Cyst
Contents
Cysts occur in all parts of the body but are a prominent topic in a maxillofacial context: cysts are one of the most common reasons for people to attend a maxillofacial clinic. In particular cysts in the jaws are common. These cysts often are remnants of the complicated embryonal developmental processes involved in the emergence of jaws and teeth from immature cells in a foetus (developmental cysts).
Much is known about embryonal developmental processes in general but not all details about the origins of cysts are entirely clear. Also, there appear to be a number of different mechanisms by which cysts grow. Especially some of the biochemical growth mechanisms have recently been investigated in detail.
Here we give a brief summary of origins and growth of epithelial cysts of the jaws, along with some comments about diagnostic steps and histological findings. Beyond this brief summary, there is a large (and growing) body of literature concerned with properties of epithelial cysts.
Epithelial cyst formation; origins and growth
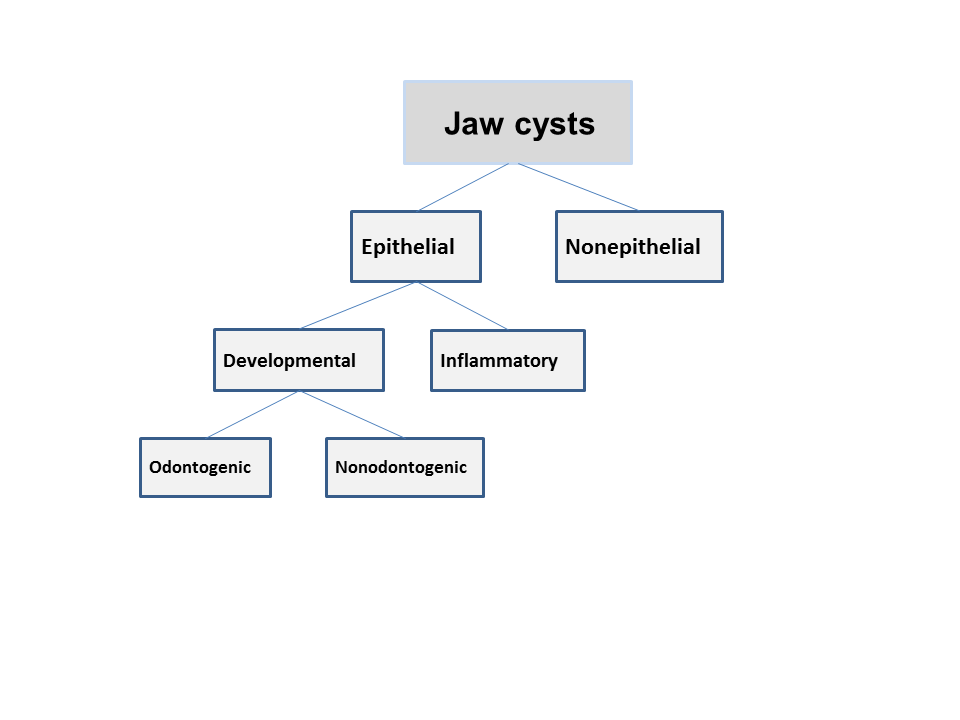
Figure 1 summarizes the classification of jaw cysts; the following discussion only refers to epithelial cysts.
Epithelium within the tooth-forming organ gives rise to these odontogenic cysts. The three different types of epithelium and the cysts they give rise to are described in Table 1.
| Type of odontogenic epithelium | Cyst |
|---|---|
| epithelial rests (glands of Serres) | odontogenic keratocyst lateral periodontal gingival |
| reduced enamel epithelium (enamel organ) | dentigerous (follicular) eruption |
| epithelial rests of Malassez (root sheath of Hertwig) | radicular |
Radicular cysts are inflammatory whilst the other odontogenic cysts listed in Table 1 are developmental.
Nonodontogenic cysts include nasopalatine (incisive canal), globulomaxillary, median and nasolabial cysts.
The relative frequency of epithelial jaw cysts is shown in Table 2.
| Type of cyst | Frequency (%) |
|---|---|
| radicular | 65-70 |
| dentigerous | 15-18 |
| nasopalatine | 5-10 |
| keratocyst | 3-5 |
| lateral periodontal | <1 |
These figures can vary a little; for example keratocysts seem twice as common in German-speaking countries than the UK.
There are several theories proposed for mechanisms supporting the growth of epithelial cysts:
Hydrostatic theory - central epithelial necrosis results in a hyperosmolar cyst fluid, leading to high osmotic pressure and causing fluid from surrounding tissues to move into the cavity. This mechanism depends on the type (and thickness) of epithelial lining of the cyst. Most cysts are roughly spherically shaped, fluid-filled cavities, strongly suggesting that some non-directional force, such as hydrostatic pressure plays a role in growth. The increase in hydrostatic pressure resulting from fluid influx into the cavity is thought to cause (or contribute to) expansion of bone.
Proliferation of lining theory - toxic products of necrotic pulp or bacteria lead to degeneration and liquefaction necrosis of granulation tissue. The epithelium then proliferates to surround the area. The exact biochemistry underlying this mechanism is not yet fully understood.
Prostaglandin theory - epithelial cells within the lining produce prostaglandin release in response to some stimulus. The prostaglandins (and/or other bone-resorbing factors) cause bone resorption, thus resulting in expansion of the cavity. It is thought that the increased bone resorption is caused by stimulation of osteoclast formation.
Special diagnostic investigations
These are specific tests carried out to help reach a diagnosis.
Radiography - this is an essential investigation for establishing the outline extent of the lesion. It also shows the relationship of teeth and associated anatomical structures such as the inferior dental nerve. Cone beam CT scans (allowing three-dimensional image reconstruction) can provide a more detailed picture to aid diagnosis or associated structures in relevant cases.
Aspiration - this can be helpful in establishing a diagnosis:
- cheesy white material suggests a keratocyst
- solid mass suggests possible tumour or very thick keratin mass
- pus indicates an infected cyst or abscess (also foul smell)
- blood can suggest either an aneurysmal bone cyst or, more importantly, a vascular malformation
- air indicates that the needle is within the maxillary antrum or it indicates a solitary bone cyst
Various tests can be carried out on the aspirate:
- culture and sensitivity - if infection is suspected
- stain for keratin - keratinised squames are suggestive of a keratocyst
- soluble protein content - keratocysts have low soluble protein content because the cyst is filled with keratin, which is mostly insoluble protein. The aspirate therefore contains less than 4g/dl soluble protein. Cysts and tumours generally have soluble protein concentrations greater than 5g/dl
- electrophoresis - not often used nowadays but the protein bands are compared with normal serum as a control. Electrophoresis can indicate keratocysts because the keratin has little soluble protein compared with serum
Incisional biopsy - if a lesion is very large or if there is suspicion of it being more than a simple cyst (for example, a keratocyst or ameloblastoma), then a biopsy is indicated.
Histological features
Histological features of odontogenic cysts
Radicular cysts (inflammatory) - these cysts develop within a periapical granuloma. The epithelial lining is nonkeratinised squamous epithelium and it is hyperplastic with occasional mucous metaplasia. Rushton bodies (peculiar glassy structures) may be found in about 10% of odontogenic cysts, and they only occur in odontogenic cysts because the material is only secreted by reduced enamel epithelium. Cholesterol clefts are often present in inflammatory cysts but are not diagnostic. A mixed inflammatory infiltrate of neutrophils, lymphocytes and plasma cells is present.
Dentigerous cysts (developmental) - these cysts are attached to the unerupted tooth at the amelocemental junction, and although this cannot be seen radiographically, it can be seen at operation. The epithelial lining, which is derived from the reduced enamel epithelium has a flat basement membrane and is a feature of developmental cysts (dentigerous cysts and keratocysts). If the cyst is infected there will be an inflammatory response, similar to a radicular cyst.
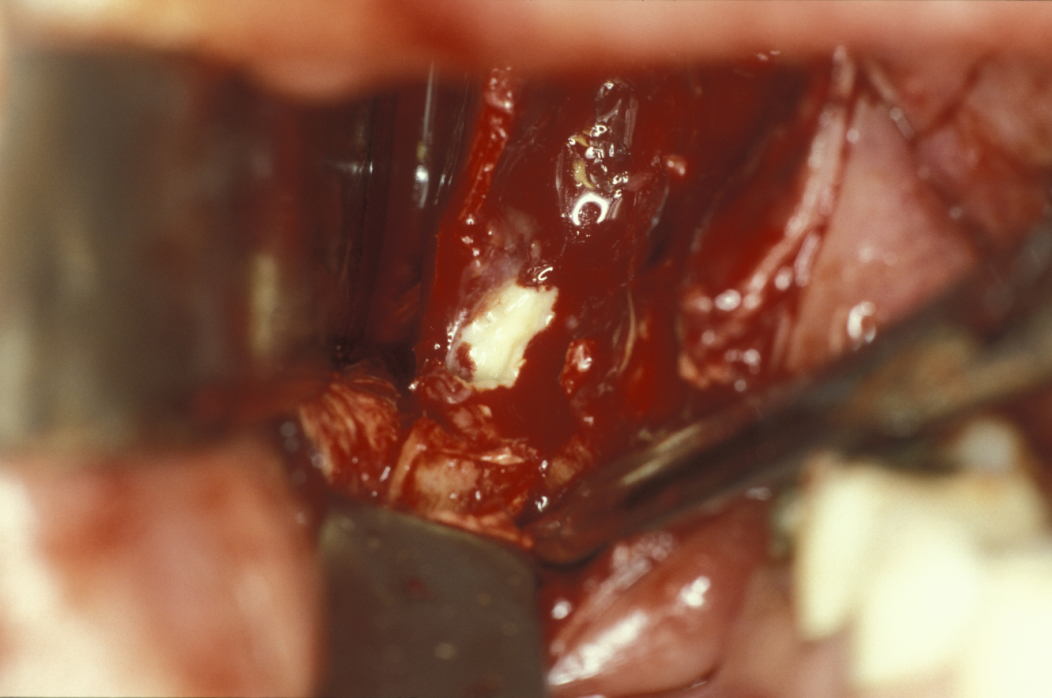
Keratocysts (developmental) - the epithelial lining in keratocysts is very friable and therefore difficult to remove completely. Microscopic ‘satellite’ cysts can be left behind at operation and this creates the problem of recurrence. The epithelium is keratinised and the keratin is shed into the lumen of the cyst producing the characteristic cheesy contents (see Figure 2). The basement membrane is flat as in a dentigerous cyst with palisaded columnar basal cells.
Histological features of nonodontogenic cysts
Nasopalatine duct cysts (developmental) – the epithelial lining of these cysts is variable among respiratory, columnar, cuboidal and squamous epithelium as it approaches the oral cavity. The specimen may contain the neurovascular bundle.