Anaesthesia
Maxillofacial surgery presents some specific issues for anaesthesia; below we briefly describe these.
Anaesthetic issues specific to maxillofacial surgery
Shared airway
Safe anaesthesia relies on an unobstructed airway to maintain gaseous exchange. This can be provided by the use of an endotracheal tube passed through the mouth or the nose into the trachea (windpipe). Alternatively, when isolation of the trachea is not essential, devices that lie on top of the larynx known as laryngeal masks (breathing masks) or ‘supraglottic airways’ may be used.
Intraoral surgery has the potential for disturbing the unobstructed airway. Similarly, anaesthetic airways placed in the mouth reduce surgical access and may be unsuitable. The needs of both the anaesthetist and the surgeon need to be balanced safely.
In many circumstances the use of a nasal tracheal tube provides the safest airway for intraoral procedures.
It is not uncommon for endotracheal tubes and supraglottic airways to become dislodged or obstructed during head and neck procedures. Anaesthetists must be constantly vigilant to protect the shared airway. Communication between anaesthetist and surgeon is essential for patient safety.
Patient comorbidities
Patients presenting for maxillofacial surgery are extremely varied. All age groups are represented and the very young and the very old present aditional challenges.
Anaesthetists grade patients using the 6 point ASA (American Society of Anaesthesiologists) score (see Table 1) which correlates comorbidities to mortality risk. Patients with high ASA scores might be declined surgery.
Table 1 The ASA score for patient assessment
| ASA classification | Description |
|---|---|
| 1 | A normal, healthy patient |
| 2 | A patient with mild systemic disease |
| 3 | A patient with severe systemic disease |
| 4 | A patient with severe systemic disease that is a constant threat to life |
| 5 | A moribund patient who is not expected to survive with the operation |
| 6 | A declared brain-dead patient whose organs are being removed for donation |
Oncology patients often have multiple comorbidities such as respiratory disease and coronary artery disease. This confers additional perioperative (during the operation) risks. Patients must be investigated prior to surgery and plans made for postoperative care.
Difficult Intubation
Difficulty with intubation and ventilation may be predicted but can occur unexpectedly. Patients posing problems with intubation include those with trismus (difficulty with opening the mouth), intraoral masses, previous radiotherapy.
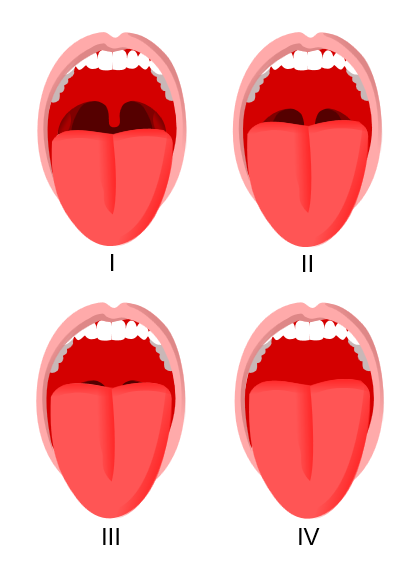
Difficult intubations may be predicted by examining the patient’s airway. The Mallampatti score (see Figure 1) assesses the ability to visualise anatomical structures through the mouth. The higher the score the more difficult are intubation and ventilation likely to be:
- Class I: the soft palate is completely visible
- Class II: the uvula is completely visible
- Class III: only the base of the uvula is visible
- Class IV: the soft palate if not visible at all.
There are many strategies to deal with intubation problems. Anaesthetists in the United Kingdom follow the Difficult Airway Society Guidelines. The final step in the guidelines is emergency surgical access through the cricothyroid membrane (elastic tissue in front of the thyroid).
Postoperative care
Careful consideration should be given by both surgeon and anaesthetist about the care of the maxillofacial patient following the procedure.
Some patients may go home the same day, others will require inpatient facilities. If the airway is at risk of obstruction (for example, by postoperative swelling), high dependency or intensive care is necessary. If airway obstruction is highly likely, it is prudent to place a temporary tracheostomy (surgical opening through the neck into the trachea (windpipe)). Temporary tracheostomies are used until intraoral swelling has subsided – often 4 to 6 days. Safe decannulation may be considered when a leak occurs around a tube when the cuff is deflated.
Patients with potential for airway obstruction must be nursed by speciality trained staff in appropriately equipped wards.