymphatic drainage system in the lower neck). Figure 1 shows a sketch of lymph node locations in the neck.
The presence of metastatic disease in the neck worsens the prognosis by about 50%. Unfortunately, it is not always possible to predict the presence of disease in the neck accurately. We know that overall, about 30% of oral cancer is likely to have spread to the neck on presentation even though it is not palpable clinically.
The decision to treat the neck is dependent on several factors:
- presence of any enlarged lymph node(s) - presumed to be metastatic disease until proven otherwise
- there is a high risk of clinically undetected disease in the neck (occult metastases)
- poor compliance expected; if a patient is unlikely to keep follow-up appointments
- microvascular access for reconstructive free flap transfer is required.
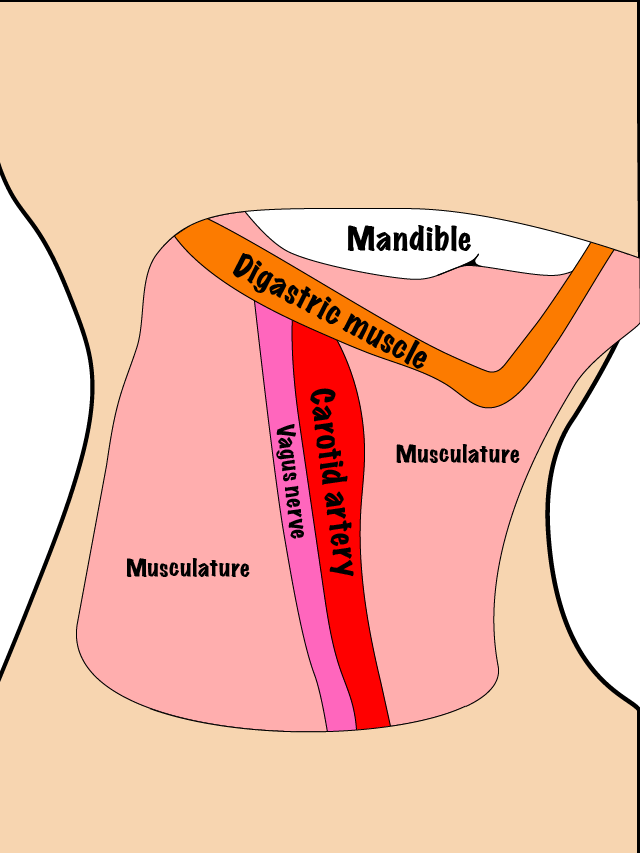
In order to achieve regional control of the disease, lymph nodes in the neck can be treated surgically with a neck dissection or by radiotherapy. Surgery is usually the preferred option. Figure 2 and Figure 3 schematically illustrate two versions of surgical neck dissection; a selective version (Figure 2) and a radical version (Figure 3).

Preferred treatment modalities in practice
Small oral malignancies can be treated effectively (with similar cure rates) using either radiotherapy or surgery. The aim is to keep to a single treatment modality, thereby reducing the side effects. In such instances, a better functional outcome (for example, tongue base better with radiotherapy) or fewer side effects (for example, surgery better when tumour is close to bone) will influence the decision. The patient’s preference after full information on the risks and benefits must also be taken into account.
Treatment of large tumours usually requires both modalities. The neck is treated surgically if the nodes are enlarged, involved, at high risk of being involved or where microvascular access is required.