Nutrition
Apart from the sensual and social pleasures of eating & drinking, there is also a more technical component to consider. We need to understand the nutritional input required to keep our bodies properly nourished. Consideration of these nutrition aspects is an inaccurate ‘science’ and a healthy dose of common sense is probably the best approach to this topic. In part this is due to the fact that much of the food and drink narrative is completely entangled with cultures and traditions, with everybody having some over-familiarity with certain aspects of eating & drinking (which drives some non-scientific approaches) as well as increasing influences of industrial food production in Western countries from the mid to late 20th century.
Obviously, there are a few key facts concerning nutrition, which we outline below. Beyond these key facts, common sense strongly suggests the following: in situations where eating is a serious, possibly long-term challenge, none of the common dietary recommendations, such as ‘five-a-day’, apply easily. Special circumstances require special approaches and that includes nutrition and diet for a good number of oral & maxillofacial patients.
The one recommendation that probably applies to most maxillofacial patients with longstanding difficulties in eating enough by mouth is; do not panic about common wisdom and recommendations about a ‘healthy diet’. Malnourishment (or rather: undernourishment; obesity is also a form of malnourishment) is definitely not healthy. A suitably adapted high-protein, high-calories diet, made up by good-quality foods, can go a long way in preventing undernourishment while minimising the efforts with eating and, hopefully, maximising the pleasures of eating. Any missing components from such an adapted diet can be supplemented as and when needed. Furthermore, be aware that difficulties with eating and swallowing are highly individual and vary enormously, even for people suffering from otherwise very similar conditions.
Accordingly, individual solutions for such problems is what is needed! The best way to find optimal individual solutions, including changes over time, is to cook at home, from scratch. It is the best way not only to adjust textures, taste and temperatures as needed / preferred, it also gives complete control over the quality of ingredients and the composition of food – and it tends to be the least expensive route to a healthy, adapted diet.
First things first, let us have a look at the basic principles of feeding the body, and work out from these facts how one can optimise nutrition obtained from limited amounts / volume / type of oral food intake.
One, easy way to keep an eye on one’s nutrition requirements is to keep a food diary. This is a completely non-judgemental way to identify any potential deficiencies, and to learn about what does and what does not work.
The components of our diets
In terms of nutrition the foods we eat are made up of macronutrients (proteins, carbohydrates, fats (and alcohol)) and micronutrients (vitamins, minerals and other trace elements) and the ubiquitous elixir of life, water.
Water
Staying hydrated and drinking enough for many with swallowing problems is probably the biggest challenge. When safely swallowing liquids is the main problem, a variety of methods to thicken liquids, or turn them into jellies can make a major difference. Thickened liquids, or jellies all count as liquid intake. All that has happened is that problematic liquids have been modified such that they are easier and safer to swallow (see our recipe data base for tasty inspiration and read about texture modifying of many foods). In particular gelatin-based jellies make excellent ‘liquids in disguise’, these jellies preserve taste and are easy to swallow because of the particular melting properties of gelatin-based jellies. In short: there should be safe & tasty ways to stay hydrated for almost everybody.
Macronutrients
Macronutrients are the source of energy and essential nutrients from our foods. Different foods are made up by different compositions of macronutrients. For example, pasta is essentially pure carbohydrates. Milk is a mixture of proteins, carbohydrates and fats in the form of an emulsion (an oil-in-water emulsion) whereas cream is a mixture of the same three types of macronutrients but with a higher relative fat content than milk (a polemic comment about skimmed milk: there is very little point in using skimmed milk in order to cut down on consumption of saturated fats – if that is the aim, spreading a little bit less butter on the toast is more effective; do the numbers! A slightly less polemic comment about milk, in favour of full milk: the ever so slightly higher fat content of full milk can well make a big difference in terms of lubricating some other foods, when that is a consideration (as is the case for many people with xerostomia (dry mouth)). Beer is a dilute solution of alcohol, some carbohydrates and proteins in water, so effective that the German Winter Olympic team used an alcohol-free specialist Bavarian beer ‘Weissbier’ as a nutritional supplement (because this type of beer contains yeast).
This gives a first hint about the usefulness of variety in any diet: a balanced, varied diet will automatically provide ‘something of everything’. Some traditional, often century-old local food traditions happen to provide automatically a good balance of some macronutrients. Good examples of such useful traditional combinations are rice & red beans, or rice & soybeans.
The different types of macronutrients provide different amounts of energy per consumed unit. A traditional (but non-scientific) unit to quantify the energy content of foods is kcal/g (the scientific measure for units of energy content of food materials is kJ/g):
- carbohydrates: ca. 3.8 kcal/g (ca. 16 kJ/g)
- proteins: ca. 4.0 kcal/g (ca. 17 kJ/g)
- fats: ca. 9.0 kcal/g (ca. 37 kJ/g)
- alcohol: ca. 7.0 kcal/g (ca. 29 kJ/g).
This brief overview, for the moment concentrating only on the energy content of the four types of macronutrients, suggests the following. In terms of calories per unit eaten, fats are the most energy-dense food (with alcohol a close runner up, although we usually do not consume undiluted alcohol). Proteins and carbohydrates are similar in energy density. Trying to follow a low-fat diet while being confronted with oral food-intake problems is obviously not a good idea, for a number of reasons (not just with respect to energy intake but also with respect to lubrication of other foods). A glass of beer or wine (unless there are other reasons to stay away from alcohol completely) not only is useful for many people to improve their appetite and/or make a meal more enjoyable, it may be a simple way to add energy content to the diet (or, at the other extreme: if losing weight is wanted / needed, reducing alcohol intake is a good choice). An empirical overall average energy intake of 2000 kcal per day for women and 2500 kcal per day for men is a standard recommendation, assuming ‘standard activity levels’ (whatever that may be…).
If the intake of macronutrients was only concerned with their respective energy density, a fat-only diet would obviously provide the most energy for the least amount of food eaten. Matters are not quite so simple because the various macronutrients have further and varied body-nourishing functions. In addition, not all food categories are equally easy / difficult / impossible to handle for many maxillofacial patients who find eating a challenge. So, let us next examine the additional nutritional roles of the four categories of macronutrients.
Alcohol is a special case amongst the four categories of macronutrients in that it only provides energy / calories but no further significant nutritional benefits. However, we should not dismiss its indirect benefit as a potential appetiser (or even mood enhancer) for special circumstances.
Proteins are essential food components for a number of reasons, not just to provide energy. It is essential to continuously provide proteins in the diet as the body’s metabolism uses up proteins from dietary supplies quickly in its maintenance of function and structure, including the body’s own protein components (muscles and skin for structural proteins, for example). In terms of function, proteins are involved in essentially all cellular metabolic processes.
Chemically proteins are all composed of modular building blocks, amino acids (Figure 1), connected by so-called peptide bonds.
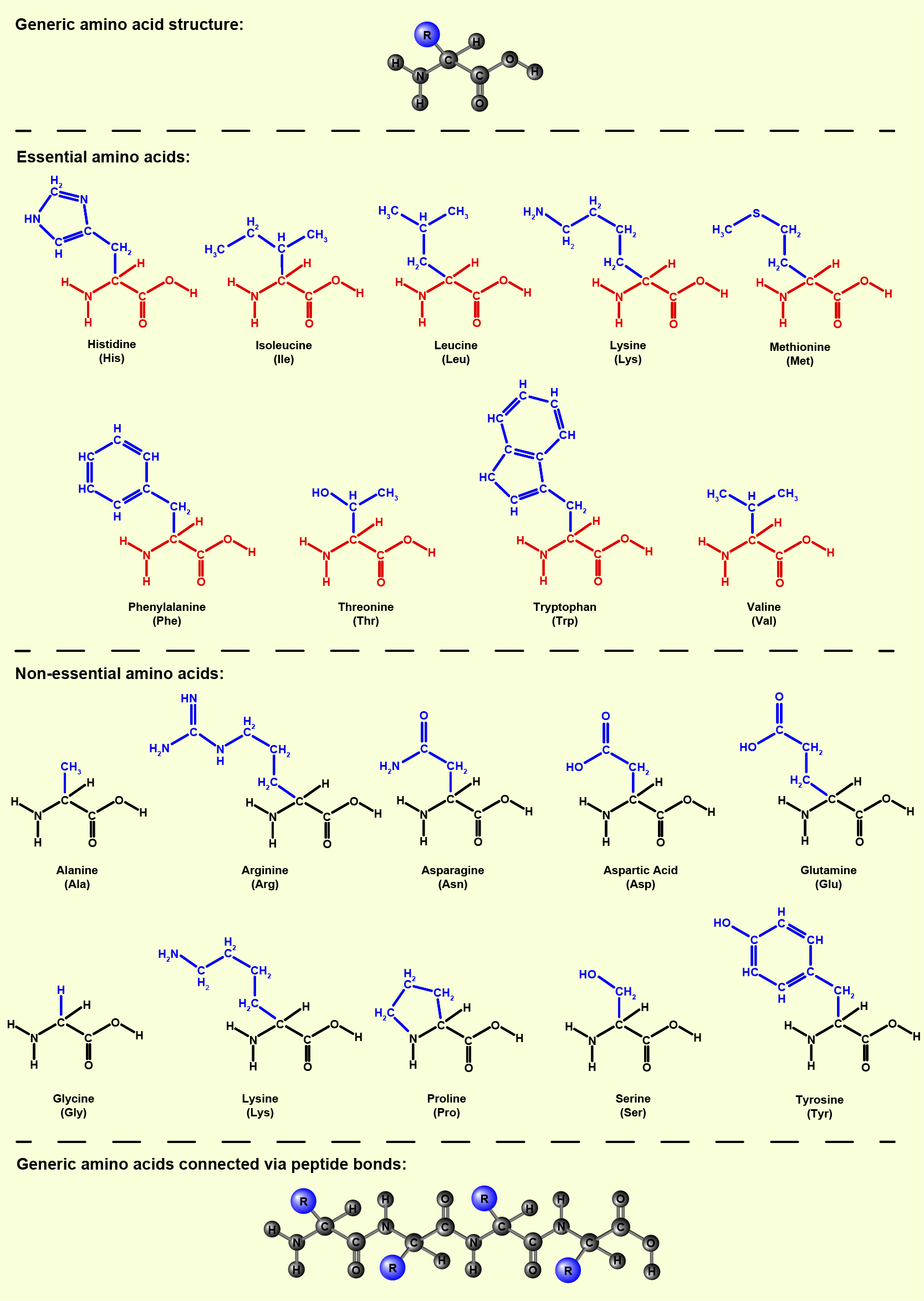
Some amino acids are synthesised in the body; these are called non-essential amino acids (but this does not mean that they are not important in metabolism). Some amino acids are not synthesised by the human metabolism and thus need to be provided by dietary sources. The needs of amino acids supplied by dietary sources differ slightly for children and adults.
Sources of proteins with particularly suitable overall amino acid composition to cover all needs are found in animal-derived foods; meat, eggs, fish and dairy products. Proteins from plant-derived foods usually have a less broad composition in terms of amino acids. That can be compensated for by a pick & mix approach, by combining several foods (for example, wheat-based foods (bread) and lentils together have a complete amino acid profile). Particularly useful plant-based protein sources are all pulses (including soy bean products) and cereals. For any vegetarian, vegan or otherwise mostly plant-based diet, the diversity of daily foods is particularly important for a complete and balanced protein supply. Protein deficiency in the diet should be avoided as far as possible as this type of diet deficiency leads rapidly to muscle wasting, vulnerability to infections and poor wound healing.
Carbohydrates typically are a significant contributor to the overall energy intake from food in a typical Western diet, although the relative amounts vary hugely across diets in different regions of the world. In some parts of the world 80 to 85 % of the dietary energy intake stems from carbohydrates, whereas in some other parts of the world it is as low as 30 %. Carbohydrate fractions tend to be high where the local diet is predominantly plant based (by and large it is plant materials that provide dietary carbohydrates). Usually diet patterns low in carbohydrates are high in fat, and low-fat diets tend to have a larger carbohydrate component (including sugar).
This degree of variability of composition of diets across the world is good to remember as many maxillofacial patients find traditional Western carbohydrate-rich foods difficult to eat (think of stodgy, sticky mashed potatoes, or similar). Furthermore, the simplest of all carbohydrates, ordinary sugar (glucose) is on the to-be-avoided list of many maxillofacial patients for a number of reasons. This could be a short term issue (for example, to give oral wounds or ulcers time to heal and minimise infection risk by avoiding sugar), or it could be a long term issue in particular for those suffering from dry mouth, xerostomia and/or difficulties opening the mouth, trismus where high sugar contents of food and drinks exacerbate dental decay problems. In short, there is no need to worry if the carbohydrate component of the diet is reduced and in part replaced by proteins and fat; this does not prevent a varied and healthy diet overall as long as an appropriate level of energy intake is achieved.
The simplest, smallest carbohydrate molecule is glucose, C6H12O6 (ordinary sugar). Glucose molecules can form dimeric and linear or branched polymeric molecules of variable size, perhaps better known in everyday life as ‘starches’. Figure 2 gives a schematic view.
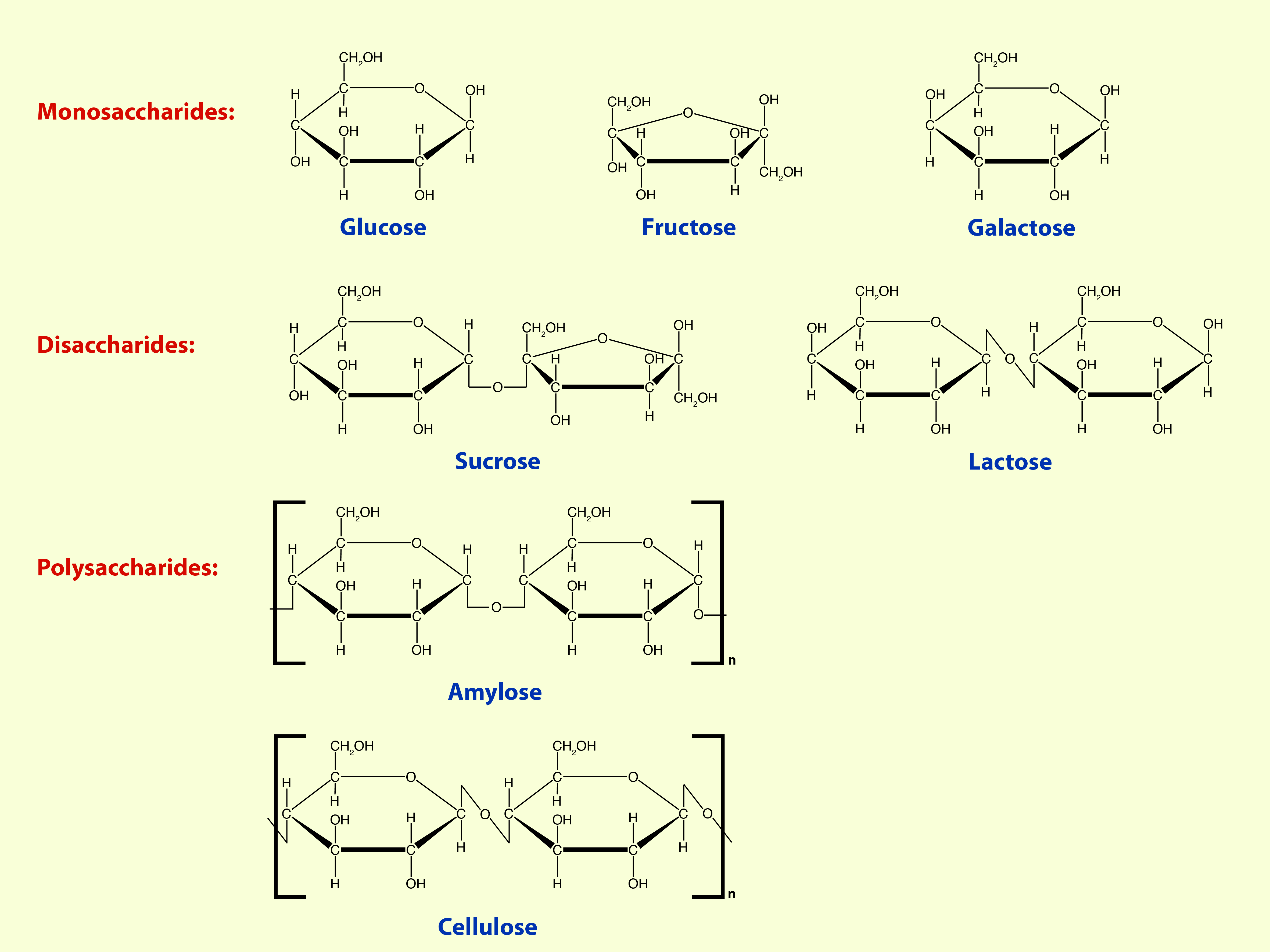
Oal intake of sugar (often hidden in considerable amounts in processed and ‘low fat’ foods and declared in misleading terms on the packaging) is problematic in a range of oral and maxillofacial conditions. Remember carbohydrates as such are not all problematic and serve important roles in digestion and energy supply to the body. Polymeric carbohydrates (usually referred to as polysaccharides) can be subdivided into two groups: those that are soluble and are broken down into small units in the digestive process, and those that cannot be digested.
Soluble polysaccharides, after being broken down in the digestive system into smaller fragments, are absorbed in the small intestines and provide energy to the body by ending up as glucose in the blood stream. Different sources of soluble polysaccharides release blood glucose at different rates; this is called the glycaemic response. If it takes longer to break down a particular polysaccharide, we feel satisfied for longer and with a slow and steady glucose supply to the blood stream, there are no insulin spikes (some pricey specialist energy gels used in endurance sports highlight this point as the marketing driver, emphasising that slow release carbohydrates help to support gluconeogenesis over long events). In the endurance events of everyday life, for example pulses and oats provide polysaccharides with a slow glycaemic response, potatoes or pasta are carbohydrates with an intermediate rate of glucose release. Any sugary foods or drinks and white bread provide glucose instantly, but with no long-lasting effect – one feels hungry soon again.
Insoluble polysaccharides are not digested and are commonly referred to as ‘fibres’. Despite not being digested, they have a very important role in the digestive system. Most insoluble polysaccharides belong to the chemical class of cellulose (see Figure 2). Cellulose derivatives can take up large quantities of water and swell in the process. This is what happens with insoluble polysaccharides in the colon, the swelling of these fibres encourages peristalsis (forward-pushing motion of the intestines) by bulking up the processed food in the intestines and reduces constipation. Some fruit, many vegetables and in particular whole grains provide variable amounts of insoluble polysaccharides. In some diets that are feasible as oral food intake for some maxillofacial patients, insoluble fibre may have to be added as a supplement. A low-fibre diet or insufficient fluid intake are not the only possible reasons for constipation. Opioid analgesics also cause constipation. Often alongside opioids a synthetic form of insoluble fibres is prescribed (containing gels that swell in the intestines, and bulk and soften stools just as insoluble fibres in the diet do; this supplement only works with sufficient fluid intake).
Table 1 gives a brief summary of some common sources of soluble and insoluble fibres.
Table 1 Common dietary sources of soluble and insoluble fibres
| Soluble fibre | Insoluble fibre |
|---|---|
| oats | oats and maize |
| beans and pulses | beans and pulses (including lentils) |
| fruit (including apple, pear, berries, citrus) | all whole grain foods |
| essentially all vegetables | seeds and fruits with edible seeds |
Fats in our diet all belong to the class of chemicals called lipids, that is chemical compounds that are insoluble in, and immiscible with, water. These properties require fats to form complexes with some specialised transport proteins in order to be carried around the body by blood without separating from this water-based transport medium. A number of different lipids play a role as dietary fats, including triglycerides, phospholipids and sterols (such as cholesterol) (Figure 3).
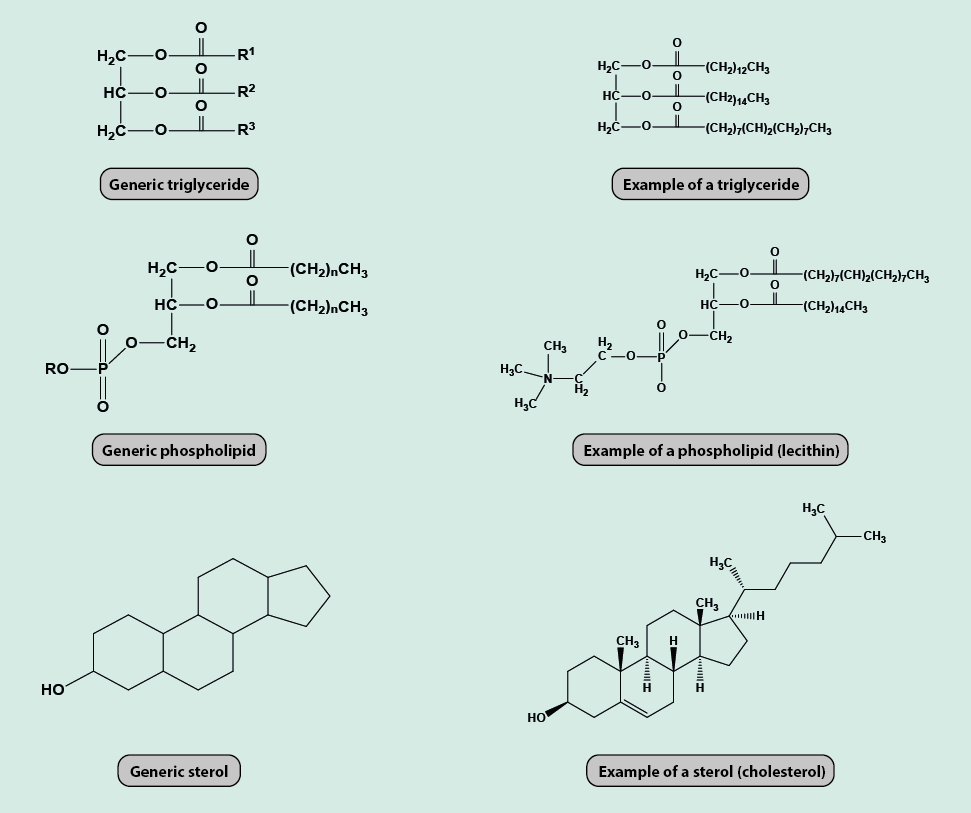
The main dietary role of fats is their provision of energy. In addition, fats in the diet are necessary to ensure the uptake of essential nutrients by acting as a carrier for nutrients that are not soluble in water. For example, vitamins A, D, E and K (see below) are only soluble in fat. Dietary fats also act as the carrier phase for many chemicals that are responsible for the taste of foods, in addition to acting as an important lubricant for foods. Some dietary fats are important for being metabolically converted into steroid hormones, prostaglandins, and some lipids that are crucial for the functioning of cell membranes. Cholesterol is an important dietary component that is only found naturally in animal-derived food. It is important in the digestive process (being a precursor of bile acids) as well as in its role as precursor of several hormones and vitamin D. Some closely related plant-derived sterols (phytosterols) exist as well.
Micronutrients
Micronutrients do not significantly contribute to the energy intake from food, they are only needed in tiny quantities. However, the right amounts and composition of vitamins, minerals and other trace elements are essential components to keep the body alive and healthy. As a rule of thumb, it can be assumed that a varied diet that includes a generous range of different foods on a regular basis will provide all necessary micronutrients. Many of the sometimes costly, dietary supplements are usually not necessary. If there are any proven and persistent deficiencies of micronutrients, these do need to be replenished; vitamin B12 deficiency being a typical example which cannot be resolved be dietary manipulation.
Vitamins are organic compounds that are necessary in small quantities to maintain a wide range of essential body functions. Some vitamins are water-soluble, others are fat-soluble (A, E, D, K); some vitamins can be stored by the body while others are needed to be constantly supplied.
Minerals and electrolytes (including calcium, iron, zinc, copper, iodine, selenium, magnesium, manganese, cobalt, molybdenum, sodium and potassium ions, as well as fluoride, chloride and phosphates) have many different roles in metabolism and are provided by many different dietary sources. Everybody probably remembers from school or historic movies the massive health effects of poor diet and resulting nutritional deficiencies in times long gone (in the developed world), such as severe vitamin C deficiency (scurvy) or rickets (bone disorder associated with severe vitamin D deficiency). No such serious effects from poor diet are likely to be seen nowadays, at least not in the Western world. However, more subtle effects of micronutrient deficiencies do play a role in health. For example, lack of iron or zinc ions, or low levels of a number of B vitamins (thiamine, B1, riboflavin B2, folate, B9; cobalamin, B12) have all been associated with otherwise idiopathic (unknown cause) burning mouth syndrome.
To cut a long story short:
- it is wise to ignore any hypes about superfoods and the latest fads about diets;
- it is wise to work from the basic assumption that the body is made to be fed by mouth, and as much as that is possible – it should be attempted;
- it is wise to switch on common-sense mode when thinking about a suitable and varied diet;
- it is wise to take control and stay away from processed foods;
- it is wise to try and enjoy food, however difficult;
- it is wise to think outside the box and try new and unusual foods;
- it is wise to consider keeping a food diary if the diet seems a little restrained.