PET scans
Positron Emission Tomography (PET) is a diagnostic scanning technique that uses a particular type of radioactive decay (positron emission) to produce three-dimensional images (tomographs) of parts or all of the body. Generally PET monitors the difference of the uptake of a particular radioisotope in different body tissues. The radioisotopes are incorporated in suitable ‘transport’ chemicals (radiotracers) that distribute the radioisotope over the body. The most common type of clinical PET scan relies on the body’s metabolism of glucose (a sugar) in conjunction with the positron emission of the radioactive isotope 18F.
The most common clinical application of this type of PET scan is in oncology, in looking for the presence or absence of malignant tumours and/or metastases and monitoring the effects of treatments.
How it works in principle
Positron emission (sometimes called β+ decay) is a type of radioactive decay. A proton in the unstable nucleus of a radioactive isotope converts to a neutron, resulting in the emission of a positron and a neutrino. A positron is an unstable particle, something like an anti-electron: it has the same mass as an electron but carries a positive charge, rather than the negative charge of an electron. When a positron and an electron collide they essentially wipe each other out and by doing so they emit two gamma-ray (high energy) photons which travel in opposite directions. It is these gamma rays that are registered and ‘counted’ by the PET scanner.
Fluorine is one of the chemical elements of which a radioactive isotope can be manufactured that emits positrons. The normal, stable fluorine isotope is 19F (fluorine is one of the few elements in the periodic table of the elements that naturally occurs as only one isotope), the non-naturally occurring fluorine isotope 18F is a radioisotope that emits positrons. The half-life of 18F is roughly two hours, so it is a fairly short-lived isotope.
Producing 18F requires access to a cyclotron or a linear particle accelerator. A common process to make 18F starts from a sample of water where the water molecules are all labelled with the (stable) 18O oxygen isotope, 18OH2. These water molecules are bombarded by accelerated protons (H+ ions). These collisions give 18F- ions dissolved in water.
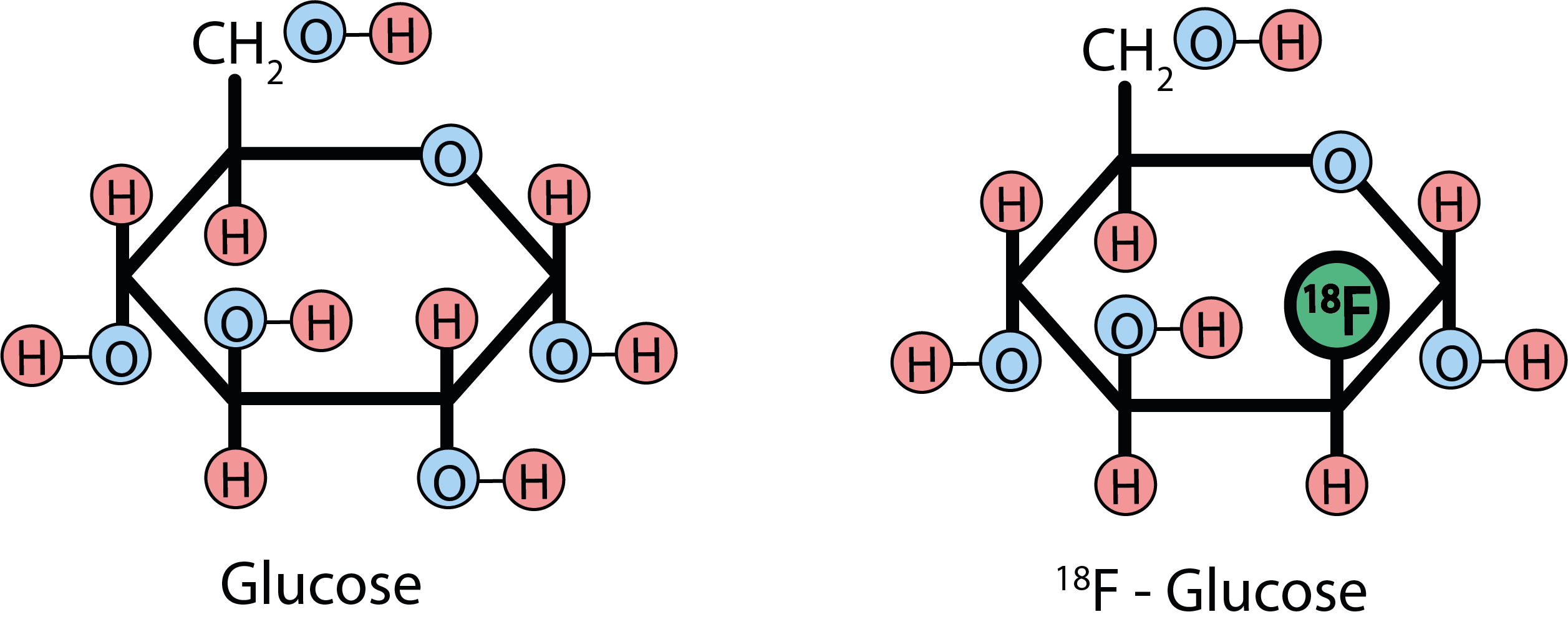
Once the relatively short-lived 18F isotopes are produced in this form, there is only little time for specialised chemical synthesis in which the 18F isotopes are incorporated as radioactive labels into a glucose molecule. Figure 1 compares the normal glucose molecule (left) with its 2-deoxy-2[18F]fluoroglucose counterpart, FDG (right) that is commonly used in PET scans as the radiotracer.
Unfortunately it is not possible to first synthesize FDG and then irradiate the chemical to produce the radioactive 18F label as irradiation in the accelerator or cyclotron would destroy the glucose molecules. Given the relatively short half-life of 18F, it is obvious that running PET scans is quite a logistical challenge and exact timing and booking is essential for a successful operation of such a scanning facility (you can contribute to the success of such a facility by arriving on time for your appointment). It is also obvious that PET scans are a fairly expensive scanning technique, when taking all underlying processes into account.
Before your PET scan you will be given a fairly small dose of FDG. You will be asked to quietly wait for about an hour, to give your body’s metabolism undisturbed time to pick up the 18F-labelled glucose molecules and distribute them around the body. You will probably also have been asked not to eat for several hours before the scan and for people with diabetes special considerations about this glucose (sugar) radiotracer need to be taken into account.
The contrast in images derived from PET scans originates from the difference in uptake of glucose by different organs and body tissues. For example, the cells in the liver and brain have a high rate of uptake of glucose, and so do the cells in many malignant tumours. This can be problematic in interpreting the scans and only radiologists with special additional training interpret PET/CT scans. Once the 18F-labelled glucose is incorporated into a cell, it cannot be metabolised any further as normal glucose would be in the cell cycle. Accordingly, the amount of radiotracer detected gives a measure of the glucose uptake by the metabolic activity of the different organs and tissues from the snapshot taken by the PET scanner.
The mechanism by which PET scans provide data from which three-dimensional body images can be constructed is different from those in CT or MRI scans: PET collects data about a body function, for example the different uptake of glucose by different organs and body tissues and thus monitors a metabolic process. Both CT and MRI scans give information about the structure of different body parts and tissues. The spatial resolution of PET images is not as good as that in CT or MRI scans but PET offers unique and complementary information.
Is it safe?
Yes; the amount of high-energy radiation you receive from a PET scan is similar to the radiation dose of a typical CT scan. A single such scan is extremely unlikely to do any harm but any use of high energy (ionising) radiation always should be subject to a careful risk / benefit analysis, especially when repeatedly such scans are carried out. FDG is a harmless chemical.
How long will it take?
The overall procedure may stretch your patience a little. After you have been given the radioactively labelled glucose, you will have to wait quietly for about an hour for the labelled glucose molecules to be transported to every corner of your body. The scan itself will also take some time, some 20 minutes or so, and you will have to be able to keep still and lie quite flat during the scan so that clear images can be recorded. The exact duration of a scan, or series of scans, depends on the kind of tissue and the parts of the body being investigated.
The main reason why it takes quite some time to collect the data for a complete PET scan is the need to have a good enough (with a fine enough grid of sampling points) set of data that afterwards can be converted into a good-quality three-dimensional image; a good quality image provides good resolution and good contrast.
Does it hurt?
No; a PET scan is a painless procedure. However, some people find confinement in any kind of scanner, especially MRI or PET, a little claustrophobic. The best advice really is to relax and ignore these environments as best you can – it is not in any way dangerous, just not particularly ‘nice’. After your PET scan is finished you may be asked to wait for a few more minutes while your scan data are roughly checked to ensure that the data are of good technical quality and can be properly processed and interpreted later on (to avoid that you may have to come back for another scan just because the scan data were not quite good enough first time round).