Cyst
Surgical management of cysts is, by and large, some form of removal of the cyst.
Before this definitive surgical intervention, a decision has to be made if a biopsy beforehand is necessary or not. Preoperative histological diagnosis is an advantage in most cases. The problem is that even if performed under local anaesthesia, it subjects the patient to an unpleasant and potentially unnecessary second procedure. Clinically and radiologically unicystic lesions where the level of certainty of diagnosis is high can quite reasonably be treated primarily and the diagnosis confirmed postoperatively, accepting that very rarely a surprise diagnosis of keratocyst (see below), ameloblastoma or even a malignancy will occur. Equally, if there is a level of uncertainty with the diagnosis, a pre-definitive treatment biopsy is the sensible option.
Another consideration before definitive surgical treatment concerns anaesthesia. If the cyst is limited to the region of a single tooth, then treatment under local anaesthesia is usually adequate. Cysts in the posterior mandible and those spanning more than two or three teeth, as well as other extended cysts, are often better treated under general anaesthesia. These can only be approximate guidelines and the treatment plan should be tailored to the individual case, taking all other factors such as medical history, size and potential definitive diagnosis into account.
Epithelial cysts affecting the jaws
As far as jaw cysts are concerned, there are essentially three surgical treatment options: enucleation (cystectomy), marsupialization (cystostomy), or slightly more aggressive forms of removal, limited resection, in some cases.
Enucleation (cystectomy)
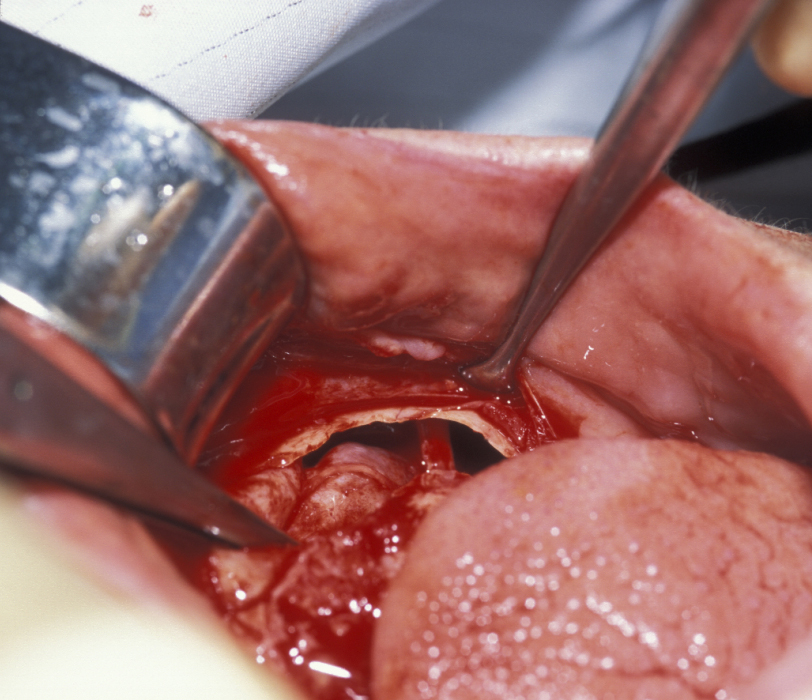
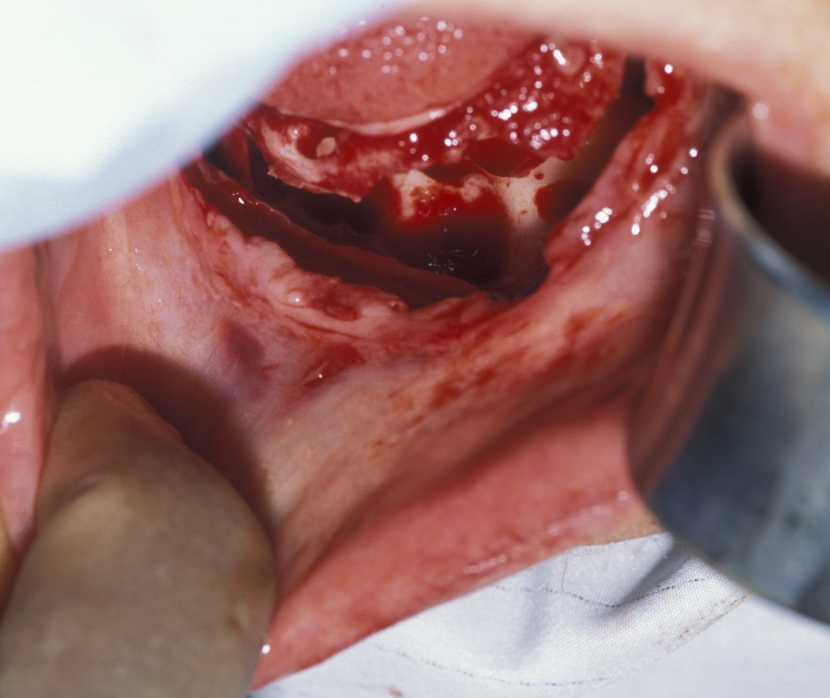
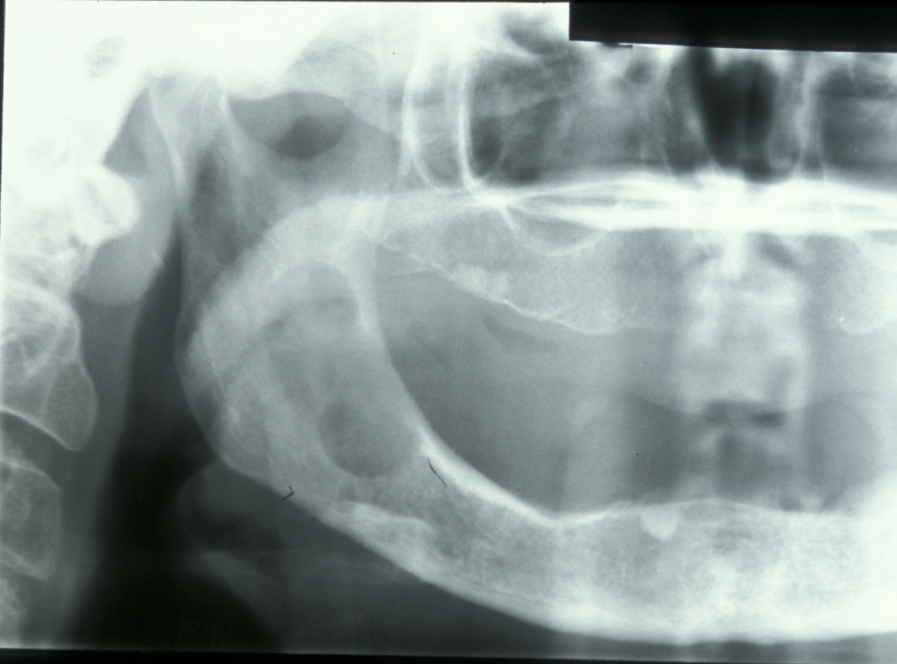
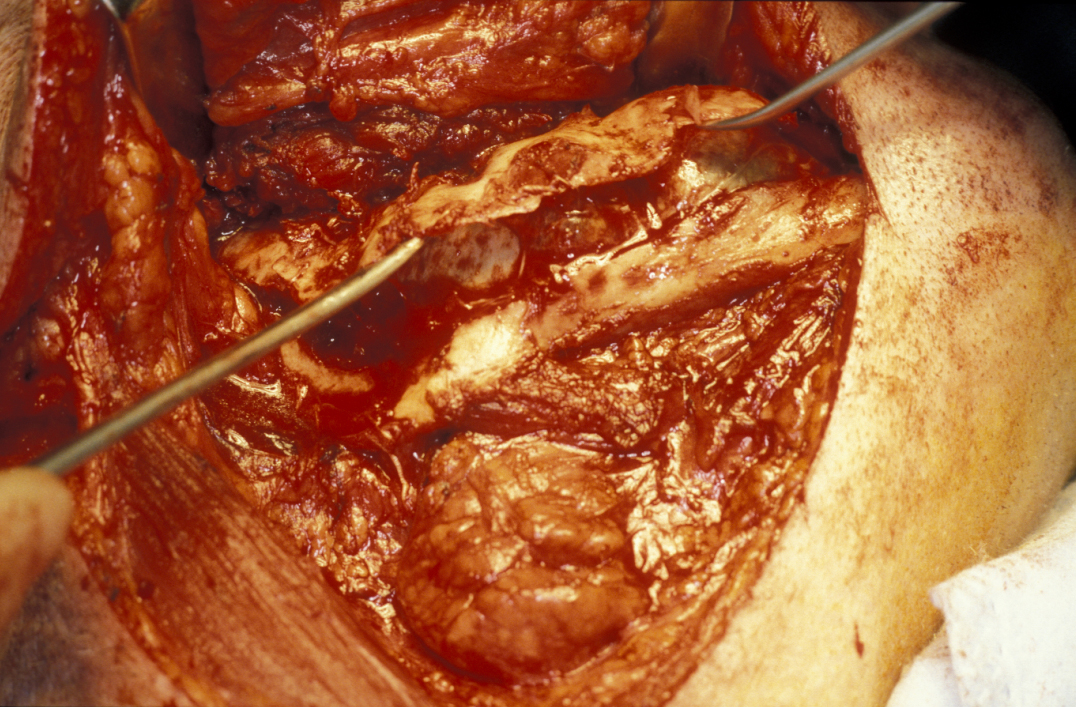
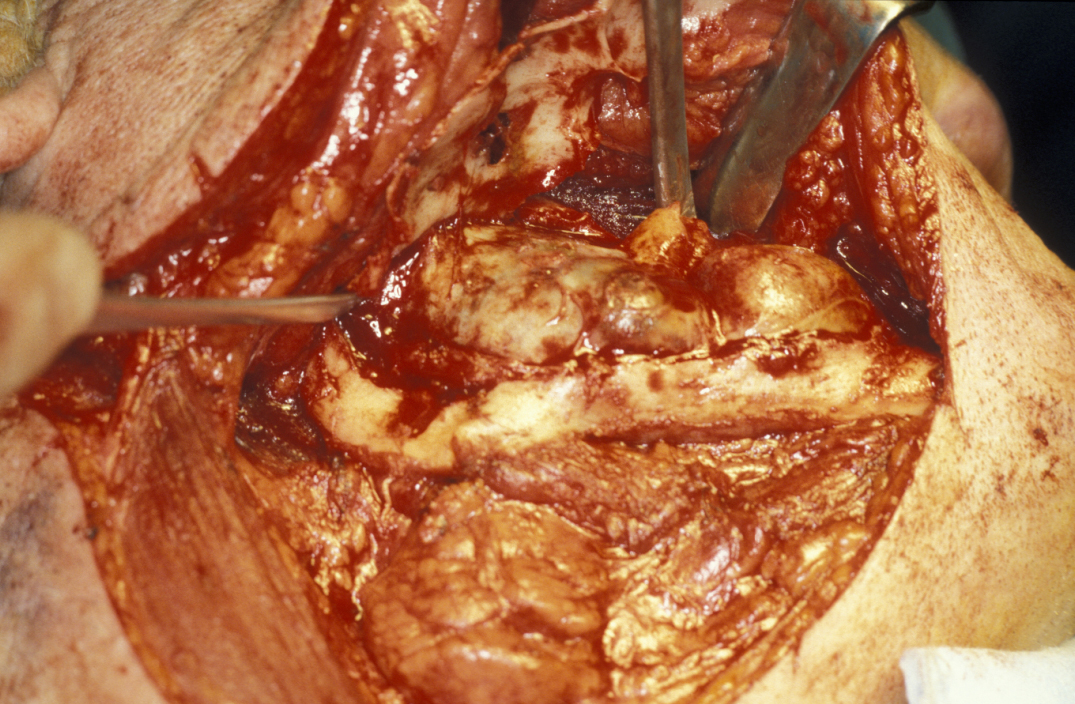
Enucleation involves the stripping away of the cyst lining from the resorbed bony cavity, resulting in a clean ‘hole’ in the bone. This deficit is filled by blood which organises into osteoid and then into new bone. There has never been an evidence-based demonstration of need to graft or fill the defect with synthetic substances. A step by step illustration of the procedure is shown in Figures 1 to 6.




Marsupialization (cystostomy)
Large cysts in which enucleation may result in extensive local damage or patients who are unfit for more extensive surgery can be managed by marsupialization. This involves exposing the cyst lining and removing a small window from the lining. This is then sutured to the mucosa. The cavity can then be packed with an antiseptic dressing and regularly changed as the cavity heals from underneath. A step by step illustration of the procedure is shown in Figures 7 to 9.



Decompression with oral grommets (tiny tubes) has been used in extremely frail patients. This procedure removes little or none of the cyst lining but places a small ‘ventilation tube’ which seems to delay growth, or may even reduce the overall size of the cyst. This procedure is essentially palliative as no formal diagnosis is reached and the bone defect remains in adults. In children some compensatory growth can occur.
Enucleation or marsupialization are the usual methods of choice for removal of:
- radicular cysts
- residual cysts
- dentigerous cysts
- eruption cysts
- nasopalatine cysts
- nasolabial cysts
Limited resection
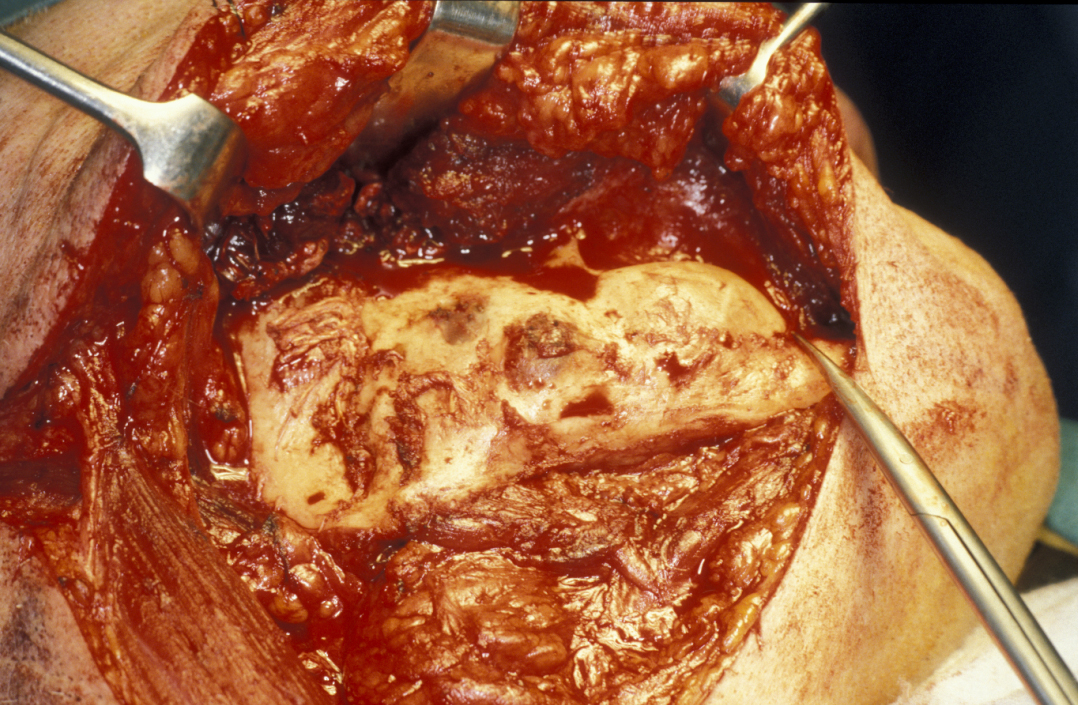
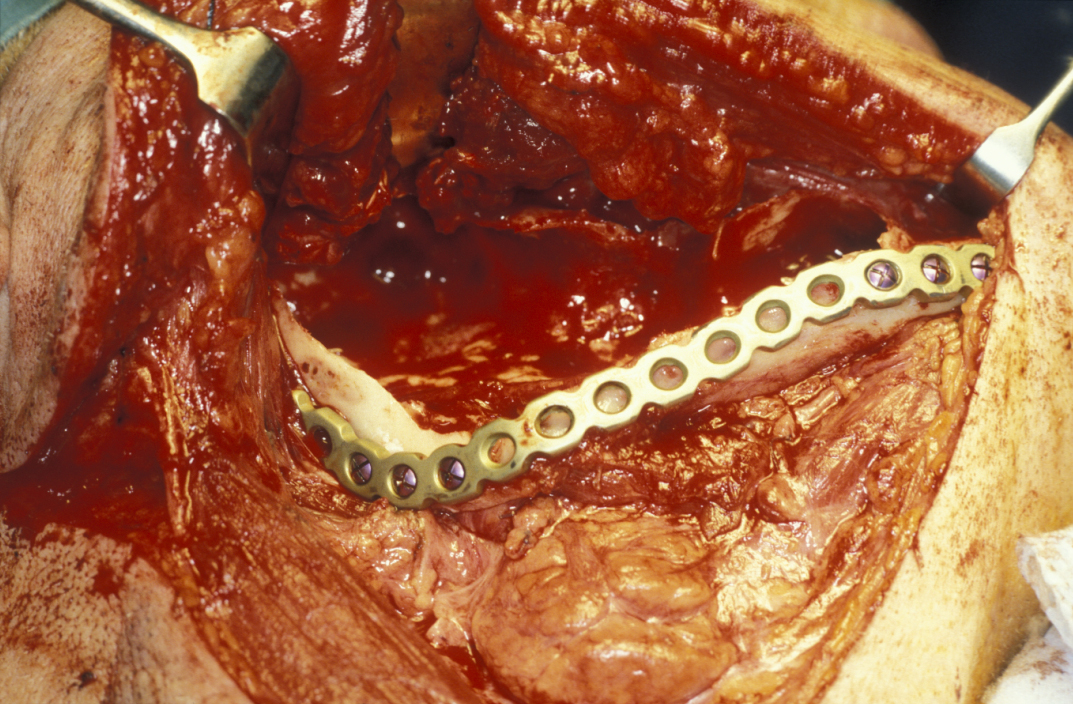
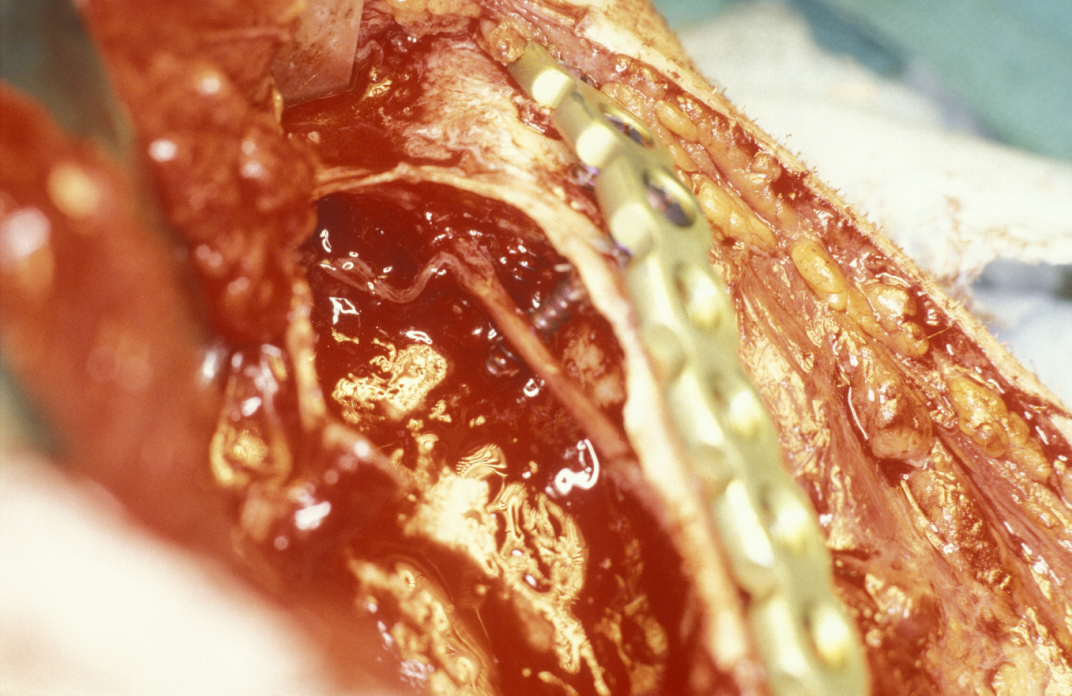
Limited resection represents a more aggressive form of removal of a cyst in that it will include the removal of bone in the vicinity of the cyst (a modified enucleation). It may also be a rim resection of the mandible (where a considerable portion of the mandibular bone is removed but a thin rim of the mandible is preserved to provide continuity of the bone). Treatment with Carnoy’s solution (a mixture of 60% alcohol, 30% chloroform and 10% concentrated acetic acid; applied locally directly after enucleation of a keratocyst) is popular with some surgeons. This is a way to reduce recurrence of keratocysts: the epithelial lining in keratocysts is very friable and therefore difficult to remove completely. Cryotherapy (local use of low temperature) may also have a role. A resection procedure with a reinforcing reconstruction plate is illustrated in Figures 10 to 15.
Limited resection is a method for the removal of:
- keratocysts / keratoystic odontogenic tumours (KOT)
- some aneurysmal bone cysts (see below)
Nonepithelial cysts affecting the jaws
Aneurysmal bone cyst
These are rare and different treatment methods have been advocated. Simple curettage (removing tissue by scraping or scooping) is usually all that is required. Some cases are complicated by severe bleeding and sudden enlargement. If this is the case the lesion may be very vascular and detailed investigations, including vascular studies, are advised. In these situations, limited resection is needed and curative.
Solitary bone cyst
These cysts often resolve spontaneously. However, the cavity is usually opened if only to confirm a diagnosis. Theoretically it could be healed by injecting the patients blood into the cyst to allow organization of clot into new bone.
Stafne’s idiopathic (unknown cause) bone cavity
No treatment is required.
Epithelial cysts affecting mouth, neck and face (other than jaw)
For these cysts affecting different areas of mouth, neck and face the usual preferred surgical approach is removal by complete excision.
Complete excision is the usual procedure for the removal of:
- oral dermoid cysts
- angular dermoid cysts
- mucoceles
- ranulae
- branchial cysts
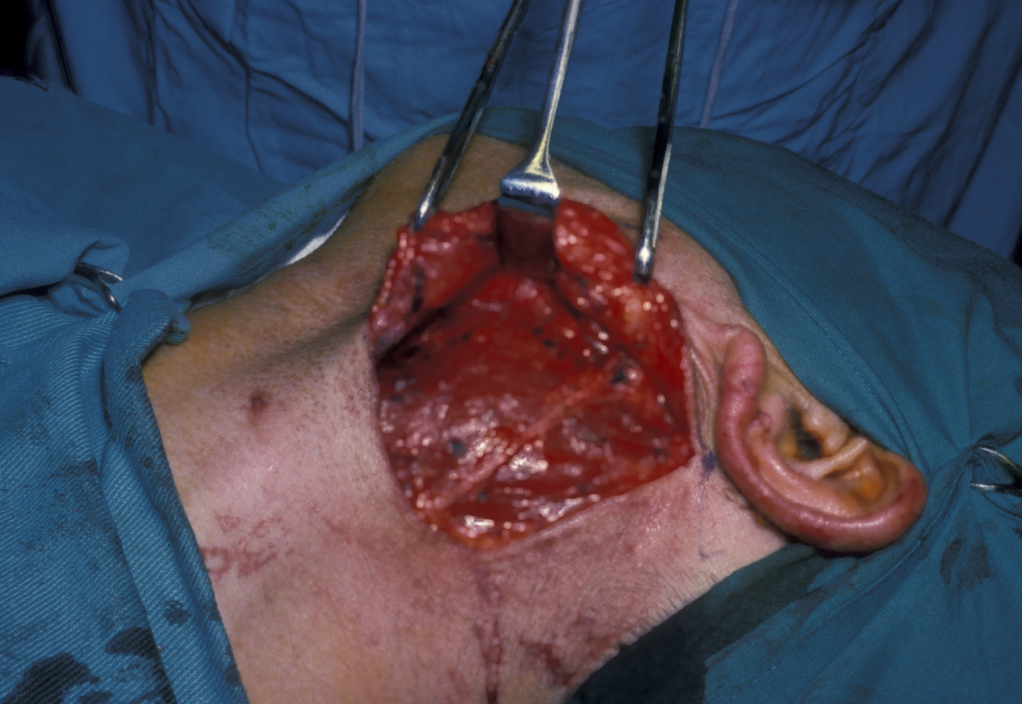
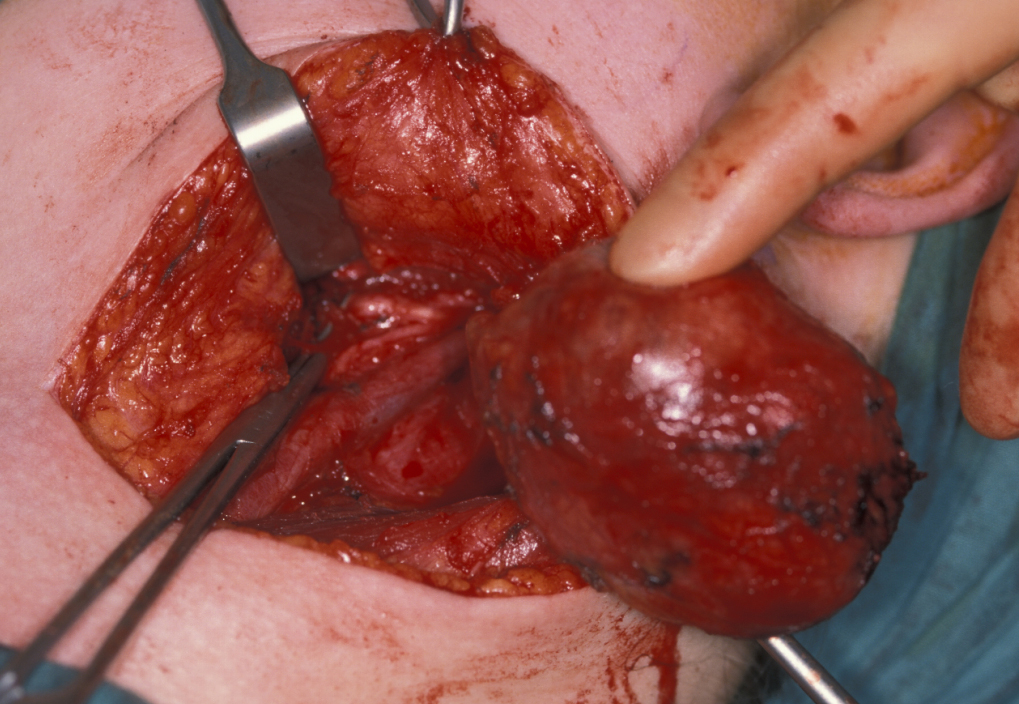
Figure 16 illustrates the distortion of the sternomastoid muscle by a branchial cyst, Figure 17 shows a branchial cyst being removed from beneath the sternomastoid muscle.
Cystic hygroma / lymphangioma (neck and mouth)
Surgical treatment of cystic hygroma (mostly in the neck) or lymphangioma (in the mouth) is usually by excision (picibanil injections into the cysts(s) can be an alternative: picibanil is a streptococcal antigen that causes selective fibrosis/sclerosis of lymphangiomas). Surgery is extremely difficult for microcystic lesions but comparatively simple for large, solitary macrocystic lymphangioma (the latter also happens to be easiest to sclerose with picinabil). Microcystic lymphangioma may require multiple excisions over many years.
Thyroglossal duct cyst
Excision of thyroglossal duct cysts requires the removal of the central portion of the hyoid bone to allow complete excision of the duct (see Figure 16).
