Broken bone
Fracture
Contents
The following information is quite technical, dealing with specific fracture repair techniques, depending on location & type of fracture(s). This section is organised in terms of locations, starting with mandible, then zygomatic complex (cheekbone) fractures, nasal fractures, midface fractures, frontal bone & frontal sinus fractures.
Treatment of mandibular fractures
Immediate treatment in the primary survey is rare. Early treatment involves analgesia, either in the form of nonsteroidal anti-inflammatory drugs or opioids. Oral or intravenous antibiotics are given because, by definition, all mandibular fractures passing through the tooth-bearing segment and periodontal ligament are compound fractures into the mouth and therefore contaminated (Condylar fragments and fractures which do not communicate with the periodontal ligament are closed injuries and do not require antibiotics. However if there is a cutaneous wound caused by the fracture fragment, or by penetration of a foreign body, they are compound fractures and so require antibiotics).
Displaced, mobile fractures are very painful. The placement of temporary stabilising wires around the teeth adjacent to the mandibular fracture will immobilize the fracture and make the patient more comfortable while awaiting definitive surgery under general anaesthesia. This can help to reduce the need for analgesics in the preoperative period.
Treatment Planning
Mandibular fractures with altered occlusion are best treated by surgery (excluding condylar fractures, see below). Fracture treatment involves reduction of bone ends and stabilisation to allow healing. Some minimally or undisplaced hairline fractures can be treated without surgery as long as the occlusion is not altered. Sometimes the patient will elect not to have surgery and will accept the slightly altered occlusion. Informed choice must be respected and documented in this instance. Close follow up is advised although the reality of trauma patient follow up in most countries and most published series is that they are a very reluctant patient cohort when it comes to hospital attendance.
Preoperative consent
Preoperative assessment of inferior alveolar nerve injury must be documented, as it may become worse postoperatively. Most mandibular fractures are approached transorally. External approaches are used particularly for edentulous (no teeth) body fractures and condylar fractures. These incisions cause a scar and there is a small risk of damage to the facial nerve. Placement of plates (whether they are intended to be permanent or to be removed) is likely, loss of teeth is possible, intermaxillary fixation (if used) may be necessary.
Mandibular Fracture Repair
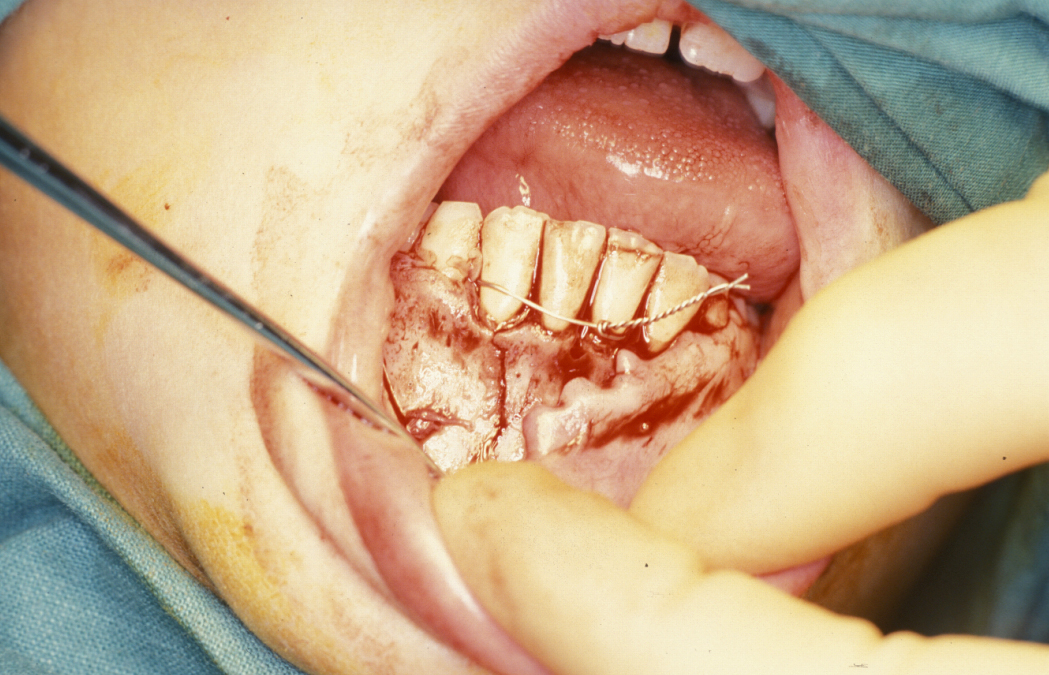
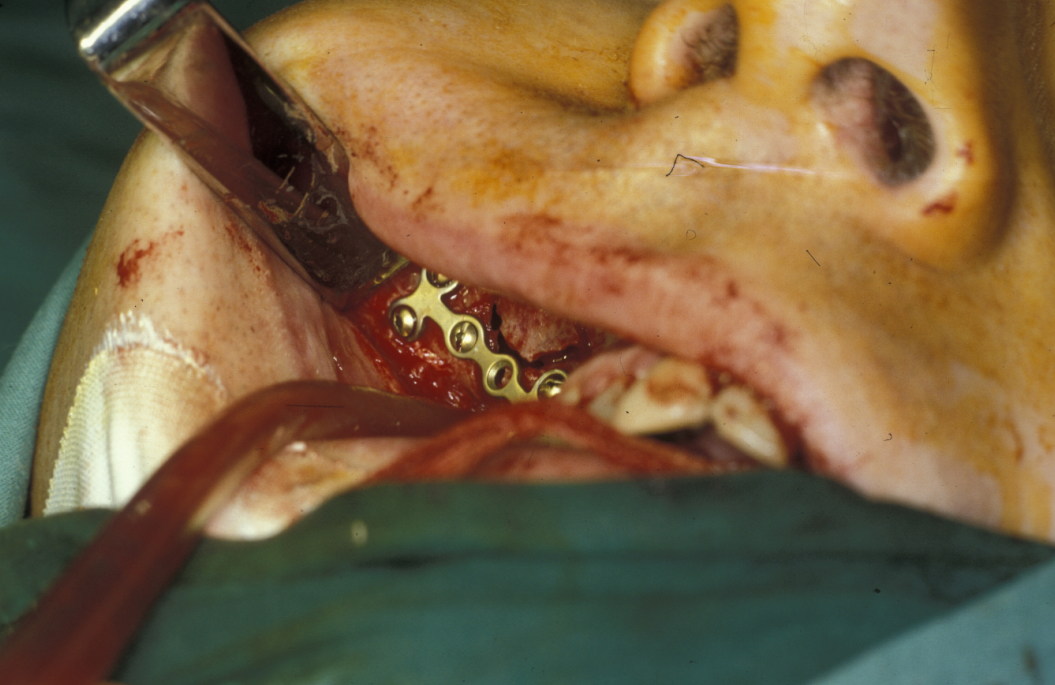
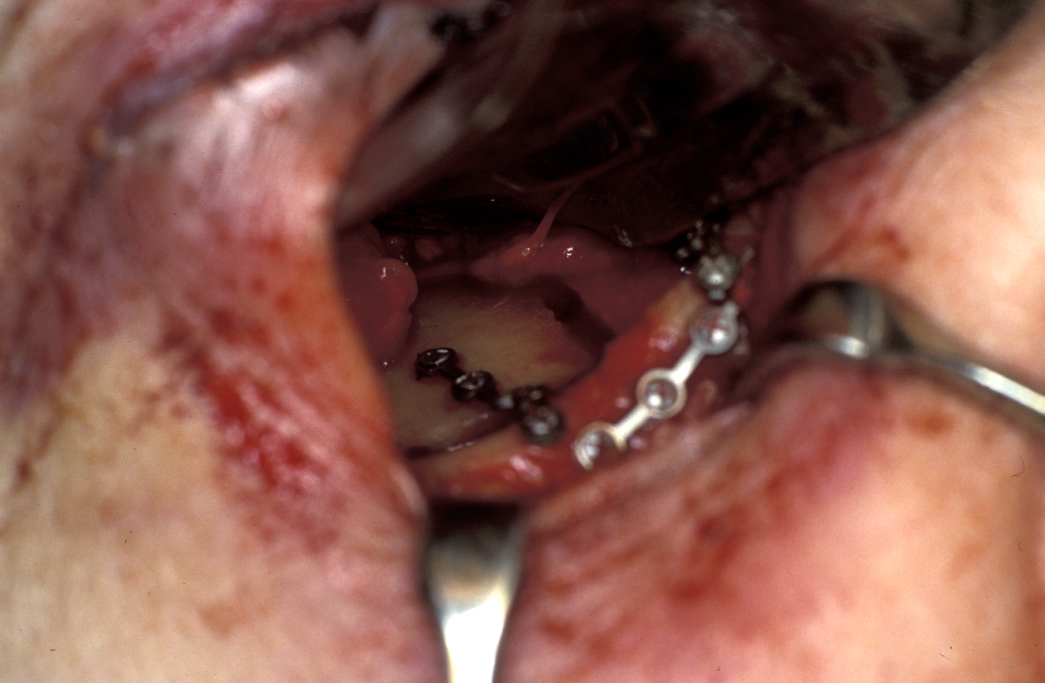
Definitive surgery usually involves open reduction and internal fixation (ORIF) under general anaesthesia, ideally using nasoendotracheal intubation. This allows the patient’s mouth to be closed and the teeth to be manipulated into their normal occlusion. This manipulation helps reduce the mandible into the prefracture bone position. Temporary intermaxillary fixation (IMF) is applied using a variety of techniques (trainee’s hand, eyelets, transalveolar screws (see Figure 1 and Figure 2), ‘rapid IMF’, arch bars). This helps to hold the fracture in its reduced position. Placing a bridle wire or tension band around the teeth can help reduce and temporarily fix the fracture.


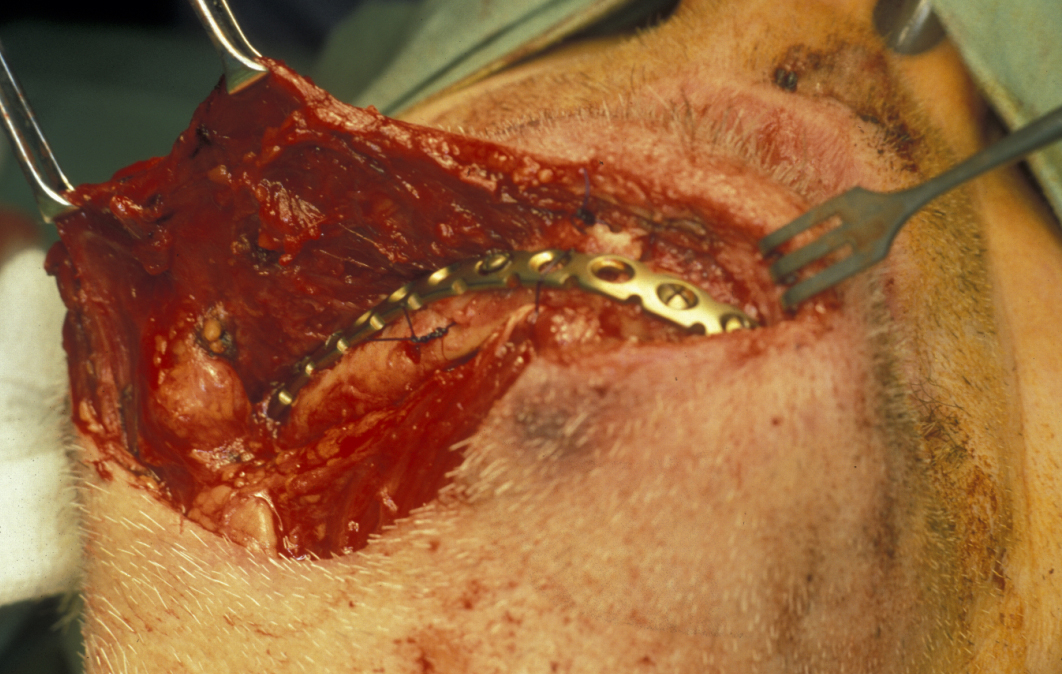
Under direct vision via buccal sulcus incisions (incision in the depression between cheek and arch of jaw) the mandibular fracture is exposed and reduction confirmed (see Figure 3).
Fixation is undertaken with titanium mandibular plates. According to Champy’s principles, in the mandibular symphyseal and parasymphyseal (the middle region of the mandible) region two mandibular plates are required, one just below the level of incisor/premolar apices and above the mental foramen and one as low down on the buccal surface as possible parallel to the lower border of the mandible. This is shown in Figure 4.

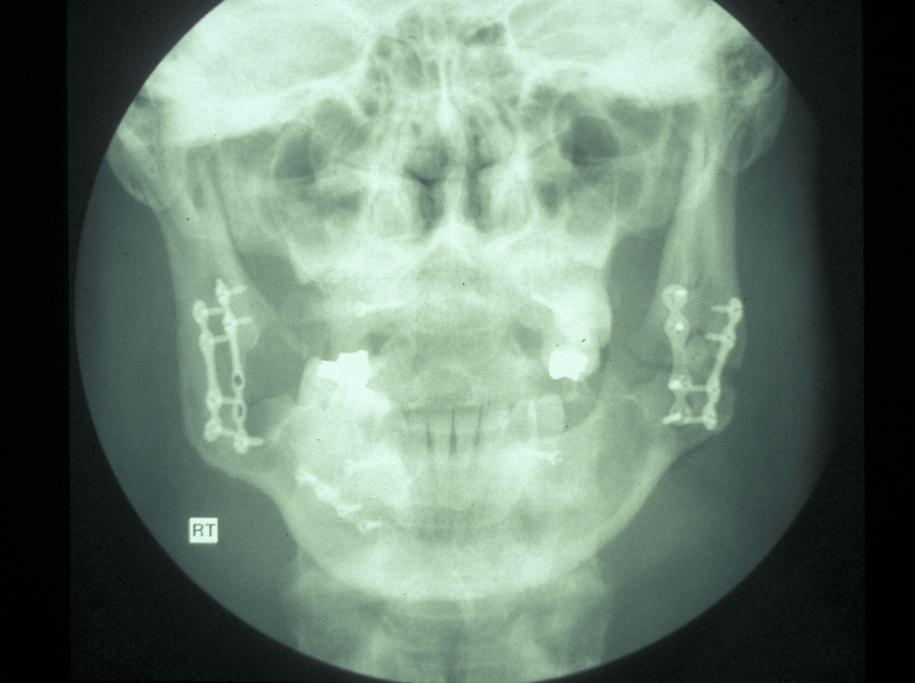
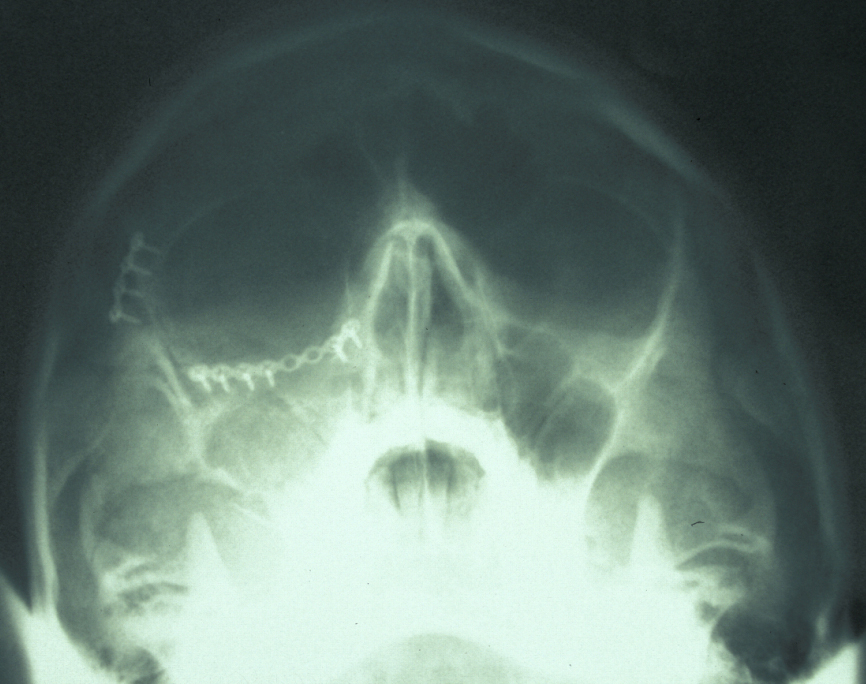
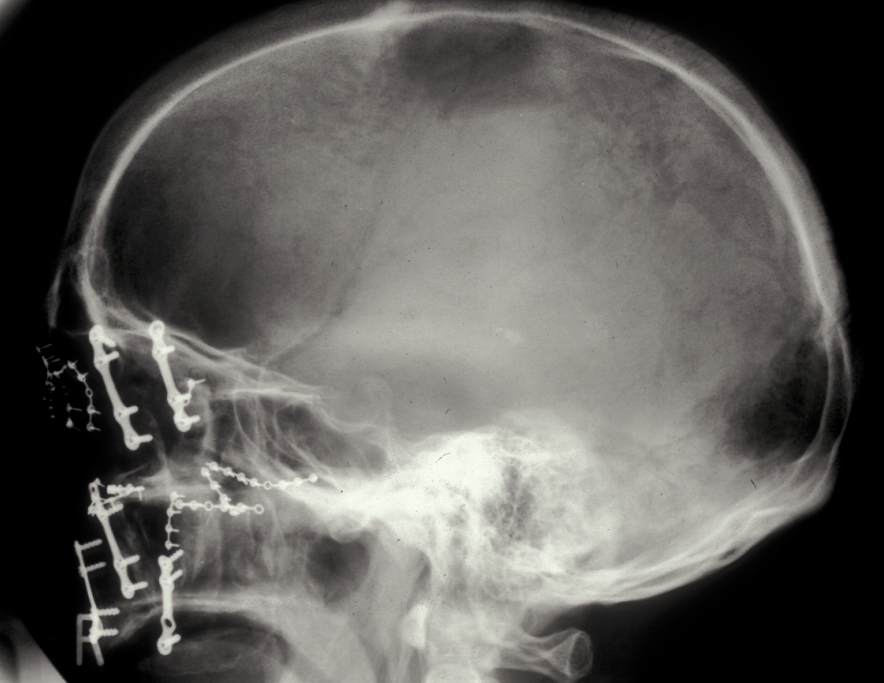
In the region of the angle of the mandible, a single plate is adequate to allow healing. In practice many surgeons now supplement this (or even replace it) with a transbuccally placed lateral plate which prevents lateral displacement of the lower border of the mandible. All these techniques use monocortically placed matching titanium screws to retain the plates which immobilise the fracture sites. Long-acting local anaesthetic regional block provides good postoperative analgesia and prophylactic broad-spectrum antibiotics are given preoperatively. Intraoral wounds are closed with resorbable sutures. If the occlusion is fully restored and stability of the fracture is assured by the plates, the intermaxillary fixation can be removed. Postoperative radiographs are taken to ensure correct placement of plates and screws and accurate realignment of mandibular fragments. It is also important to reassess the position of the condyles following ORIF as malpositioning can lead to TMJ problems later on (see Figure 5).
Mandibular fractures in children: fractures in children up to six years of age normally receive conservative treatment. An indication for osteosynthesis (reduction and fixation of a fracture) may be a simple or multiple fracture with displacement, especially when the possibilities of conservation fixation are limited.
In such cases two aspects that may be taken into account include, first, that a single 1.5 mm microplate is normally sufficient for the stabilization of the fracture, and second, because of the position of the teeth germs, the microplate should always be placed at the lower border of the buccal side. Fractures of the jaw in children 6 to13 years old require attention to the tooth germs.
Mandibular fractures in elderly patients: atrophic ‘pencil thin’ or ‘pipe stem’ mandibular fractures are common in elderly edentulous (toothless) patients and can be devastating to the elderly patient (see Figure 6).
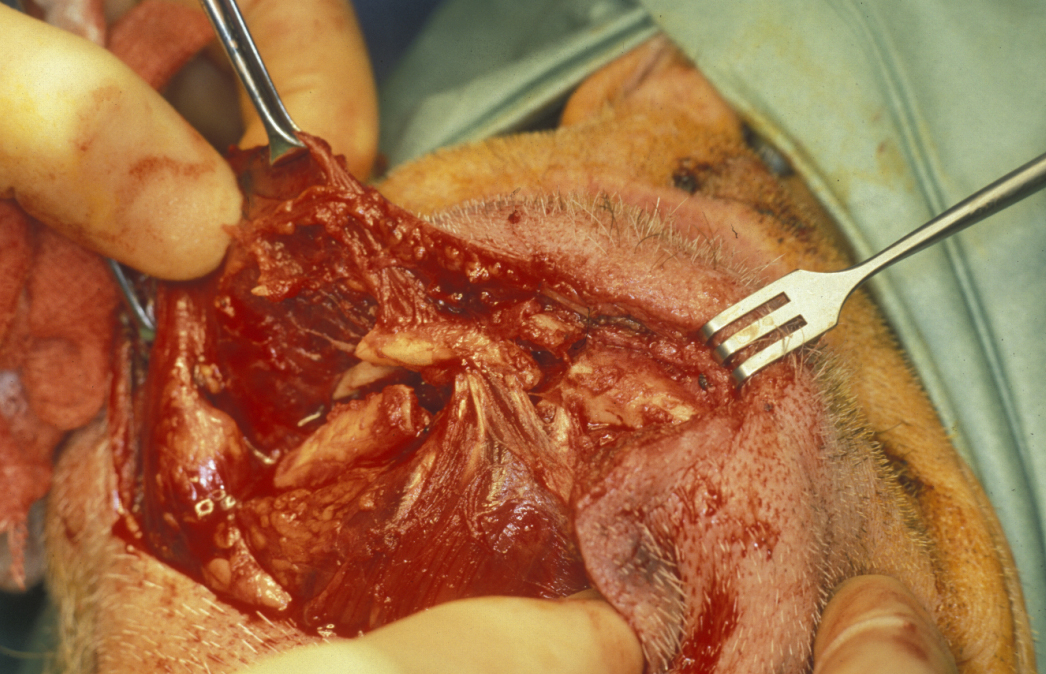
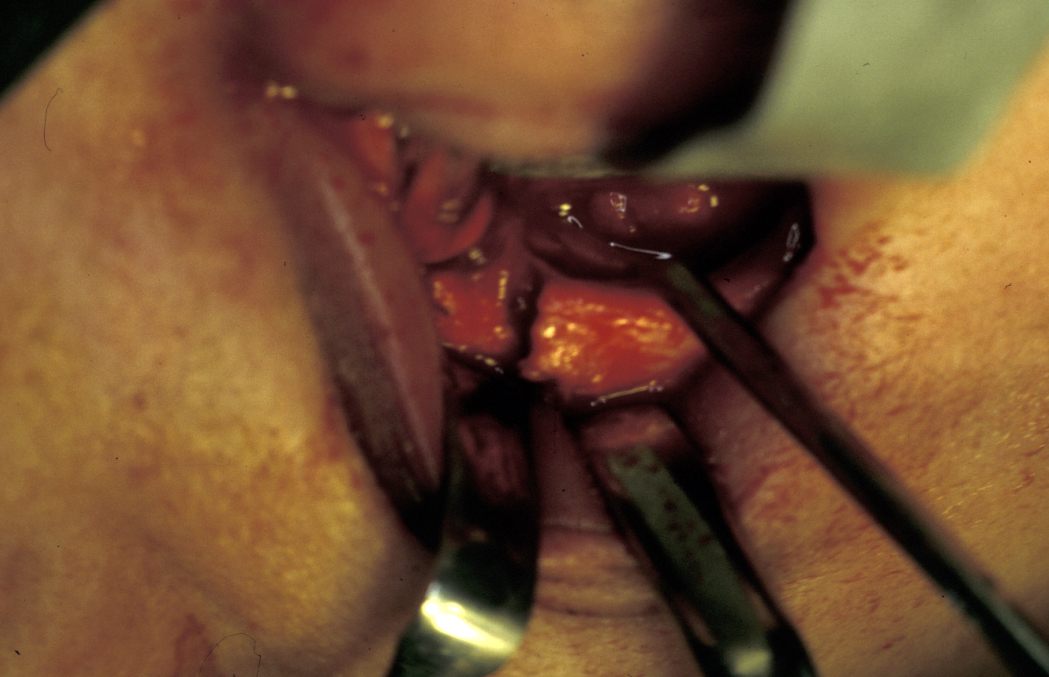
Malunion and even non-union are common and eating and nutrition deteriorate rapidly. Fracture repair is best done by keeping the maximum possible amount of periosteum intact and plating via an extraoral approach using a more rigid plate with bicortical screws that confer far greater rigidity and stability to the fracture site (see Figure 7 and Figure 8). This approach carries a greater risk of damage to the inferior alveolar neurovascular bundle but is balanced by the far higher success rate compared with conservative or monocortical plating techniques.
There are unfavourable conditions for healing in fractures of the atrophic edentulous mandible, such as a reduced cross-section and smaller contact area of the fractured ends as well as usually dense and sclerotic bone that is poorly vascularised.
However, because in extremely atrophic mandibles the subperiosteal plexus is probably the major blood supply to the bone, a supraperiostal dissection has been suggested and a supraperiosteal placement of plates and screws were recommended in the literature (personal experience with this technique showed it to be totally unhelpful as soft tissue ingrowth from the periosteum (membrane surrounding bone) loosened the screws far too early).
The advantage of rigid fixation is that it makes any postoperative maxillomandibular immobilization unnecessary. It allows free movement of the mandible, normal speech, and immediate uptake of a soft, solid diet and thus provides greater comfort for the patient.
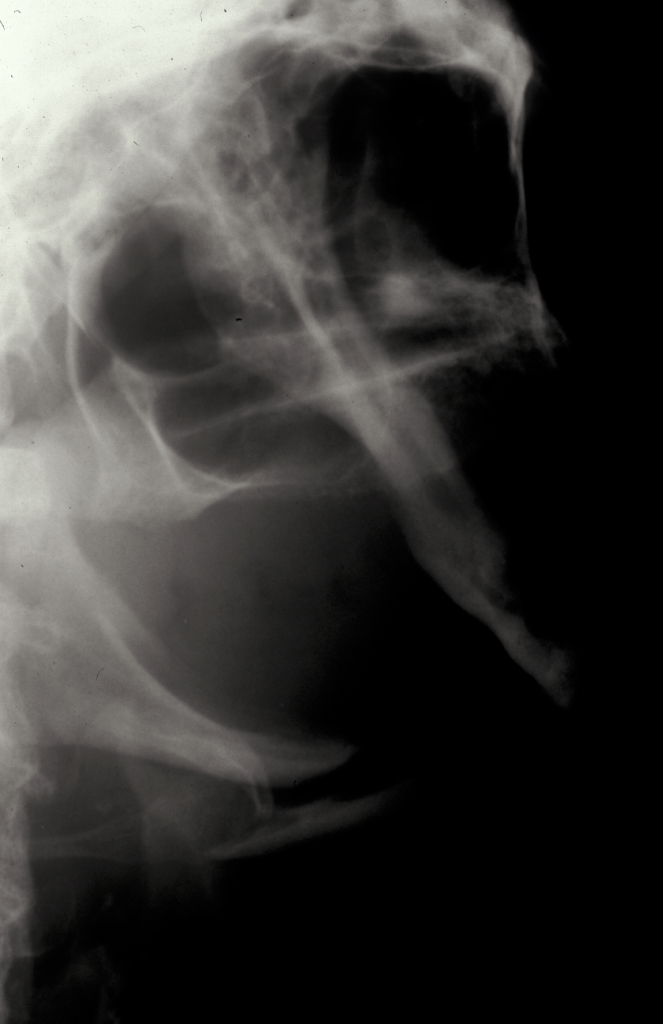
Condylar fractures: these are the most common mandibular fractures. They are treated conservatively in children up to 12 years with soft diet, analgesia and function. Young adults (12-18) are also treated conservatively in the majority of cases. Adults (>18) are treated with 7-10 days of heavy elastic IMF (fixation) and the occlusion reassessed. If malocclusion persists then ORIF of the condyle is undertaken. Overlap of fragments greater than 5 mm and angulation greater than 37°are postulated to warrant ORIF. Logically the function rather than the radiographic appearance should predicate the decision to undertake ORIF (see Figure 9 and Figure 10 for illustration).


A trend is emerging in the surgical literature confirming superior functional results following ORIF of condylar fractures, where this is indicated. This is supported by existing evidence. Endoscopic assistance, performed transorally, may also provide an alternative means for treating a subset of these injuries, reducing visible scar formation and possibly facial nerve damage.
There are still areas of condylar trauma surgery which some surgeons consider controversial: condylar head fractures and displaced paediatric fractures. The use of resorbable osteosynthesis techniques may be of benefit in both these clinical settings. Promising outcomes have been anecdotally reported following fixation of such fractures in children as young as 6 years of age. This finding is contrary to most accepted guidance which recognizes extensive condylar remodelling in children less than 12 years old.
Indications for ORIF of mandibular condyle fractures are either absolute (and applicable to children as well) and include displacement into the middle cranial fossa, impossibility of obtaining adequate occlusion by closed reduction, lateral extracapsular displacement of the condyle and invasion by a foreign body (for example, a gunshot wound). Relative indications apply to adults with condyles displaced out of the fossa and associated malocclusion and include: bilateral condylar fractures in an edentulous patient when a splint is unavailable or when splinting is impossible because of alveolar ridge atrophy; unilateral or bilateral condylar fractures when splinting is not recommended for medical reasons (such as seizures, psychiatric problems); bilateral condylar fractures associated with comminuted midfacial fractures; bilateral condylar fractures and associated gnathologic problems e.g. retrognathia or prognathism, open bite with periodontal problems or lack of posterior support.
While condylar open reduction and fixation is heavily endorsed by some, it is worth looking carefully at the published examples – all too often cases are shown which are relatively easy to access and fix whereas others are quietly left as ‘technically not feasible’. The old adage ‘the ability to do an operation is not an indication’ is worth keeping in mind in this area of facial traumatology.
Open treatment of mandibular condyle fractures (retromandibular approach traversing the parotid capsule) is associated with morbidity; complications from open treatment include haemorrhage, infection, weakness of the facial nerve, auriculotemporal nerve dysfunction (affecting the mandibular joint and ear), Frey’s syndrome (abnormal sweating of the cheek) and unsightly scars.
Comparing open and closed treatment of mandibular condyle fractures indicates less pain with open treatment. Both treatment options for condylar fractures of the mandible yielded acceptable results. But operative treatment, irrespective of the method of internal fixation used, was superior in all objective and subjective functional parameters.
Indicators of favourable outcome
- Restoration of the pre-traumatic mandibular appearance
- Restoration of pre-traumatic occlusion
- Normal function and mastication (chewing)
- Normal mandibular movement
- Normal speech
- Absence of chronic infection
- Absence of pain and iatrogenic (caused by treatment) nerve injury
Indicators of unfavourable outcome
- Failure to restore pre-traumatic appearance
- Failure to restore pre-traumatic occlusion
- Difficulty with mastication and speech
- Limited mandibular movements
- Mandibular malunion / non-union
- Chronic infection
- Chronic pain
- Failure of recovery of sensory dysaesthesias
- Iatrogenic damage to trigeminal nerve (5th cranial nerve, 3rd division mental / inferior dental nerve)
- Creation of iatrogenic motor nerve injury (facial nerve) during extraoral incisions
- Unacceptable facial scarring
- Dental trauma and other pathology not identified preoperatively
- Infected plates
- Iatrogenic injury to tooth roots by screw placement
Treatment of zygomatic complex (cheekbone) fractures
Treatment aims
- Restoration of facial appearance
- Restoration of orbital volume, globe position and prevention of enophthalmus (posterior displacement of the eye)
- Repair of orbital floor fractures with reduction of herniated orbital contents and release of trapped inferior rectus muscle (muscle for eye movement)
- Decompression of infraorbital nerve, promoting recovery of sensation
- Restoration of full range of mandibular movements
- Restoration of a normal occlusion by reduction of zygomatic and tuberosity displacement
Treatment planning
Surgery is ideally carried out after most of the swelling has resolved, around 7 to 10 days after injury. Earlier surgery in the presence of oedema tends to create a higher risk of poor scarring, difficulty in access and ectropion (drooping lower eyelid). General anaesthesia with oral intubation is usual (small risk of a significant bleed after some zygomatic fracture reductions, so a cuffed tube rather than a laryngeal mask is preferable). The aim of surgery is to reduce the fracture in order to restore the bone to its normal position. The bones are then fixed so that they heal in this position (Open Reduction Internal Fixation, ORIF). Occasionally the fracture locks into a stable position after reduction and no fixation is required. The time between injury and operation should be used to obtain all necessary information and act on it (Hess charts (eye examination), CT scans and so forth).
Preoperative consent
There is possible scarring from plate insertion and orbital floor repair, and eyelid scarring. Chemosis (gross swelling of the conjunctiva) is common after transconjunctival incisions if that incision is used in accessing the infraorbital rim and floor. There is a risk of developing a retrobulbar haemorrhage after surgery (which would necessitate further, emergency, surgery).
Zygomatic fracture repair
Incisions to gain access to the fractures and place plates to stabilise the fracture after reduction include a temporal Gillies incision (see Figure 11),

upper lateral blepharoplasty (eyelid) incision, crows foot incision (along eyebrow), lateral brow incision, infraorbital incision (see Figure 12),
transconjunctival incision, subcilliary (eyelid) incision and intraoral buttress incision.
Zygomatic fractures including zygomatic arch fractures are reduced by inserting a hook under the body of the zygoma caudally (to the back) in a vertical line from the lateral canthus (angle between upper and lower eyelid). The hook is named after Stromeyer. Interestingly these surgical variants can be seen from unit to unit in the UK and internationally.
Reduction of a zygomatic fracture can be carried out in three ways:
- Temporal approach - the incision is made in the hairline two fingerbreadths above the tip of the pinna (outer part of the ear). Skin, temporoparietal fascia and temporalis fascia are dissected while trying to avoid superficial temporal vessels (but ligation of these, if it happens, is not a disaster). An elevator is inserted just deep to the temporal fascia. It is passed along the lateral surface of the temporalis muscle and enters the natural space beneath the zygomatic arch deep to the zygoma.
- Percutaneous approach - a small stab incision in the cheek allows access for a bone hook to carry out the reduction.
- Intraoral approach (Keen is the eponym in US) - an incision is made in the upper buccal sulcus (depression between cheeks and arch) to expose the fracture at the buttress (see Figure 13).
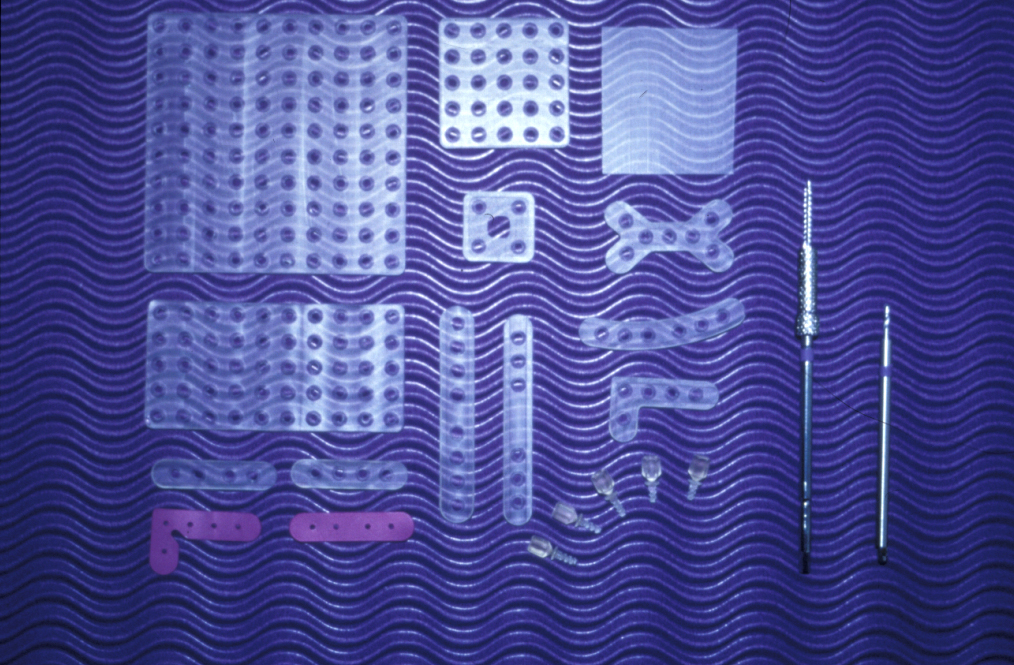
The direction of reduction (elevation) is to reverse the direction of the movement of the zygoma due to the impact. This is generally in an upward and outward direction opposite to that causing the fracture in the first instance. The aim of reduction is to restore the bone fragments to their symmetrical pre-injury position. This is assessed by visual inspection after satisfactory elevation, unless the fracture lines are being directly exposed and visualised. Elevation is generally easily achieved during the first fourteen days after injury. After this time the fracture has started to heal in its incorrect position and elevation can be more difficult. Simple fracture patterns may allow the fracture to be reduced into a stable position and require no formal fixation. If the fracture falls back into an abnormal position after gentle palpation it is considered unstable and requires fixation. Fixation is in the form of low profile titanium or resorbable plates (usually 1.0mm, 1.3mm or 1.5mm thick, but this is changing as technology improves) placed across one or more of the fracture sites (frontozygomatic, infraorbital or buttress). Titanium has been the material of choice since 2000. Resorbable plates and screws have more recently become available but have not yet displaced titanium as the material of choice (see Figure 14).
Small, asymptomatic orbital floor defects require no treatment. If the patient has persistent diplopia (double vision), enophthalmos (displacement of the eyeball), or significant herniation of orbital contents into the antrum, repair is indicated. A bone graft from the outer table of skull (see Figure 15) or anterior wall of
maxilla, artificial resorbable material, titanium mesh, preformed titanium plates, Gore-Tex sheet, lyophilised dura and cartilage have all been used. The repair allows orbital volume to be maintained and encourages bony healing to restore the orbital defect. Care must be taken to ensure that none of the extraocular muscles become trapped in the fracture or under the repair, as this would cause even worse diplopia. The forced duction test is classically described as the test for ensuring this has not happened. The surgeon rotates the eye upwards by pulling on the inferior rectus muscle to ensure that there is no limitation of passive eye movement.
The patient is advised not to blow their nose for a period of two to three weeks postoperatively. This reduces the risk of surgical emphysema forming in the soft tissues of the periorbital and zygomatic region. This is helped by using nasal decongestants for the first postoperative week.
Postoperative care
Antibiotics are given intravenously during surgery and for two postoperative doses if plates are used. Radiographs are taken to confirm good reduction of the fractures and satisfactory plate and screw positioning, although published audit would suggest that these films rarely influence treatment. Topical chloramphenicol ointment is applied to skin and conjunctival wounds to promote healing and make suture removal easier. If necessary, eye exercises are prescribed to encourage mobility of the globe. Sutures are removed after five days.
Indicators of favourable outcome
Restoration of facial appearance, restoration of eye position and function, recovery of infraorbital nerve function, minimal scarring, no pain or infection associated with plates (see Figure 16).
Indicators of unfavourable outcome
- Abnormal facial appearance
- Lack of symmetry
- Eye problems, persistent double vision
- Heavy scarring, eyelid scarring
- Temporal hollowing from temporalis muscle atrophy
- Persistent numbness
- Infected plates or chronic pain in plates
- Migration of orbital floor repair material
Post-Traumatic Orbital Reconstruction – Anatomy
- ‘Safe distances’ (those distances within which it is considered safe to dissect within the orbit) have been derived from measurements made from intact orbital rims in dried adult skulls and are of limited value in cases of severe orbital disruption.
- In high-energy injuries, the subperiosteal plane can be difficult to identify or be completely absent because of the extent of disruption of the orbit. The plane is often absent in old injuries, where the surgeon may be attempting to correct post-traumatic enophthalmos.
- Despite the accuracy of modern imaging, the size of the defect on CT is often smaller than the size of the defect encountered at the time of operation.
- The anatomical landmarks of the deep orbit are both hard and soft tissue structures:
- Infra-orbital nerve
- The inferior orbital fissure
- The greater wing of the sphenoid
- The orbital plate of the palatine bone.
Blow-out fractures of the orbital floor are rare in children under five. The very young are more likely to have a fracture of the roof. The investigation of choice is a CT scan. Approaches to the facial skeleton may include the subtarsal (lower eyelid) approach that gives good access for reconstruction of the medial canthal ligament (connects eyelids to the skull) and is less likely to damage the lacrimal system. Fractures of the roof and supraorbital rim are approached through a coronal flap (incision to the scalp, leaving no visible facial scars). Access to the frontozygomatic suture in this series is via a horizontal upper lid blepharoplasty.
Management of orbital blow-out fractures in children: fractures of the orbital floor are rare in children under 8 years old. It is more likely that these fractures would involve the anterior orbital floor and be associated with diplopia. Classic presentation of an orbital blow-out fracture in a child is with no subconjunctival haemorrhage, a ‘white eye blow out fracture’ with upgaze diplopia and general malaise caused by the oculovagal reflex (caused by pressure or traction on the eyeball, see below). There is marked restriction of motility in upward and downward gazes and may be little evidence of disruption to the orbital floor on CT scans, possibly only a small crack or trapdoor defects with little bony displacement. The greenstick trapdoor of bone in the orbital floor or medial wall in children tends to spring back after fracture and trap inferior orbital soft tissues, typically the inferior rectus muscle. If not released quickly, it may cause a permanent ischaemic necrosis and potentially a Volkmann ischaemic contracture and permanent impairment.
The oculovagal reflex presents with bradycardia (slow heart rate) associated with traction on the extraocular muscles or compression of globe (atropine may be necessary). Refractory vomiting is also a feature of the reflex in children and this may be uncontrollable until the child is anaesthetized. It is worth noting that a less severe set of symptoms can be seen in adults with posterior but otherwise similar white eye blow-out fractures.
Treatment of nasal fractures
Aims of treatment
- To restore normal anatomy and function
- To correct associated orbital/cranial/ethmoidal (bone at root of nose) deformity
Initial treatment
A septal haematoma must be evacuated by needle aspiration or incision as soon as possible after it is identified to prevent septal ischaemia and necrosis.
Plane 1 and 2 injuries
These are injuries that lie anterior to a line joining the nasal bones and the anterior nasal spine and are confined to the cartilaginous nasal skeleton (plane 1) or injuries that are limited to the external nose, not involving the orbital rims (plane 2). These fractures are treated by closed manipulation under local or general anaesthesia to reduce the deformity (see Figure 17 and Figure 18). Nasal packs and an external splint are then placed to hold the nose in position.


A long-standing deformity may require a submucous resection or septoplasty (both operations to straighten a deviated septum). Complex residual deformity may require post-traumatic rhinoplasty (procedure to restore form and function of the nose).
Plane 3 injuries
These are fractures (nasoethmoid and nasoorbital fractures) that involve the orbital walls and anterior cranium. Fractures involving the nasoethmoidal and nasoorbital complex are more demanding. Fractures here can lead to loss of nasal projection, widening of the intercanthal distance (distance between the eyes), unsightly appearance of the nasal bridge, and considerable breathing difficulties. If the intercanthal distance is greater than 40mm, open reduction and internal fixation of the nasoethmoidal complex is required to reattach the medial canthal ligament. This usually means fixing the bony attachment of the medial canthus rather than the canthus itself, although a specific piece of fixation apparatus is available to fix the ligament in rare instances.
Access for this operation is by coronal incision to avoid scarring in the forehead region or local lacerations or scars. The bones are then elevated with intranasal forceps and fixed in place with microplates. Reconstruction of the nasal bridge with an autogenous bone graft may be required. Profuse bleeding can occur perioperatively but is controlled by anterior nasal packs placed at the end of the procedure.
Indicators of favourable outcome
Haemostasis, normal nasal anatomy, acceptable aesthetics, good nasal air entry.
Indicators of unfavourable outcome
Failure to control haemorrhage, nasal deformity, nasal obstruction, patient dissatisfaction.
Treatment of midface fractures
Treatment aims
- Restoration of facial appearance and occlusion
- Stabilisation of fractures to allow healing.
- Reduction of any fractures of the palate
- Prevention of oronasal fistula formation
Preoperative consent
Facial scarring is possible, possible IMF application (fixation screws for immobilization), a temporary tracheostomy and/or nasal packs may be necessary.
Midface fracture repair
Simple undisplaced fractures can be treated conservatively as long as there is no derangement of the occlusion or alteration of the facial profile. Complex displaced fractures with significant facial and occlusal change require open reduction and internal fixation of fracture fragments. All fracture repairs are carried out under general anaesthesia with nasal intubation ideally. If this is not possible, a temporary tracheostomy or a guarded flexible orotracheal tube is used.
The first manoeuvres during fracture repair are disimpaction and restoration of the fracture fragments to their premorbid position. Le Fort I fractures are treated by simply disimpacting the fracture and then closing the patient into their normal occlusion. Once the occlusion has been restored, temporary IMF (fixation) is applied. An incision in the maxillary buccal mucosa allows access to the buttresses and pyriform aperture (pear-shaped opening in the skull). The fracture is then exposed and mini plates placed. Two plates are normally placed on each side to stabilise the fracture; an example is shown in Figure 19.
The Le Fort II fracture requires buccal sulcus incisions and infraorbital incisions and fixation at the level of the infraorbital margin as well as the buttress region.
The Le Fort III fracture involves frontozygomatic repair, frontonasal fracture repair and zygomatic arch repair. The latter fracture repair is best approached through a coronal incision, which gives good access to the zygomatic arch. It is imperative that the arch is returned to its pretrauma position, as this determines the anteroposterior projection of the face and prevents any postoperative facial deformity. The zygomatic arch tends to ‘telescope’ under the force of the initial impact, thus shortening the anteroposterior facial dimension.
Special Situations: Le Fort II and III fractures often involve disruption of the orbit and orbital floor, medial and lateral wall repair is an integral part of the operation.
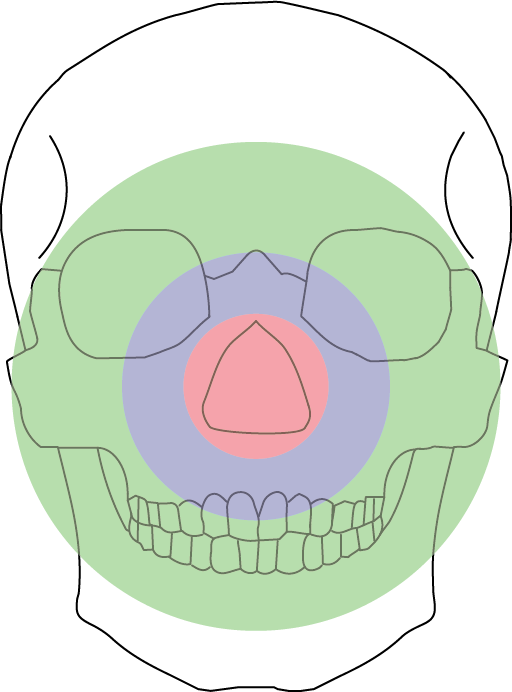
If midface fractures occur in conjunction with complex mandibular fractures and condylar fractures, it is imperative that a logical sequence of repair is taken. Mandibular condylar height must be restored to ensure the overall posterior facial height does not change. Once the condyle is repaired, the frontozygomatic suture and zygomatic arch can be repaired, thus setting the outer facial frame. The next fracture to approach is the lateral orbital wall, maxillary buttress and finally inner circle of medial orbital wall and piriform fossa. Adhering to this sequence of repair allows achieved logical sequence, rational stepwise reduction of the fractures and optimises the chances for a return to premorbid position; see Figure 20 for illustration.
Postoperative care
Postoperative analgesia, antibiotics and meticulous oral hygiene are required. Condylar height and midfacial position should be confirmed on postoperative radiographs. Skin sutures should be removed at five days, removal of coronal flap staples at seven days. Temporary IMF with elastic bands should be placed to reinforce the occlusal position for at least seven days. Soft diet is recommended to ensure the plates and the reduced fractures do not move. Contact sports should be avoided for approximately three months postoperatively.
Indicators of favourable outcome
Restoration of occlusion, restoration of facial appearance, restoration of eye function, good healing without infection, absence of palatal fistulae.
Indicators of unfavourable outcome
Deranged occlusion, flattened (‘dish face’) appearance, lack of nasal projection, persistent diplopia, shortened face, infection of plates, exposed palatal bone and development of an oro-nasal fistula, hypertelorism (wide eye separation).
Treatment of frontal sinus fractures
Treatment aims
- Restoration of forehead continuity and prevention of long-term deformity
- Surgical access to assess and repair any dural tear, to prevent long term risk of intracranial complications.
- Access to the frontal sinus so that sinus obliteration can be carried out and deliberate blockage of the nasofrontal duct communication can be undertaken. This prevents long term frontal mucocoele (cyst) and reduces the risk of cerebrospinal fluid (CSF) leak through the nasal roof.
- If process 3 is not part of the overall treatment plan, for example when the posterior wall is intact and there is little evidence of frontal sinus lining damage and dysfunction, the essential step is to maintain ventilation of the sinus by a patent nasofrontal duct. This may require intervention ranging from minimal (inhaled nasal decongestants for a week) to maximal conservative intervention (functional endoscopic sinus surgery).
Preoperative consent
There will be a coronal incision and a small risk of alopecia (hair loss) and temporal hollowing (depression near the temple). The sense of smell may be further altered. Postoperative drains will be present.
Fracture repair
Access is via a coronal flap, which exposes the frontal bone, orbital roof, medial orbital wall, and nasal bones. If the frontal bone is minimally displaced it is reasonable to reposition the fragments and fixate by microplating. In the case of missing frontal bone the sinus can be directly examined for posterior wall fractures, CSF leak and mucosal damage. If the frontal bone fragments are displaced but not missing, it may be necessary to carry out a mini-craniotomy (removal of some bone from the skull) of the frontal bone overlying the frontal sinus in order to adequately examine the frontal sinus. If the mucosa is significantly damaged, one school of thought is that it should be completely excised, the frontonasal duct obliterated and the sinus obliterated by bone graft. If the posterior sinus wall is involved a popular neurosurgical technique is to remove the posterior wall, carry out dural repair and allow the brain to expand into the defect ‘cranialization’. The most important issue is whether the sinus is maintained, in which case it must have adequate ventilation via the frontonasal duct as described above.
CSF leaks are uncommon and usually resolve without surgical intervention. Confirmation requires testing for the presence of beta-2-transferrin because glucose levels and the ‘target sign’ or ‘ring test’ are not reliable. Antibiotics are not recommended, due to acquired resistance. Initially leaks are observed for 7-10 days, followed by CSF direction (lumbar drain) for 5-7 days. If repair is required, high-resolution CT scans or intrathecal injection (into the spinal canal) of fluorescein (contrast agent) are needed to identify the site of leakage.
Repair of the frontal bone defect can be achieved with inner table from the cranial vault, fracture fragments, outer table bone graft or free iliac bone. If there has been a substantial degree of bone loss, acrylic plates were popular as a custom made cover for the defect. Alternatively, titanium sheets can be used in the acute setting and cut to shape or fabricated based on CT scans. Several other cranioplasty materials have recently become available (for example, polyarylether-etherketone (PEEK)). Long term follow up involves monitoring for frontal mucocoele development, meningitis, frontal bone deformity, potential infection of the plates and CSF leak.
Indicators of favourable outcome
Restoration of anatomy, airway, lacrimal function, eye function, no meningitis.
Indicators of unfavourable outcome
Facial deformity, telecanthus, eye problems, retention cyst (mucocoele), meningitis, loss of sense of smell (anosmia).