Swallowing
Swallowing is one of our bodies’ functions that we rarely pay attention to, we take it for granted – until something goes wrong. Swallowing is a complicated process involving a large number of feedback loops, including voluntary and involuntary steps in the process. Several areas of the brain have been identified as ‘control centres’ for regulating the swallowing process. Under normal circumstances we swallow about 500 to 2000 times daily, swallowing requires the concerted actions of about 50 pairs of muscles and 5 main cranial nerves (nerves in the skull). It will not come as a surprise that it takes only a little disturbance of this complicated system to produce problems of some sort with swallowing (dysphagia).
An understanding of the swallowing process when everything functions as it should is helpful (we believe) for understanding the various ways in which swallowing can be compromised and the ways in which such difficulties can be either circumvented or at least much reduced in many cases.
Here we sketch
- the normal course of events in the swallowing process (for solid and liquid foods);
- how our bodies actually acquire the ability to swallow safely (starting with the foetus up to the age of around two years).
The normal swallowing process
The swallowing process is best described as a series of phases. These phases are different for liquid and solid / semi-solid foods (liquids are rapidly and directly transferred from the oral cavity to the oesophagus (gullet)). For solid / semi-solid foods the location of the bolus (lump of solid / semi-solid food) roughly defines the phases of the swallowing process:
- pre-oral (anticipatory) phase
- oral preparation phase
- oral phase
- pharyngeal phase (throat)
- oesophageal phase (gullet)
The anticipatory, pre-oral phase precedes the opening of the mouth, before putting food in the mouth. At this initial stage the food is checked (look, smell, temperature, consistency) for suitability; this check has voluntary and involuntary components. The final step of this phase is the sensory input from the lips from touching the food, before accepting or rejecting it.
The oral preparation phase continues the careful examination of the food that has now been put in the mouth (smell, taste, temperature and volume). This stage is largely ‘automated’ but is under voluntary control: if the food fails the examination, it can be spit out at this stage. If the food passes the examination, at this stage some early alert for the swallowing reflex is initiated.
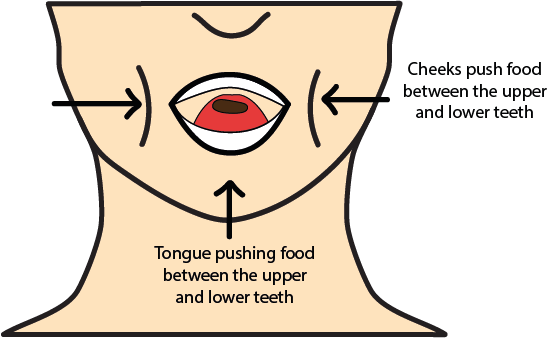
The main task for the oral preparation phase is to form a bolus (lump of food) suitable for swallowing, and placing it according to the stage of the process. This involves chewing and a thorough mixing of the food with saliva. Chewing in itself is quite an engineering achievement, making use of all the many subtle (and not so subtle) anatomical features of the jaws, teeth, tongue, facial muscles and several of the cranial nerves. For example, sensory controls avoid injury by biting oneself.
At this stage we also can talk without danger of choking on the food. In particular the occlusion of teeth in the upper and lower jaws is a fascinating construction, allowing for cyclical chewing movements that continue until the bolus is accepted (by receptors) as ready to move on. Figure 1 gives a brief and much simplified summary of the oral preparation stage and how the chewed food is moved around the mouth for proper bolus formation.
Olfaction (the smelling of food) plays an important role toward the end of this phase: this sensory information is forwarded via the (nasal) receptors to the control loop that eventually triggers (or prevents) the swallowing reflex. The duration of the oral preparation phase varies strongly amongst individuals, but there seem to be some common patterns of particle size of certain foods after chewing and before swallowing.
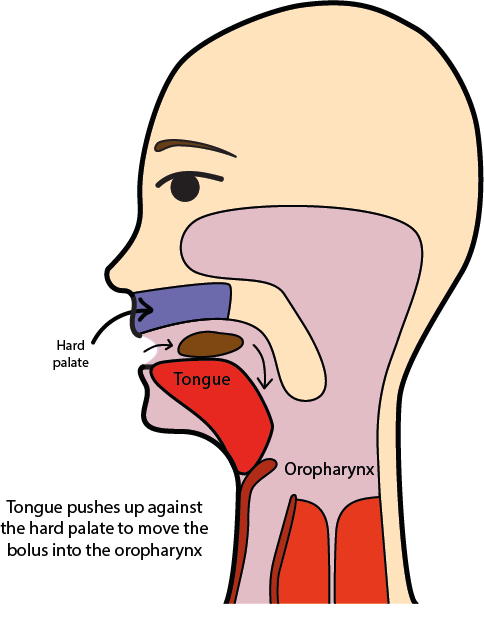
During the oral phase the bolus is transported from the mouth to the oropharynx (area at the back of the mouth below the soft palate and connecting to the upper part of the throat), as is symbolised in Figure 2 and Figure 3.
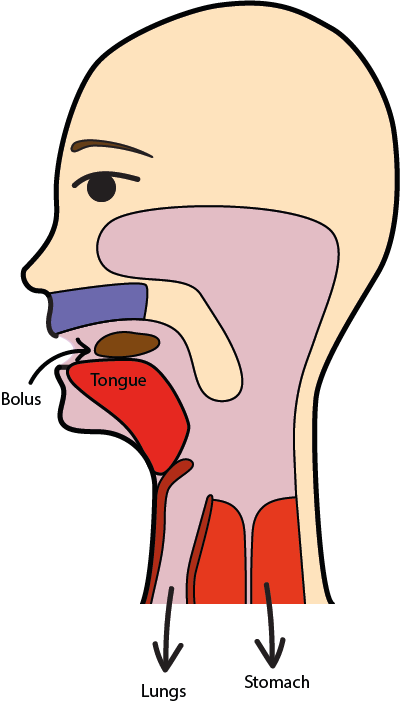
The oral phase is under voluntary control; it starts with a range of motions of the tongue which essentially pull the bolus along the centre of the tongue from the front and middle of the mouth to the back. This transport motion is enabled by the successive actions of a whole range of muscle groups placed alongside and at the bottom of the tongue (see Figure 3 for a much simplified cartoon version of the bolus transport). This transport motion of the bolus is supported by a closed mouth. The oral phase ends with triggering the swallowing reflex when the bolus reaches the trigger area at the back of the tongue / mouth.
During the pharyngeal phase the transport / backward motion of the tongue helps to push the bolus into the hypopharynx (the lower part of the pharynx; the pharynx is the passage leading from the oral cavity to the larynx (voice box) and connecting to the oesophagus (gullet); air passes through the pharynx on the way to the lungs, food passes through the pharynx on the way to the oesophagus). This bolus transport requires the concerted (and powerful) action of a number of muscles and nerves.
Figure 4 shows a cartoon version of this stage of the swallowing process; the sketch highlights the need to protect the nasal cavity and the airway from food entering them. The soft palate is pushed back and blocks off the nasal cavity, the airway is protected from food entering by a series of blocking steps by epiglottis (a flap of cartilage and mucosa, at the back of the tongue) and larynx. During the swallowing passage at this stage, there is a reflex triggered which stops breathing during this stage; the entire pharyngeal phase lasts for up to a second.
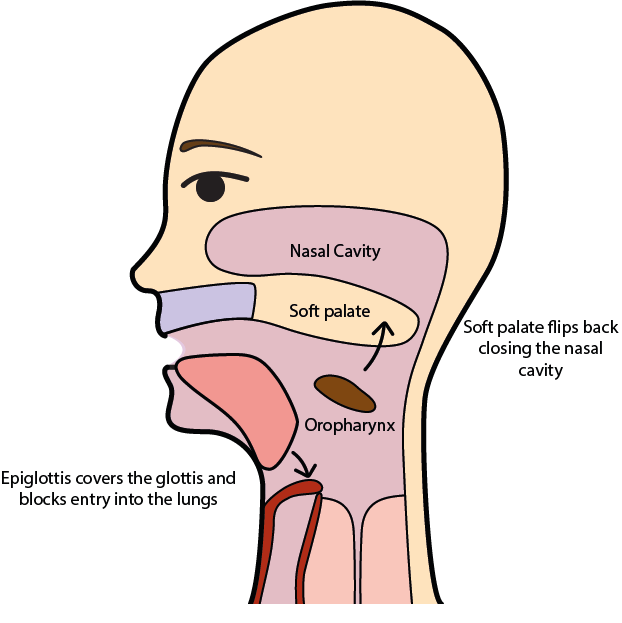
The swallowing reflex is involuntary (it is tactile but thermal stimuli such as cold foods can help with muscle tone). Solid and semi-solid foods are being swallowed in cascades, it is thought that a volume of about 5 ml (content of a teaspoon) is the most comfortable volume to swallow. The end of the pharyngeal phase is marked by the opening of the upper part of the oesophagus.
The oesophageal phase is completely under involuntary control. Transport of the food bolus through the approximately 25 cm long elastic muscle tube making up the oesophagus occurs in peristaltic waves. Figure 5 shows a sketch of this stage.
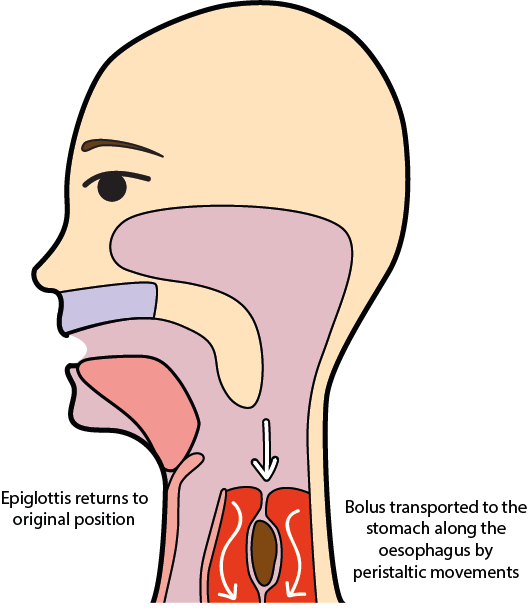
The initial transport wave takes several seconds (between 4 s and 40 s) for the bolus to travel to the stomach. A secondary wave is initiated mechanically by left-over food particles sticking to the wall of the oesophagus, essentially for cleaning up the passage way. The oesophagus maintains a high longitudinal muscle tone so that, in principle, we can swallow when in a headstand. However, in an upright position gravity helps with the bolus transport.
Swallowing liquids is a challenging task. An old-fashioned but perfectly valid definition of a liquid is that it will fill any cavity it can reach, here the oral cavity when we take a sip of a liquid. Swallowing a liquid is a rapid and direct passage, usually omitting the oral phase, which may only take a fraction of a second for the initial stages, overall less than a second to reach the stomach. This speed of events, together with the space-filling properties of liquids make it more difficult to swallow liquids safely. These considerations about the swallowing of liquids include saliva (of which we produce an estimated amount of 0.75 to 1.5 l daily)!
Development of swallowing abilities
Safe swallowing of a whole range of foods of mixed textures and temperatures is an ability which our body has to learn as it grows and develops, similar to having to learn how to walk, or talk. Sadly, for a variety of reasons our bodies also tend to unlearn the ability of competent swallowing when we get old and frail - dysphagia of some sort is a common, and often neglected, problem for many elderly people.
The very first, primitive swallowing attempts of a foetus can be observed around week 12 of pregnancy and it takes until approximately 4 years of age to develop competent swallowing abilities. The development starts in week 3 of pregnancy with the formation of a primitive mouth; followed by early embryonal structures that later on form face, nose, mouth, larynx and pharynx. From around week 10 the glottis (opening between vocal cords in the larynx) is open, from weeks 13 - 15 the foetus starts some early form of pharyngeal swallowing process where the motions of lips, mouth, pharynx and oesophagus are distinct from each other. Weeks 17 – 20 see some early practice of the foetus to suck, followed by the development of reflexes such as biting or choking. At this stage, the foetus stimulates the mouth and swallows up to 400 ml of amniotic fluid daily. From around week 32 of pregnancy, the foetus can suck and swallow so that babies born at this stage of pregnancy can be either breast or bottle fed.
After birth the sequential sucking-swallowing process is established, together with coughing and choking reflexes and some early primitive hand-to-mouth coordination. Early primitive reflexes get replaced by more refined motor and orofacial skills over the first year (as the brain develops). The anatomical oral proportions of a newly born are different from those of an adult. In a young baby the palate, without teeth, is flatter than in an adult and the airway and oesophagus are better separated from each other. That allows babies to breath without aspiration while they are sucking, it is only during swallowing they have to stop breathing (triggered by a reflex) like an adult.
At 2 months old, a baby learns to control their head position, alongside spontaneous mouth opening and closing of the lips. At 3 months old, the neck flexion improves; at 4 months old lip and tongue control have reached a developmental stage such that feeding is possible (this is in parallel to developing control over using the arms).
At 5 - 7 months old, overall body control and motor skills improve and for most infants drinking from a cup is possible, as is eating of soft foods, and the early choking reflex is reduced over time. At 7 - 9 months old, most infants are able to sit properly and support their torso; well-coordinated movements of tongue, lip and chewing have been learned at this stage. At 10 - 12 months old, the hand and finger coordination is a little more refined (pincer grip) and eating with fingers, biting and some controlled chewing are established and need practising.
Learning to walk and further improving manual motor skills at age 13 - 18 months is a parallel development with learning to talk and to eat foods of all consistencies and textures. At 19 - 24 months old most infants learn to eat independently with a spoon and to drink from a cup with properly closed lips.
It takes all the time from 24 - 48 months of age to further improve the various body motor skills (such as jumping, using scissors, and so on) as well as becoming fluent with feeding independently (if messily…) and competent at safely swallowing all kinds of foods.
Diagnostic methods, such as real-time MRI investigations, are important for the identification and assessment of swallowing disorders, especially because there are so many different such dysphagia conditions. Figure 6 and Figure 7 give an example by comparing the swallowing process of thickened pineapple juice in a healthy person (Figure 6) with the swallowing process in a person suffering from a degenerative muscle-wasting condition, IBM (Figure 7).