X-ray
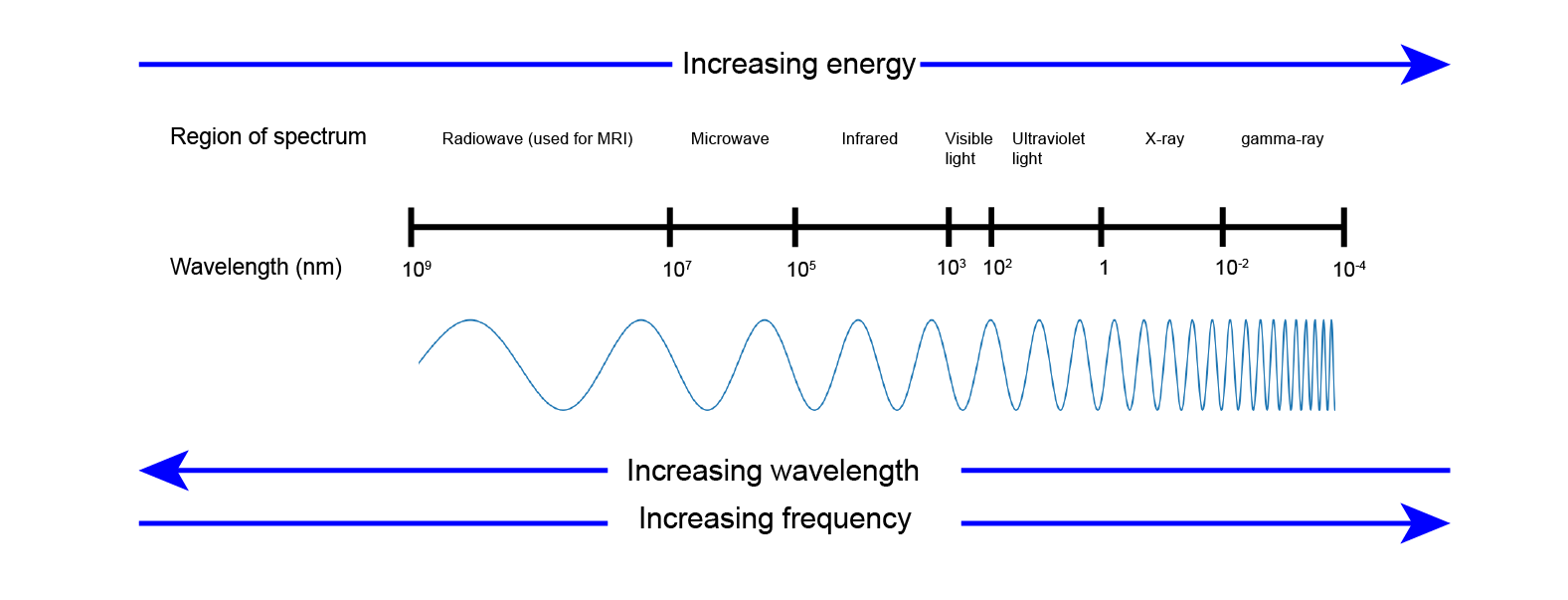
X-rays are radiation in the ionising, high-energy range of the electromagnetic spectrum of radiation (Figure 1). We cannot see this form of radiation because the human eye is only capable of observing frequencies within the narrow band of visible light. X-rays are utilised in the diagnosis (radiography) and treatment (radiotherapy) of numerous conditions.
X-ray radiation was first discovered in 1895 by the German physicist Wilhelm Conrad Röntgen who named it ‘X-radiation’ to signify its unknown nature. Radiation in this frequency range is important because it has enough energy to pass through materials that are opaque to visible light and other forms of electromagnetic radiation. The ability of X-rays to pass easily through skin, plastic and so on makes this a powerful imaging tool for use in medicine and other areas - to ‘see’ inside the body, or in airport security to check luggage; the list of X-ray applications is long.
The basic physical principles outlined below equally apply to CT scans. Ordinary X-ray images are two-dimensional projections of X-ray representations of parts of the three-dimensional body. CT scans instead take multiple X-ray images of a three-dimensional object from many different angles and in this way permit the reconstruction of three-dimensional images from the complete data set.
Radiography as a diagnostic imaging technique aims to create the highest possible X-ray image resolution with the lowest possible radiation dose in order to prevent any unnecessary tissue damage from exposure to high-energy radiation.
How it works in principle
X-rays are produced when the kinetic energy of sufficiently fast (accelerated) electrons is converted into electromagnetic radiation, that is photons. In medical imaging this is primarily done using so called X-ray tubes. An X-ray tube is an evacuated glass vessel housing two electrodes: a negatively charged cathode and a positively charged anode. The cathode typically consists of a tungsten filament and is the source of the electrons. The anode is similarly constructed using an outer surface of tungsten and is the target of the electrons.
When a high voltage is applied across the tube, electrons are emitted from the cathode. These accelerate towards the anode and, on striking the target, cause the emission of photons with energies in the X-ray range. In order to record an X-ray image, the relevant part of the body will be strategically positioned between the X-ray source and a detector. Positioning is important both to ensure enough X-rays are detected (for good spatial resolution of the image) and to keep the radiation dose received as low as reasonably possible (to avoid tissue damage; known in the medical world as ALARA – as low as reasonably achievable). There are many different types of detectors, depending on the application area of X-ray investigations.
X-rays travel in straight lines (like visible light) from the source and, on passing through the body, are attenuated (weakened) by interactions with the various body tissues. Historically X-ray images were recorded on photographic film and developed using a dark room.
Different tissues absorb X-rays at different rates and this differential absorption creates the familiar ‘shades of grey’ contrast seen in X-ray (and CT) images. Calcified structures such as bones and teeth absorb X-rays most strongly and thus appear white on the traditional photographic film radiographs, since fewer X-rays are reaching the photographic film. Air barely absorbs any X-rays, resulting in a blackening of the image corresponding to such regions. Soft tissues (fat, muscle, organs) have varying levels of absorption and appear as shades of grey on the image. We cannot feel the passage of X-ray radiation through the body.
The use of photographic film in radiography has now largely been superseded by digital technologies. Digitally recorded X-ray images have some advantages over traditional film. Digitally recorded X-ray images can be immediately viewed (and shared) on high-resolution computer screens and the image data can be easily stored. The radiation doses required for digital X-ray images tend to be slightly lower than with the use of traditional film X-rays: digital data can be electronically enhanced, so an essentially lower-resolution data set may still provide an acceptable image resolution.
Digital X-ray images typically still look like old-fashioned ‘shades of grey’ X-ray images recorded on photographic film, mainly because the companies producing X-ray imaging equipment were afraid of causing culture shock in the medical community by switching to a completely different pictorial representation of X-ray images. This point is not quite as trivial as it may seem: the human eye can only distinguish grey-scale contrast above a certain threshold; alternative visual representations of X-ray (and other digitally recorded) imaging results may well have technical advantages – there is an ongoing discussion about this.
Dental panoramic radiograph (DPT)
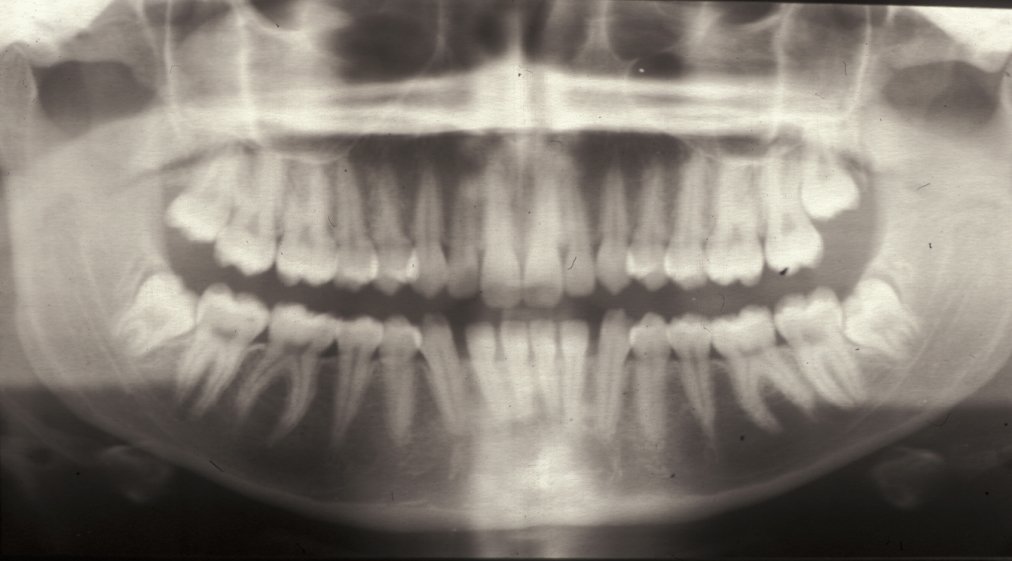
One of the most commonly used X-ray examinations for oral and maxillofacial conditions is the dental panoramic radiograph (DPT), a panoramic X-ray image of the upper and lower jaws and teeth.
Obtaining such a panoramic, extra-oral radiograph involves a rotating mechanism with the X-ray source and the detector placed opposite to each other and the head carefully positioned in between. For recording the image, the X-ray source moves in a semi-circle around the back of the head and the detector moves similarly in a semi-circle opposite the X-ray source. Careful positioning of the head permits focus mainly on the upper and lower jaw regions while deeper and more superficial structures will be blurred in the image. The idea is to i) maintain a constant distance between the focus region to the X-ray generator and the detector, and ii) to obtain a perfect perpendicular projection at every stage of the screening. It is impossible to find such a perfect solution and the acquisition of DPTs is by necessity a practical compromise.
In practice, these panoramic images do show projection artefacts and ghost images, and there is a shadow from the cervical (neck) spine. It is important to remember that a two-dimensional representation / projection of a three-dimensional object will never be a perfect representation. Overall, a DPT does not provide highly defined local detail but gives a very good overview with a relatively low exposure to X-ray radiation– in many practical situations very highly resolved local detail is not required anyway. Panoramic radiographs can also be obtained for people suffering from trismus or from a particularly active gagging reflex, both making the recording of intraoral radiographs difficult or impossible. Figure 2 shows an example of a panoramic radiograph.
Plain X-ray film
Mainly used in the domain of dentistry (bitewing radiographs for single teeth) but also with some applications in oral & maxillofacial surgery investigations, the intraoral placement of a piece of X-ray film together with a suitable choice of angle for taking the (single) X-ray image and projecting it onto the film can provide useful information. For example, calculi (stones) of the submandibular or sublingual salivary glands can be well characterised by such a straightforward plain radiograph.
Cone beam computed tomograph (CBCT)
Cone bean computed tomography, CBCT, is a more recent technique to obtain X-ray images of the head and neck region. The method uses a differently shaped X-ray beam (a cone shaped beam) and was introduced as an alternative to both DPT (see above) and CT imaging. The radiation dose is significantly higher than for a DPT image, but significantly lower than in a CT scan. CBCT images do suffer from artefacts similar to those in DPT images. CBCT has been advertised as the new gold standard of X-ray imaging in dental and oral applications – its benefits and disadvantages remain to be properly assessed.
Common contrast agents in X-ray investigations
Sometimes the use of a chemical substance called a contrast agent is required to improve the contrast in an X-ray image, enabling investigations on structures that would otherwise be difficult to observe. The ideal contrast agents should give maximum contrast for minimum effective radiation dose and have few, or no, adverse effects.
Contrast agents for X-ray investigations work by accumulating in structures/organs and need to be extremely efficient at absorbing X-rays. ‘Heavy’ elements (relative to the other chemical elements in the body) fulfil this task as X-ray contrast agents: the atoms of heavy chemical elements have a large number of electrons, and they absorb X-rays via the so-called photoelectric effect. The more electrons in an atom of a substance, the more efficiently it will absorb X-rays – X-ray radiation will efficiently knock out ‘photoelectrons’ from such X-ray contrast agent substances.
This excellent power of absorption of X-rays by contrast agents strongly enhances the contrast in X-ray images between the investigated area (where the contrast agent accumulates) and surrounding tissues. The most commonly used X-ray contrast agents are barium sulphate and iodine, with both barium and iodine being heavy chemical elements.
Barium sulphate is a white powder which is administered orally as a thick suspension in water. Barium sulphate is used because it is essentially insoluble in water, hence will leave the body as it entered and hence has no toxic side effects. It is used for a type of X-ray investigation called a ‘barium swallow’ to examine swallowing difficulties (when swallowed, the barium sulphate suspension coats the lining of the throat and gullet, giving very detailed images of these structures and their functions). The swallowing process is examined along the passage through larynx and pharynx (throat) and oesophagus (gullet) by sipping some barium sulphate suspension, followed by recording essentially an X-ray video of the swallowing process.
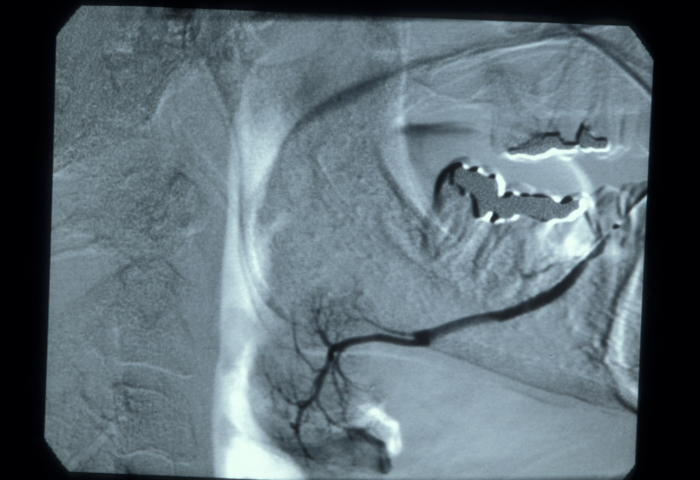
Iodine (in an aqueous solution) is used as an X-ray contrast agent for the examination of obstructions in the ducts of salivary glands, the recording of a sialogram. The iodine solution is injected into the salivary gland duct, followed by the recording of X-ray images to track the flow as well as structural local details. An aqueous, rather than an oily, iodine solution is used because it has low viscosity (hence will help to depict very fine detail) and does not cause any lasting problems if there is a leakage from the duct. Figure 3 shows an example of a sialogram. There may be some minor discomfort with the injection of the iodine contrast agent into the duct of a salivary gland. Iodine as a contrast agent has the advantage of being a bacteriocidal (killing bacteria) substance, although it is also quite allergenic.
Contrast agents commonly used for X-ray investigations are usually well tolerated.
Radiation dosage exposure in diagnostic X-ray imaging
Diagnostic X-ray imaging uses the lowest possible dose of radiation, the recording of a single X-ray image of a small area, such as a single tooth, only leads to radiation exposure for a fraction of a second. When thinking about X-ray radiation exposure from medical imaging, it may be useful to remember that we are being continually exposed to naturally occurring, ionising background radiation from the environment. For example, recording of a DPT image results in radiation exposure to approximately 0.01 mSv (milliSievert; Sievert is the unit in which radiation dose is often measured), equivalent to approximately 1.5 days exposure to natural background radiation. This is different with CT scans: a CT scan of the head amounts to 2 mSv radiation dose, equivalent to natural background radiation of approximately one year.
As with all interventions, risks and benefits must be weighed. These considerations will be different for a pregnant woman, for an infant or for an elderly person.