Jaw joint problems
Contents
The moist suitable treatment option(s) for jaw joint (temporomandibular joint; TMJ) disorders obviously depend on the cause of the jaw joint problems, but age and other health and further considerations need to be taken into account as well. The treatment options can be broadly divided into non-surgical (appropriate for the majority of cases) and surgical approaches. Only a small proportion of cases of TMJ problems benefit from surgery. It has been estimated that approximately 5 % of the population seek treatment and of these approximately 1 in 20 will undergo some form of surgery.
Temporomandibular joint pain dysfunction syndrome (TMJPDS)
Many treatments are available, none of which have been consistently shown to be superior to the others. Because TMJPDS is not a progressive disease, the main goals of treatment are to reduce or eliminate pain, joint noises and to restore normal function. This is best achieved when contributing factors such as stress, depression, and oral parafunctional habits (such as bruxism (grinding teeth)) are also addressed. Psychogenic factors are mostly found in conjunction with myofascial pain and dysfunction. In such circumstances psychotropic medication and psychotherapy may be beneficial.
Nonsurgical treatment
Explanation and reassurance is probably one of the most important components of treatment: the cause and nature of the disorder are benign.
Lifestyle changes include a soft diet and avoiding heavy chewing, wide yawning, chewing gum, and any other activities that would cause excessive jaw movement. Any remediable source of stress should be identified, and an attempt should be made to try and change lifestyle accordingly.
Massaging the affected muscles and applying moist heat promotes muscle relaxation and helps soothe aching or tired muscles.
Biofeedback techniques allow a patient to identify muscle overactivity and can be linked to learned techniques of muscle relaxation. This is not usually available in the hospital environment.
Jaw exercises are indicated in cases of parafunction and may prove useful for clicking joints, restricted mouth opening and recurrent anterior dislocation of the meniscus.
Analgesia involves simple non-steroidal anti-inflammatory analgesics (NSAIDs) and will relieve the pain and certainly reduce inflammation around the TMJ. These drugs also have an identifiable effect in improving the capacity of the synovial fluid (viscous fluid in the joint capsule) to act as a lubricant.
Restorative and prosthetic rehabilitation provide occlusal balance, posterior support and correct vertical discrepancies.
A variety of occlusal splints have been suggested in the treatment of TMJ dysfunction (see Figure 1).

Psychiatric support should be considered where a psychogenic element may be seen. Dosulepin, amitriptyline and nortriptyline have all been shown to be useful medications but close monitoring is essential.
Few, if any, controlled studies exist to support the benefit of ‘alternative therapies’ treatment modalities, but in refractory cases (resistant to conventional treatment) such possible treatment options include
- Ultrasound - popular with a small evidence base supporting its role in symptomatic relief.
- Laser (LILT, Low Intensity Laser Treatment) - no follow up evidence.
- Transcutaneous electrical nerve stimulation (TENS) - may provide temporary symptomatic relief.
- Acupuncture - not widely used for this condition but has a role in the management of some people’s chronic pain.
- Relaxation therapy - really an extension of self-help.
- Hypnosis - no real evidence available to support this treatment for TMJ disorders but has an established role in chronic pain treatment in general.
Surgical treatment
Injectables The presence of muscle spasm in easily accessible muscles of mastication (particularly the masseter and temporalis muscles in patients with myofascial pain as the primary symptom) has created interest in overcoming this problem. Originally it was felt that this was the main benefit of the soft coverage splint (see below) but many feel that the presence of this ‘irritant’ between the teeth may actually encourage bruxism (grinding of teeth). The widely available botulinum alpha toxin has become increasingly used (without any sound randomised controlled clinical trials) in a logical extension of an approach based on overcoming painful muscle spasm. Injected directly into masseter and/or temporalis muscles leads to between 3 and 6 months of enforced decreased muscle activity and provides apparently effective analgesia in a group of patients.
Other surgical interventions Around 5 % of patients with TMJPDS require surgery. A range of surgical procedures are currently used, ranging from arthrocentesis and arthroscopy to more complex open joint procedures (see below). These surgical procedures are more useful for cases of internal derangement with severe chronic pain or significant mechanical symptoms.
Internal derangement
Initial treatment is essentially along the lines of treatment for TMJDS (see above). When there is no response to such conservative treatment options and there is a clear internal derangement of the meniscus, ‘lysis and lavage’ (a minimally invasive procedure that involves irrigation and washing out of the joint; using Hartmann’s solution (a mixture of sodium chloride, sodium lactate, potassium chloride and calcium chloride dissolved in water)), is often helpful, achieved either by arthroscopy (see below) or simple joint irrigation (by means of suitably placed needles/syringes). If the condition relapses or locking of the jaw is a major problem, meniscal placation or eminectomy (see below) can be effective surgical treatment options.
Osteoarthritis
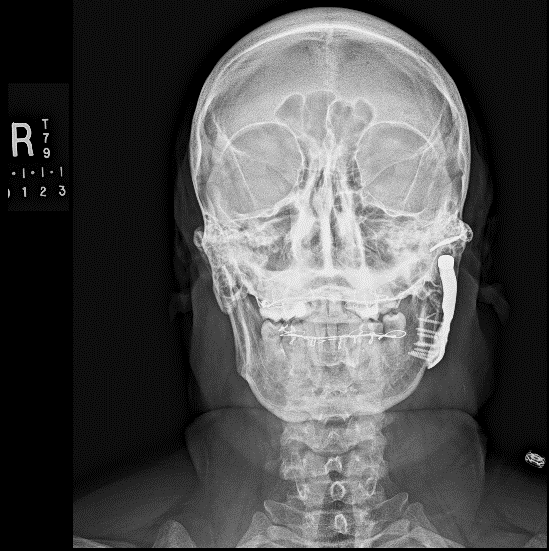
Treatment in the first instance is essentially along the lines of treatment for TMJDS (see above). However, over time the condition may require jaw joint replacement (see below). Steroid (anti-inflammatory) injections into the joint are useful for pain relief, but can damage the articulating surfaces in the joint further and may result in accelerated joint destruction. Injection of a steroid into the lower jaw joint space is shown in Figure 2.

Rheumatoid arthritis
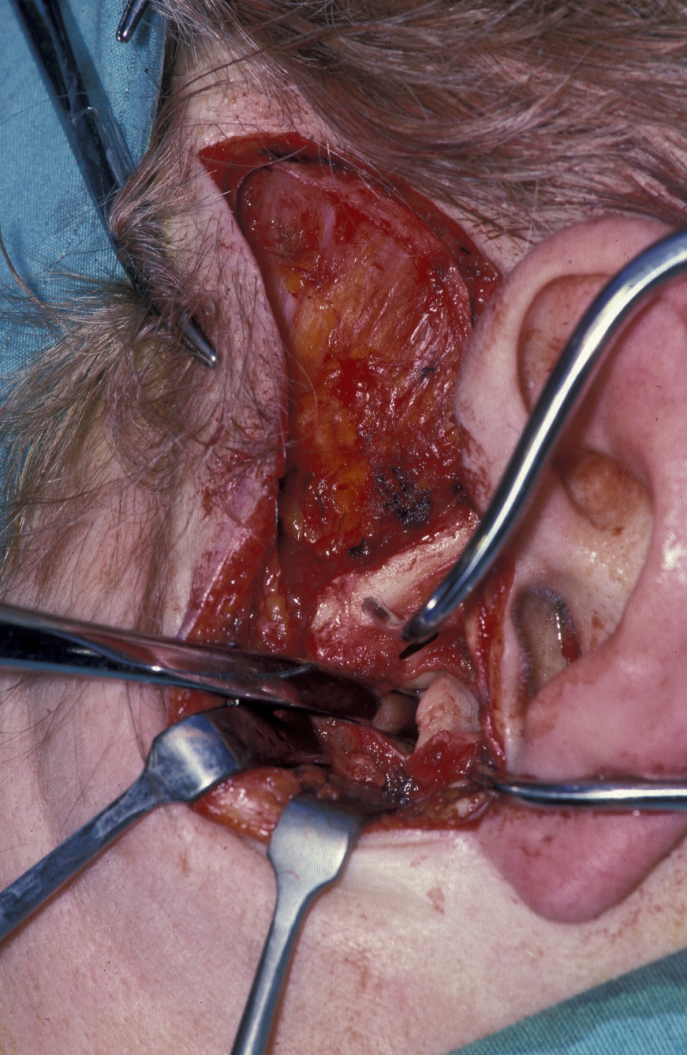
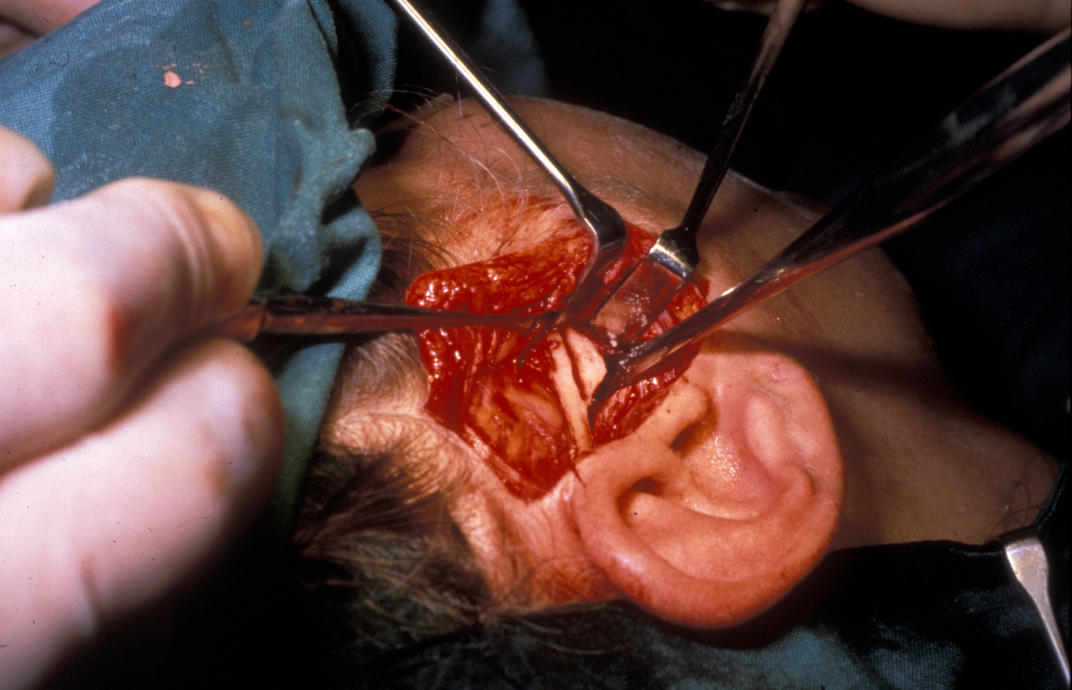
Treatment in the first instance is essentially along the lines of treatment for TMJDS (see above). Steroid (anti-inflammatory) injections into the joint are useful for pain relief, but can damage the articulating surfaces in the joint further and may result in accelerated joint destruction. Excision of pannus (inflammatory synovial (viscous fluid) tissue in rheumatoid joints that covers the articular cartilage and progressively destroys the articular cartilage) via a standard preauricular (in front of the ear) approach can relieve symptoms (see Figure 3). Total condylar destruction may necessitate prosthetic joint replacement.

Infective arthritis
Treatment includes antibiotics, and drainage of any pus. Joint lavage (see above) may be required. In young patients infective arthritis can result in ankylosis (see below), so aggressive physiotherapy and prolonged follow up are usually necessary.
Ankylosis
The key to this is identification of at risk cases and prevention. When mouth opening is mildly limited, aggressive physiotherapy is required. Mechanical obstruction is addressed by surgery to the relevant part (see below).
In adults the joint can be simply excised (gap arthroplasty (restoration of the joint)) and an interpositional material placed to prevent recurrence of ankylosis. Many such materials exist, including temporalis muscle, silastic (silicone rubber) and ear cartilage. Alternatively the joint can be completely replaced.
In the growing face of young patients, the ankylosed segment may need to be excised, but can be left, or replaced with a costochondral (rib) graft. The graft will actually grow, completely unpredictably (over, under or no growth are equally likely). Total joint replacement (see below) using either stock or custom prosthesis are increasingly recognized as a predictable and long-lasting solution.
In all cases aggressive mouth opening exercises are important. In longstanding cases bilateral coronoidectomies (removal of the coronoid process of the mandible) may also be necessary – as in any joint, if the muscles are not put through their full range of motion they will contract and fibrose.
Splint therapies
A considerable amount of hot air is generated over the value of various forms of splints. Most district hospital practices restrict themselves to simple lower soft full occlusal coverage splints. Dental practitioners with a ‘TMJ interest’ often have a range of hard acrylic splints (sometimes the same splint with a different name) which they believe in. Nobody should undergo any permanent occlusal rehabilitation until it has been verified that symptoms resolve with temporary ‘ideal’ occlusion using a removable splint.
Lower soft bite raising appliance
This is a thermoplastic polyvinyl, full occlusal coverage splint (see Figure 1 above).
A lower alginate impression is taken and the splint fitted as early as possible. The splint is worn it in the evenings and at night. Benefits are usually apparent after 1 – 2 months of wear. Quite how it works is a matter of conjecture, there being several theories, including a placebo effect. The splint may absorb excessive occlusal forces; it may allow repositioning of the meniscus, it may restore muscle balance or even vertical dimension. Whatever the reason, it eases symptoms in the majority of patients. After 6 – 8 months wearing the splint gradually has to be terminated.
Hard acrylic splints
These require considerably more refined dental techniques for manufacture and are multiple in nature, depending on the ‘occlusal theory’ they are attempting to correct. They include: the localised interference splint which is really just a habit breaker; the stabilisation splint which aims to recreate an ideal occlusion; the anterior (front) repositioning splint which postures the mandible forward; and the anterior bite plane which disengages posterior molar contact. The further reading section has details of these very dental approaches to the treatment of TMJ pain/dysfunction. All of these splints can give rise to occlusal changes and careful monitoring is necessary.
Edentulous (without teeth) TMJ patients should receive essentially the same treatment approach as dentate patients, with the obvious proviso that an adequate prosthesis may be helpful.
Currently used ‘TMJ operations’
Athroscopy and arthrocentesis (washing out synovial fluid from the joint capsule)
This minimally invasive surgical procedure involves a minimum of inserting an ‘input and outlet’ needle into the upper or lower joint space of the TMJ and irrigating the space with Hartman’s solution (see above) or saline. The idea is that adhesions are broken down and inflammatory intermediaries are washed out.
If a specially designed fibre optic endoscope (an arthroscope) is placed into the joint through a small incision instead of the input needles, the joint surfaces can be inspected; this is known as TMJ arthroscopy (see Figure 4). A number of micro-instruments or fibre-optic lasers can be delivered in this way.
After the procedure injection with hyaluronic acid (a lubricating component of synovial fluid) may be beneficial, but the evidence base is incomplete in a similar way to corticosteroids.

‘High condylar shave’
This means approaching the condyle (the rounded upper end of the mandible) by an open operation and resecting and reshaping the damaged joint surface (see Figure 5).
There has been a vogue for preserving the meniscus to allow a new lower articulatory surface to form. Current thinking is moving in favour of excision of damaged meniscus but a new articular fossa is usually implanted in these cases. Fat grafting following discectomy rather than fossa replacement has a number of advocates, particularly in North America.
Eminectomy
Eminectomy, removal of the articular eminence, is a favourite surgical approach to recurrent dislocation of the TMJ (see Figure 6).
Eminectomy becomes popular for the treatment of internal derangement approximately every 5 years. This is then followed by a period of condemning it for exactly the same problem.
Jaw joint replacement
Joint replacement is a significant operation for symptomatic irreparably damaged joints. Costochondral rib graft (see Figure 7) or customised prosthetic joints are used. The unpredictability of costochondral rib (a third are stable, a third resorb and a third overgrow) and refinements to customised prostheses have moved almost all jaw joint replacement for terminal joint damage to these devices (see Figure 8).