Broken bone
Fracture
Contents
In this section we revisit the different locations of fractures. We give an account of signs & symptoms associated with the different fractures, alongside a description of the most common methods to investigate these injuries.
Mandibular fractures
The mandible is a rigid horseshoe of bone with a modified hinge joint at either end. It is much more sensitive to lateral than frontal impact (it takes around 190 kg frontal impact to consistently fracture condyles in cadavers).
Common fracture patterns are shown diagrammatically in Figure 1.
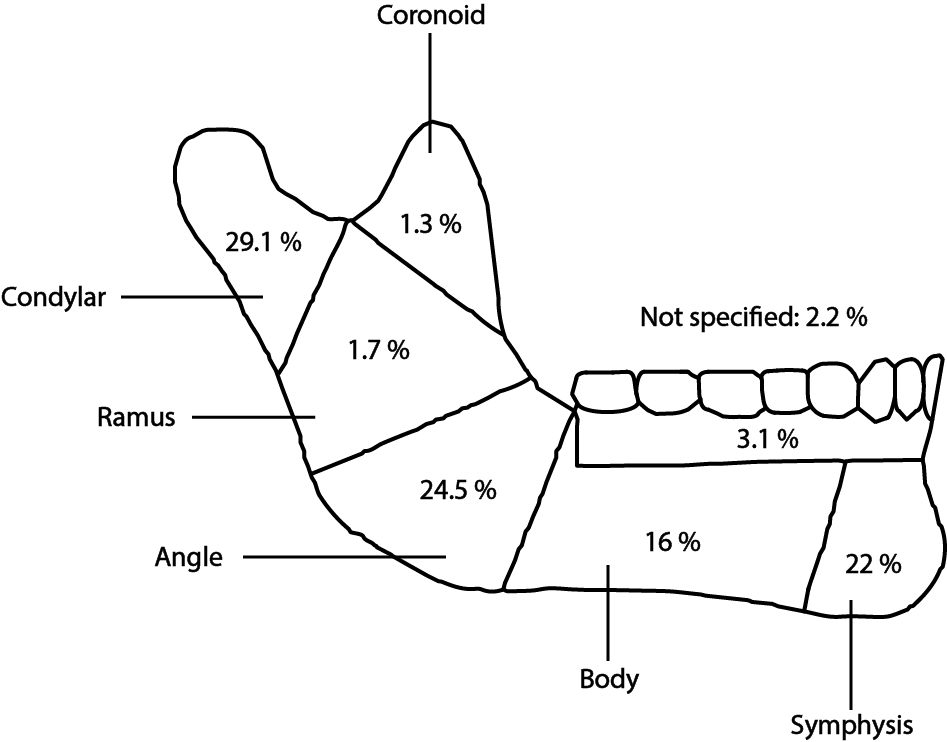
These percentages change with age, as do the specific types of fractures seen between paediatric and adult mandibles and dentate and edentulous mandibles.
Intracapsular fractures of the condyle are commoner in childhood due a short neck of the ramus, whereas condylar neck fractures are commoner in adults. Body fractures of the edentulous mandible are commoner than in the dentate mandible as the loss of bone height and density after tooth loss is greatest at that point.
The condyle is the commonest site of fracture of the mandible but the type varies with patient age. They can be intracapsular or extracapsular, displaced, undisplaced or dislocated.
Bilateral condylar fractures are classically seen in falls and road traffic collisions, in which a large frontal impact can occur. The classical ‘Guardsman's fracture’ involves fracture of bilateral mandibular condyles with or without symphyseal (chin region) fracture, caused by a fall or blow to the point of the chin (the term comes from UK royal palace guards fainting in the attention stance and landing on their chins).
The angle and the parasymphyseal (close to the chin) regions are commonly weakened by the presence of third molars in various stages of eruption and the canine teeth, respectively. These are the most common sites of fracture resulting from a lateral impact, more usually caused by a blow.
Combinations of fractures are possible and should be always looked for.
Symptoms
Symptoms may include pain in the lower jaw, abnormal bite, bleeding from the mouth, loose teeth, numb lip, pain in the temporomandibular joint region, limited mouth opening, swelling of the floor of mouth, and swelling of soft tissues around the mandible. Immobility of the mandible is usually in an effort to prevent pain, but can be caused by spasm of the muscles of mastication.
Signs
Clinical examination of a mandibular fracture may well show, depending on the level of fracture displacement and fracture pattern, no evidence of disruption of the mandibular body and essentially a normal occlusal contact pattern. These fractures represent undisplaced hairline fractures of the mandible and are confirmed by radiological investigation. Examination of a displaced mandibular fracture will show disruption of the occlusion and subtle or obviously mobile fragments. Sharp bony fragments or fractured teeth may be encountered during intraoral examination.
Lingual haematoma (bruising of the tongue) is swelling and bruising on the floor of the mouth adjacent to the fracture site. Fractures of the ascending ramus and condyle may present with no gross clinical signs. The external auditory canal needs to be examined for bleeding which may be from a base of skull fracture or, more commonly, condylar neck fracture connecting with the external ear canal.
Investigations
The combination of plain X-ray radiographs taken from different directions gives adequate diagnostic information for most mandibular fractures (DPT, dental panoramic tomogram (see Figure 2) and posteroanterior radiographs (see Figure 3)).
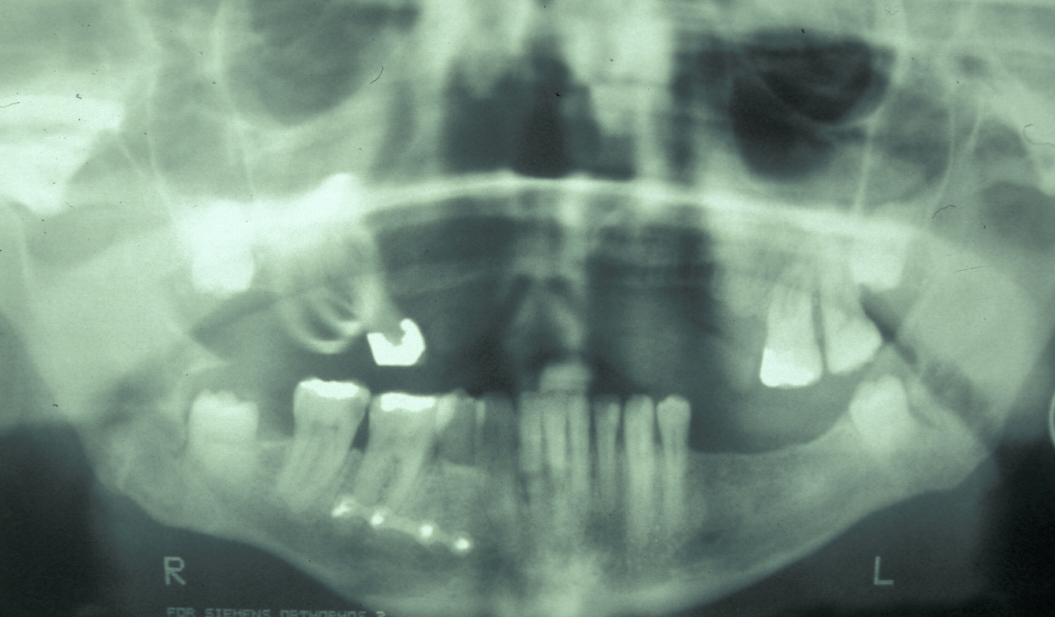

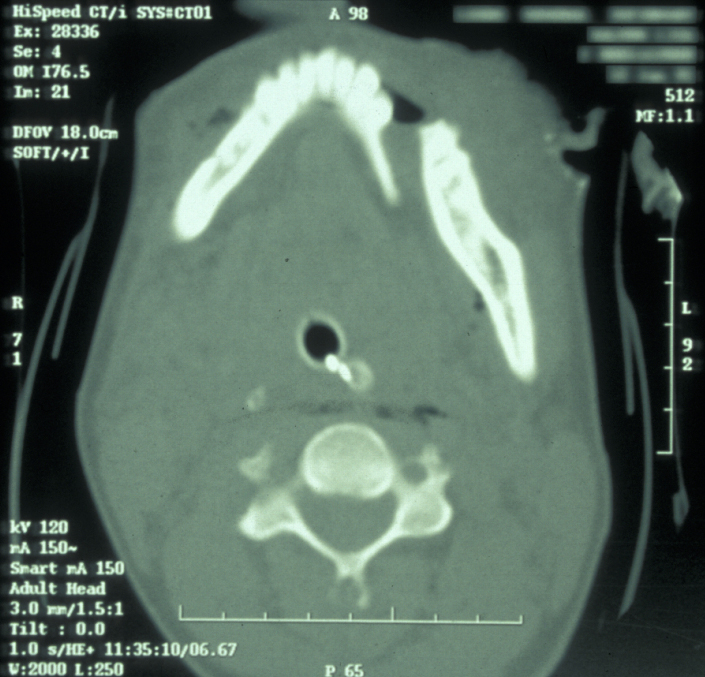
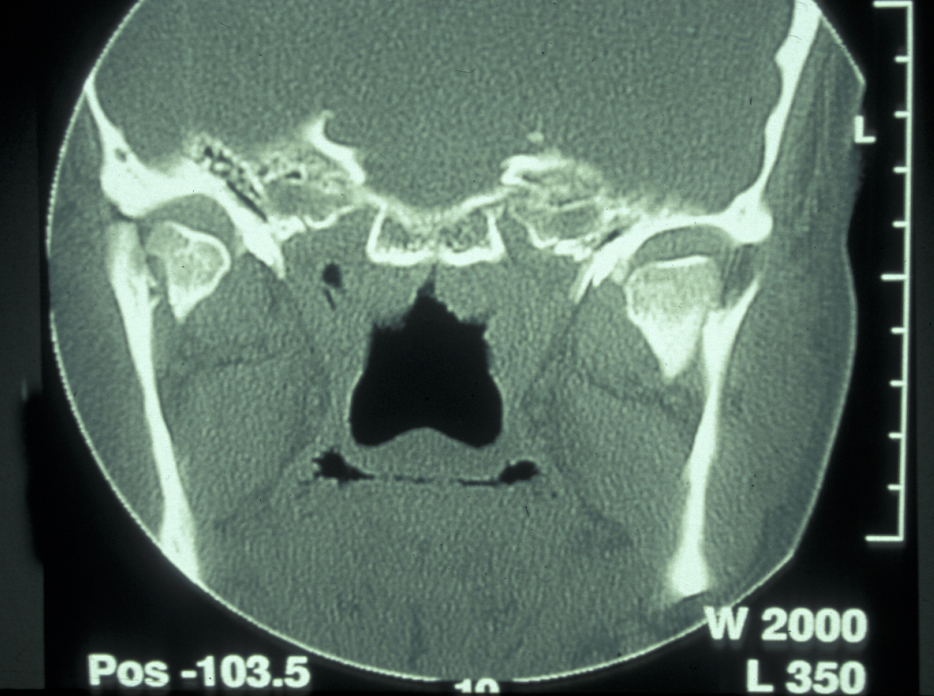
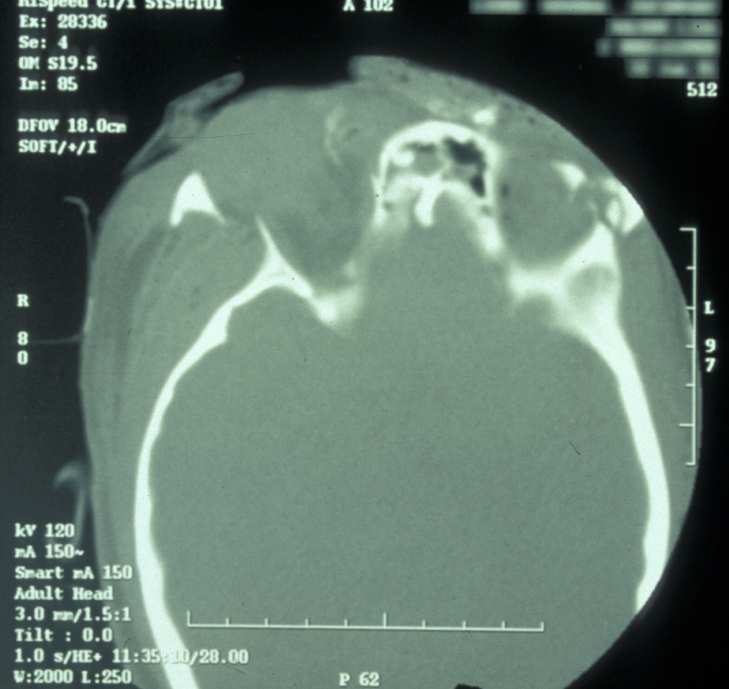
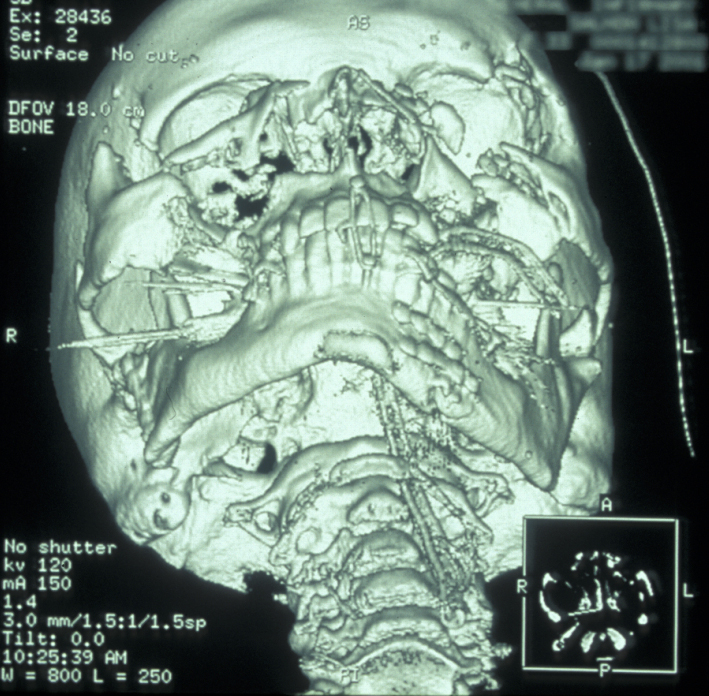
If the patient is unable to stand in the DPT machine, left and right lateral oblique mandibular views will give good imaging of the body of the mandible. If the patient has multiple complex maxillofacial fractures a CT scan (CT coronal and axial images, with or without 3D reformatting) is helpful (see Figure 4). The CT scan will help assess condylar fracture position, angulation and any fractured dislocation of the condylar head. A CT scan is also useful to image multi-part mandibular body fractures.
Zygomatic complex fractures
Many patterns of zygomatic complex fractures are possible. The classical 'Tripod' fracture involves fractures in the frontozygomatic region, infraorbital margin and zygomatic arch. Displacement can be marked in one direction, rotated or in a combination of movements. Comminuted fracture patterns pose a difficult reconstructive challenge and usually occur in high impact injuries such as road traffic collisions.
Symptoms
Numbness of the cheek and side of nose on the affected side are common. The teeth in the corresponding upper quadrant may also feel numb. There may be an altered bite (in extreme cases the maxilla is pushed down causing posterior premature contacts) or inability to open the mouth (caused by the zygomatic arch impacting on the coronoid process), a flattened cheekbone and in cases where the orbit is involved, double vision.
Zygomatic fractures with gross displacement can disrupt the orbital volume and eye suspensory ligaments leading to hypoglobus (lowered eye level) and enophthalmus (a sinking of the eyeball into the socket). Globe displacement and trapping or later fibrosis of the periorbital fat and muscle can also cause diplopia (double vision), usually on upward gaze.
Signs
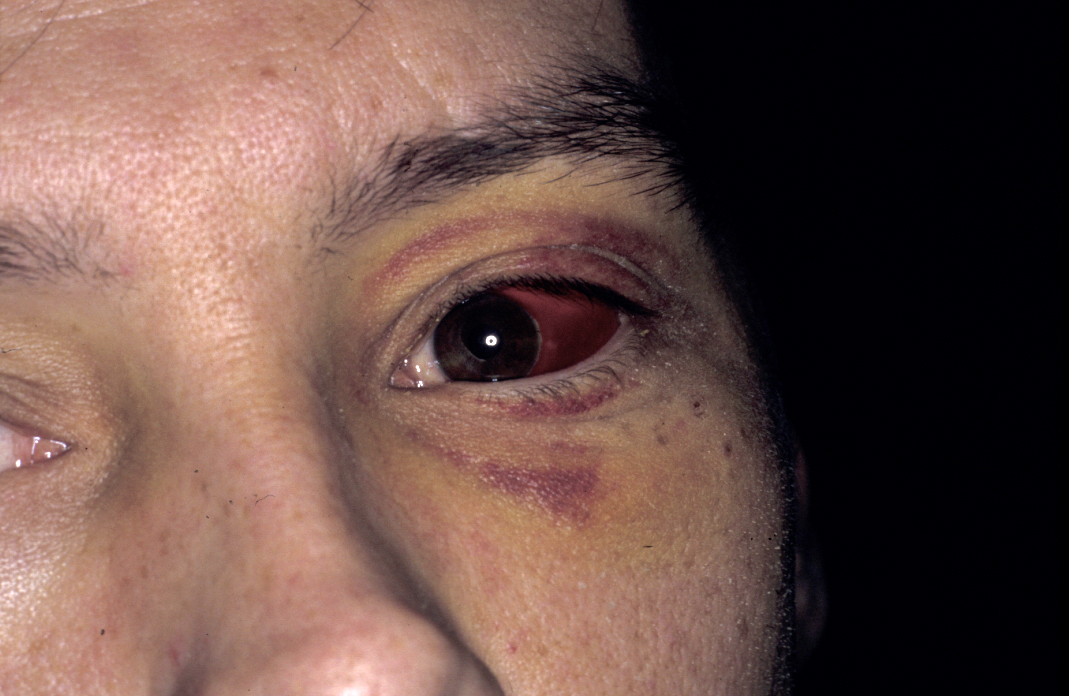
There is facial asymmetry, loss of cheek prominence and indentation of the zygomatic arch (dimpling over fracture) although these can be masked by swelling. Subconjunctival haemorrhage (see Figure 6) suggests direct trauma to the eye or fracture of the orbital walls or floor. A complete lateral subconjunctival haemorrhage usually indicates a zygomatic fracture. Medial subconjunctival haemorrhage implies naso-orbital fracture. Eye position needs to be examined from in front, below and above because otherwise subtle changes may not be seen if swelling is marked.
Palpation reveals facial asymmetry by comparing the normal and the injured side. Palpation of the infraorbital margin shows a palpable step and discontinuity of the bone. Palpation in the upper labial sulcus may reveal a fractured lateral maxillary wall, which feels boggy due to the presence of a haematoma. Sometimes a sharp laterally overlapping bone fragment is felt. Usually the fracture is impacted and therefore not mobile.
Testing sensation will reveal loss of nerve function in the distribution of the infraorbital nerve. Documentation of the extent of loss can be used to gauge nerve recovery in the months after trauma by repeat assessment.
Ocular involvement of zygomatico-orbital complex fractures: it is imperative that the visual acuity of the eye is fully assessed and recorded at initial presentation:
- Pupillary reaction, consensual reflex and accommodation.
- Visual acuity using a Snellen chart.
- Visual fields.
- Eye movements in an ‘H’ shape.
Any abnormality in acuity mandates discussion with an ophthalmologist (see Figure 7). Abnormalities of eye movement as seen in orbital blow out fractures necessitate formal assessment of ocular movement (Hess chart) by an orthoptist (specialist in eye movement disorders).

Retrobulbar haemorrhage (bleeding behind the eyeball) is a surgical emergency. The classic signs are pain, proptosis (protrusion of the eye), dilated pupil, ophthalmoplegia (weakened eye muscles) and decreasing visual acuity. Immediate surgical intervention to prevent permanent loss of visual acuity is necessary. The mechanism behind retrobulbar haemorrhage in orbital trauma is believed to be an arterial bleed rather than the venous bleed seen in retrobulbar blocks.
Orbital apex compression by oedema may respond to high dose steroids. Damage by fragments of bone is not reversible and the prognosis is poor.
Investigations
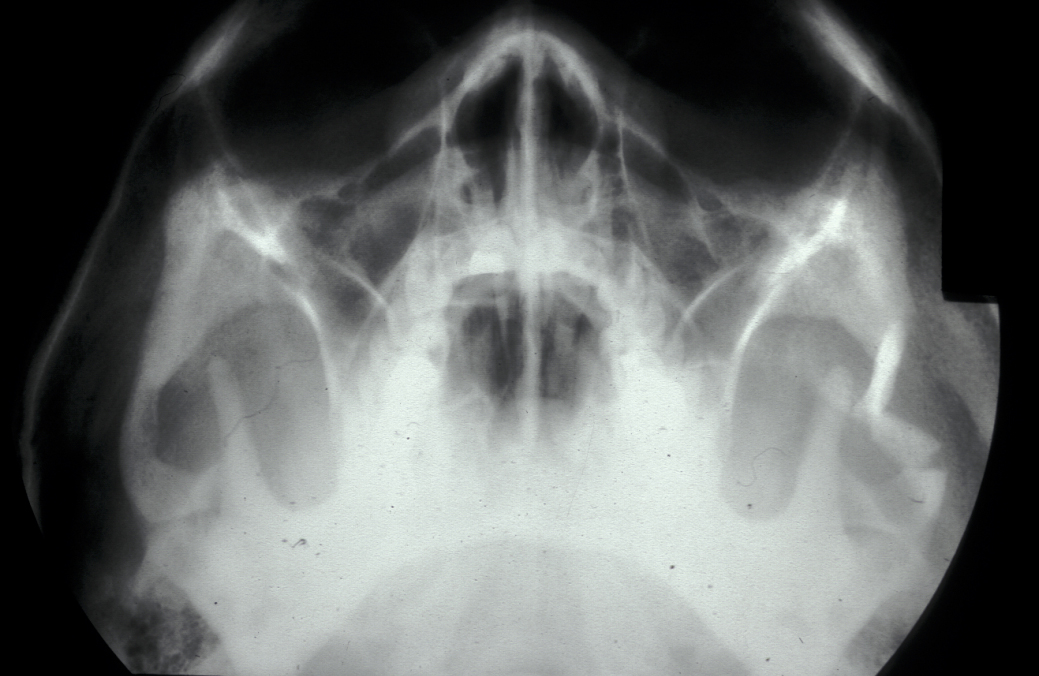
Plain film X-ray radiographs from different angles generally give sufficient diagnostic information. Combined they give good imaging of the zygomatic complex and can be used to determine the level of displacement and fracture pattern. Teardrop appearance into the maxillary antrum suggests an isolated orbital floor fracture (a 'blow out orbital fracture'; see Figure 8). Identification of this type of fracture mandates further investigation by a coronal (vertical plane view) CT scan and Hess chart test (eye test to assess motility of the eye).
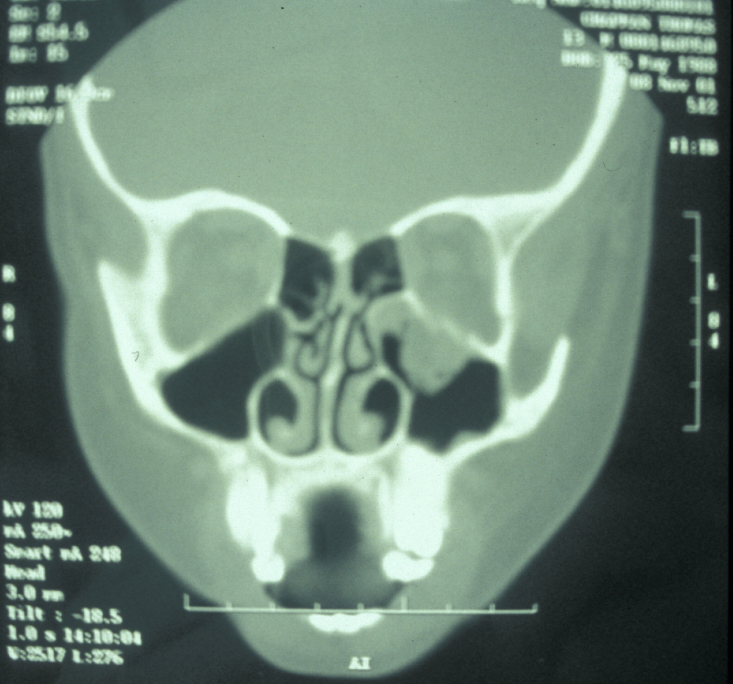
Isolated zygomatic arch fractures are best visualised on a submentovertex view (view at base of skull). However, an adequate view of the fracture is usually visible on occipitomental views (see Figure 9).
In the case of comminuted and badly displaced zygomatico-orbital complex fractures the use of coronal and 3D reformatted CT scans of the orbit will give the best imaging possible to aid planning of fracture repair.
Nasal fractures
Pattern of nasal fractures
These were described in the literature.
Plane 1 injury: the injury lies anterior to a line joining the nasal bones and the anterior nasal spine and is confined to the cartilaginous nasal skeleton.
Plane 2 injury: injuries that are limited to the external nose, not involving the orbital rims.
Plane 3 injury (naso-ethmoid and naso-orbital fractures): injuries that involve the orbital walls and anterior cranium.
Symptoms
Difficulty in breathing, nosebleeds and appearance are the main problems.
Signs
Deviation of the septum and nasal bones. Flattening, dislocation and obstruction. A septal haematoma should be evacuated (drained) early to prevent cartilage necrosis.
Investigations
Plain X-ray films are of limited diagnostic value. Complex fractures of naso-ethmoidal bones warrant CT scanning to assess extent of injury.
Midface fractures
Patterns of midface fractures
Patterns of midface fractures are schematically shown in Figure 10.
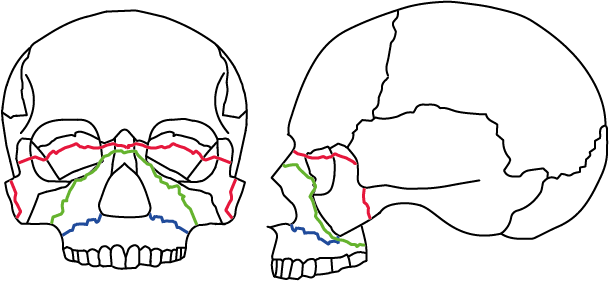
Colours in Figure 10 refer to:
Blue Le Fort I fracture; involves disjunction of the left and right maxilla.
Green Le Fort II fracture; involves fractures through the orbital floor and medial orbital wall and lateral maxillary wall.
Red Le Fort III fracture; involves disjunction of the mid facial skeleton from the base of skull. The fracture is through the pterygoid plates, zygomatic arch, FZ region and frontal nasal process bones, superior aspects of medial and lateral orbital walls.
Symptoms
These include: pain, swelling, bruising, mobility of the upper teeth (feels soft to bite), altered occlusion (usually an anterior open bite) and bilateral numbness in the distribution of the infraorbital nerve.
Signs
The following are often present: swollen face, palpable fractures, mobile maxilla (Le Fort I; see Figure 10), mobile maxilla and pyriform aperture (Le Fort II; see Figure 10), mobile midface with zygoma and separation at frontozygomatic suture and base of skull (Le Fort III; see Figure 10). Bilateral black eyes (panda eyes); bilateral numbness of the infraorbital nerves (Le Fort II). A premature contact of the posterior teeth causing anterior open bite can be seen. High impact trauma can cause the palate to split down the midline and create multipart fractures of all facial bones. Bleeding from the nose can be torrential. Major displacement produces the classic 'dished in face' appearance.
Investigations
Plain film X-ray radiographs from different angles (occipitomental views) give some information, but a much more accurate assessment of the extent of the fracture can be obtained from CT scans (see Figure 11 for an example).
CT scans also allow 3D reformatted images of the facial skeleton to be produced as shown in Figure 12.
Study models allow the patient’s premorbid occlusion to be assessed and are helpful to have in the operating room as they allow the surgeon to visualise the correct occlusion prior to fixation. They can also be used to construct custom arch bars which will be used for intermaxillary fixation during surgery and post-operatively. Obtaining impressions on a seriously injured patient in the acute phase is, however, not always possible or even humane. It may simply be necessary to work with the scans and the surgeons understanding of normal anatomy. If timing permits models can be generated without the trauma of impression taking by milling from 3D CT scanning reformatted information. Several commercial organisations offer this service.
Frontal bone fractures and frontal sinus fractures
Symptoms
In the acute setting in association with head injury it is an incidental finding.
There may be concerns over appearance or recurring bouts of frontal headache (due to frontal sinusitis), alterations in the sense of smell or nasal discharge.
Signs
The fracture involves the anterior wall of the frontal sinus, and is often associated with orbital roof fracture, naso-ethmoidal fracture, posterior wall fracture and complex cranial-vault fracture. A dural tear can lead to a cerebrospinal fluid (CSF) rhinorrhoea. A simple test to confirm CSF is to look for the presence of glucose on testing paper. Reliable laboratory assay testing for CSF specific proteins is also available.
Preoperative assessment is often difficult as there may well be a significant head injury. The patient is often on the operating table under the care of the neurosurgical team when maxillofacial involvement is requested.
In the case of a nonacute setting, frontal sinus fracture leads to cosmetic deformity of the frontal bone. If the frontal sinus mucosa is damaged or the ventilation system of the frontal sinus is impaired, a history of recurring infection may be given.
Investigations
Plain X-ray films will give only a vague idea as to the extent of the injury. CT scans are mandatory, allowing accurate assessment of the fractures; they will not provide any information on sinus function but will show fluid collection within the sinus. It therefore becomes very difficult to plan treatment with any evidence base and individualised ‘best guess’ treatment depending on presentation (acute or chronic) and symptoms is usual.
Craniofacial fractures
Craniofacial injuries may be associated with a significant head injury. In cases of complex craniofacial trauma overlying soft tissue, skull and brain may be lost (see Figure 13). Rotational flaps, free tissue transfers or tissue expansion may be needed to provide soft tissue coverage and a healthy environment for the rigid protection for the injured brain

Investigations
Further detailed imaging investigations for assessment are important. It is imperative that the brain is covered to prevent further injury. The indications for a CT scan include:
- Glasgow Coma Scale score lower than 13 when first assessed in emergency department.
- Glasgow Coma Scale lower than 15 when assessed in emergency department 2 hours after the injury.
- Suspected open or depressed skull fracture.
- Sign of fracture at skull base (haemotympanum, ‘panda’ eyes, CSF from ears or nose, Battle’s sign (bruising over the back part of the temporal bone)).
- Post-traumatic seizure.
- Focal neurological deficit.
- More than one episode of vomiting.
- Amnesia of events more than 30 minutes before impact.
Injuries to the cervical spine
Traditionally plain X-ray radiographs are the initial investigation of choice to detect cervical spine injuries. Three views of sufficient quality are needed for reliable interpretation. With rapid access spiral CT scanning being used much more frequently in major trauma centres, plain radiography of the cervical spine, although described in ATLS (Advanced Trauma Life Support) has become less common. Definitive interpretation of ligamentous injury requires MRI.