Facial skin cancer
Basal cell carcinoma, BCC
Numerous types of basal cell carcinoma, BCC are described clinically and pathologically (nodular, cystic, pigmented, morphoeic (infiltrative) and ulcerated) but the most important feature is that of margin definition: clearly or ill defined (see Figure 1 and Figure 2). The latter are more clinically dangerous as infiltration can extend far beyond the visible margins.

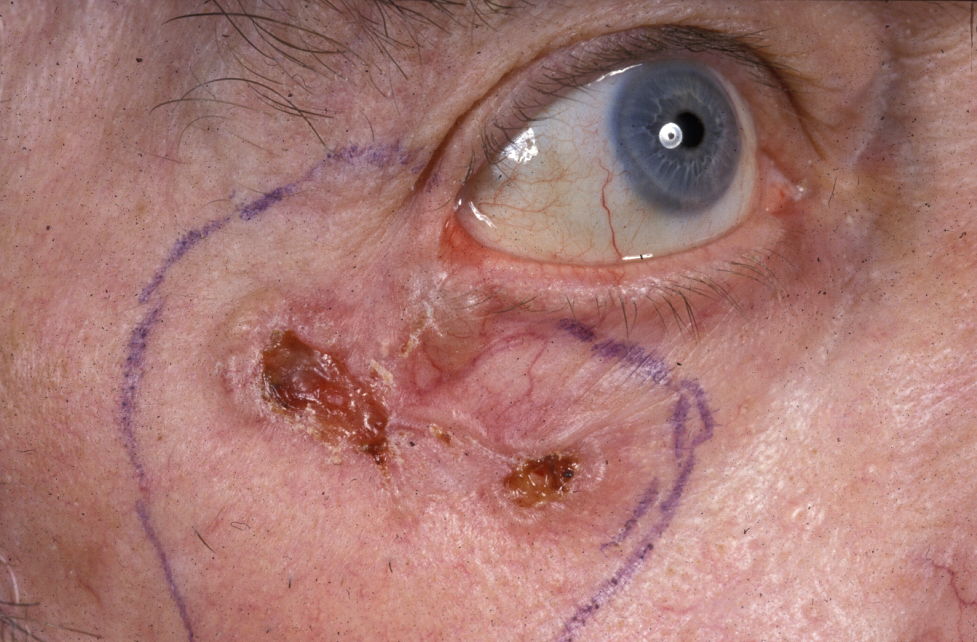
BCCs very rarely metastasise but will progressively cause local damage if neglected. They are called ‘rodent ulcers’ due to the progressive gnawing away of tissue. Their rate of growth is slow and measured in months and years (see Figure 3).

BCC is a slow-growing, locally invasive malignant epidermal skin tumour predominately affecting white skinned people. Perivascular or perineural invasion are features associated with the most aggressive forms of BCC. It is the most common cancer in Europe.
Aetiological factors appear to be genetic predisposition and UV radiation. Increasing age, male sex, fair skin types I and II (Fitzpatrick scale; type I always burns and never tans, type II usually burns and tans minimally), immunosuppression, high fat diet, arsenic exposure are other factors. Multiple BCCs are a feature of basal cell naevus syndrome (Gorlin syndrome, a rare genetic disorder which, amongst other conditions, increases the risk to develop skin cancers). The use of imaging techniques such as CT or MRI scans are indicated in cases where bony involvement is suspected or where the tumour may have invaded major nerves, the orbit or parotid gland. Broadly, the available treatments for BCC can be divided into surgical and nonsurgical, with surgical techniques subdivided into excision and destruction.
Squamous cell carcinoma, SCC
These usually arise in sun-damaged skin, especially of the scalp and ear, presenting as a raised nodule, an ulcer with raised everted edges or as a fleshy fungating lesion (see Figure 4).

Clinical differentiation between SCC and BCC is not always easy, but with SCC metastasis to the regional lymph nodes occurs much more frequently, and their rate of growth is greater (see Figure 5).

Primary cutaneous SCC is a malignant tumour which may arise from the keratinising cells of the epidermis or its appendages. It is locally invasive and has the potential to metastasise to other organs of the body. Its occurrence is usually related to chronic UV light exposure and is therefore especially common in people with sun-damaged skin, fair skin, albinism and xeroderma pigmentosum (a rare genetic disorder where repair of DNA damage caused by UV radiation is impaired; in extreme cases all exposure to sunlight becomes impossible (‘moon children’)).
Other causes include:
- ionising radiation
- exposure to arsenic
- pre-existing lesions such as Bowen’s disease (‘SCC in situ’; possibly early stage of SCC)
- immunosuppressive drugs (after transplants, inflammatory conditions)
- lymphoma or leukaemia
- human papilloma virus, HPV
Factors that influence the metastatic potential of SCC include: anatomical site, size, tumour thickness, level of invasion, rate of growth, aetiology, degree of histological differentiation and host immunosuppression. Topical agents such as imiquimod (substance that triggers interferon production in skin cells and is thought to help in this way to eliminate malignant cells by increased immune response) may have a role in preventing the development of skin dysplasia in high-risk renal transplant patients. With multiple, frequent or high-risk SCCs, prophylactic use of systemic retinoids may be considered.
Kerato-acanthoma is a self-resolving but rapidly developing skin lesion which can mimic a SCC as it produces a dome- or volcano-like lesion with central ulceration. Although kerato-acanthoma will spontaneously resolve, the diagnosis is often very difficult and concern over this means accurate histological diagnosis is needed and excision is often advisable.
Malignant melanoma
Malignant melanoma is more common elsewhere on the body, but does present on the face and is classified as follows:
- superficial spreading melanoma – the most common type
- nodular melanoma – the most aggressive type (see Figure 6)
- lentigo maligna melanoma – the type most likely to affect the face of the elderly
- acral lentiginous melanoma (most common type for people with darker skin; often affects palms of hands or soles of feet)
- amelanotic melanoma

Lentigo maligna is a pigmented patch on the face, which progressively enlarges, shows atypia of the melanocytes histologically and has the potential to develop into lentigo maligna melanoma. Early surgical excision is advised.