Adrenaline
Adrenaline, also known as epinephrine in North America, occurs naturally as a hormone and acts as a neurotransmitter (Figure 1). In its synthetic form, it is also used as a medicinal drug. Amongst other hormones, adrenaline is synthesised in the body by specialised cells in the adrenal glands (two glands located on top of the kidneys); its natural precursor is the amino acid tyrosine.
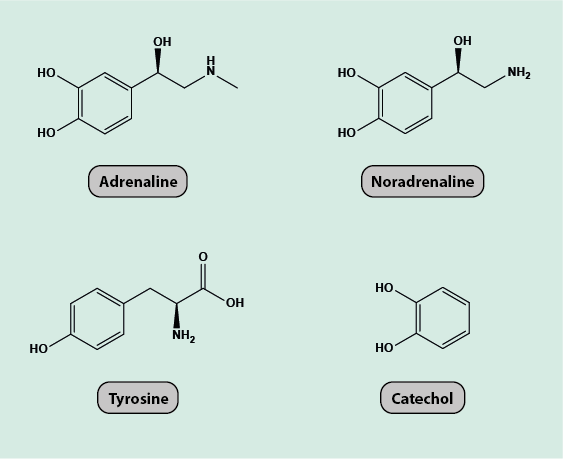
Adrenaline (as well as the closely related noradrenaline) is produced and released in response to emotional, physical or environmental trigger signals. Adrenaline plays an important role in the body’s sympathetic nervous system that responds rapidly to perceived danger (‘fight or flight response’) and stress. In this capacity, the main physiological effects of adrenaline include
- rapid release of glucose into the blood (for rapid energy provision to the body);
- increase of heart rate and blood pressure;
- relaxation of the smooth musculature in the respiratory tract (for rapid provision of enhanced oxygen supply);
- constriction of small peripheral arteries to divert and concentrate blood flow to brain, respiratory and cardiac systems;
- in addition, some interactions with the ‘reward system’ in the brain may occur (known in the context of the ‘adrenaline junkie’, seeking risk and extreme situations and activities (extreme forms of physical activity stimulate adrenaline release) and/or drugs).
These normal physiological properties of adrenaline also explain its role and functions as medication. Adrenaline can be administered in different ways, including inhalation and injection.
Adrenaline is the first-line choice of medication in the treatment of severe allergic reactions (anaphylaxis). Symptoms of anaphylactic shock are difficulty breathing caused by airway constriction, low blood pressure, urticaria (skin rashes) and facial swelling (angioedema; may affect other parts of the body too, especially hands and feet) and nausea. Adrenaline counters these effects by increasing the blood pressure (by its action as a vasoconstrictor and the resulting higher resistance in the peripheral vascular system), by improving the stroke volume of the heart, by bronchodilation (easing breathing by relaxing the muscles of the airway), and by decreasing angioedema. People with known severe allergies are advised to carry an emergency supply of adrenaline for immediate self-administration (by injection) for anaphylaxis. Another role as emergency medication of adrenaline is in the treatment of cardiac arrest, where adrenaline is used as a stimulating agent during resuscitation. It is vital to be aware that in cardiac arrest adrenaline is administered intravenously – this is the only time it is, when given or self-administered for anaphylaxis and similar reasons it is given subcutaneously or intramuscularly.
Asthma is another condition where the bronchodilation effects of adrenaline are helpful, especially where other treatments are not effective. The usual administration route for asthma is by inhalation.
Adrenaline is often included in local anaesthetics because of its vasoconstrictive properties, reducing superficial bleeding and prolonged anaesthesia. Local anaesthetics without a vasoconstrictor are virtually never used in the head and neck region because of this long established experiential rationale. Local anaesthetics with added adrenaline tend to be avoided in areas such as the fingers and toes.
Like any other medicinal drug, adrenaline has adverse effects that may make it unsuitable for people with hypertension (high blood pressure). Adverse effects include increased heart and breathing rates, dilated pupils, dizziness and general nervousness, excessive sweating. Repeated and/or high dose use of adrenaline can have adverse effects on the heart muscle tissue. Adrenaline interferes with the working of other neurotransmitters, in particular tricyclic antidepressants and the class of antidepressants known as MAOIs (mono-amino-oxydase inhibitors; also used to treat Parkinson’s disease), and beta-blockers (a class of drugs used to treat hypertension and other cardiovascular conditions).