Anticoagulant medications
Anticoagulant medications (mistakenly called ‘blood thinners’) are a group of substances, widely prescribed in the prevention and treatment of venous thrombosis, the blocking of a smooth blood flow in the veins by a clot (antiplatelet medications are used for very similar purposes addressing conditions of the arteries).
Anticoagulants are widely used because cardiovascular diseases (such as cardiac conditions) are extremely common conditions in the western world. For example, coronary heart disease (a heart attack) can range from a reversible ischaemic episode to a fatal event if a large part of the myocardium is deprived of oxygenated blood. Anticoagulants are also widely used in dialysis and in heart bypass surgery, and in the aftercare following surgery in general (to prevent deep vein thrombosis, DVT, as a possible consequence of immobility).
The main mode of action of anticoagulants is their ability to reduce the formation of a protein, thrombin, or to block its action. Thrombin, in turn is essential to turn soluble fibrinogen into networks of insoluble fibrin (a main component of a blood clot); reduced thrombin activities thus reduce the formation and growth of venous blood clots. Fibrin is more important in the formation and stability of clots in veins, whereas platelets generally have a more important role in clot formation in arteries.
The two most widely used anticoagulants are heparin and warfarin; both substances have been known for a long time (heparin was discovered over 100 years ago, an early version of warfarin has been known for 80 years).
Heparin in therapeutic doses is commonly used in surgical aftercare, in the form of subcutaneous (under the skin) injections, it cannot be taken orally because the substance cannot be absorbed from the intestines. Heparin is a naturally occurring, large molecule that is also produced in very small quantities by the immune system.
Heparin-induced thrombocytopenia (low levels of platelets)) is a rare (estimated prevalence of 0.1 to 5 percent) but serious adverse reaction to treatment with heparin. It is caused by an immune reaction from antibodies that recognise complexes between heparin and one of the platelet factors (factor 4), leading to unusual blood clotting events. This form of thrombosis is distinct from ‘normal’ (and common) thromboses and is associated with high morbidity (such as loss of a limb) and mortality. The fundamental cause for the unusual immune reaction is not yet known. The condition can be diagnosed with a full blood count, clotting studies and immune assay. Currently the only known treatment is intravenous application of immunoglobulin G. We mention this very rare adverse effect of heparin as it has recently (spring 2021) drawn attention by its similarity to extremely rare unusual blood clotting events in conjunction with thrombocytopenia following COVID-19 vaccination with adenovirus vector-based vaccines.
Derivatives of warfarin are also naturally occurring substances that are produced by some fungi. Warfarin is a small molecule (see Figure 1) and can be taken orally.
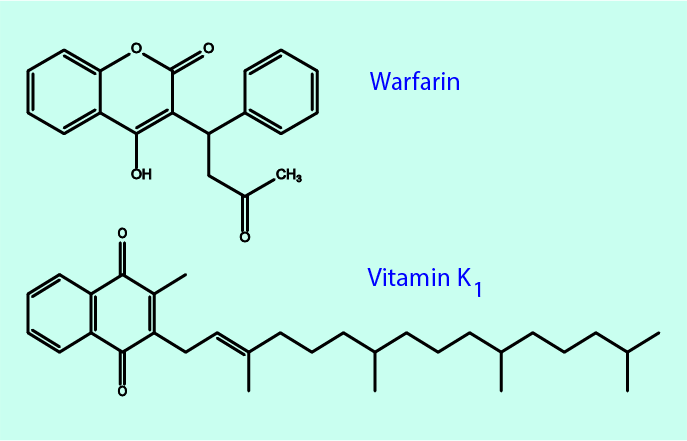
Warfarin is the most widely used anticoagulant, not least because its function can be reversed if necessary. The antidote to warfarin (to stop excessive bleeding) is vitamin K, a vitamin that is necessary in the cascade of blood clotting events. Warfarin inhibits the vitamin-K dependent biosynthesis of several of the blood clotting factors (proteins).
Nature uses anticoagulants in other circumstances too: for example, the saliva of some spiders, snakes, ticks and leeches contains substances with anticoagulant properties. More recent developments of more specific synthetic anticoagulant medications have taken inspiration from these ‘bio-molecules’.
A maxillofacial clinic certainly is not the place for the treatment of cardiovascular conditions. However, a number of maxillofacial patients will be on long-term medication with anticoagulant drugs. This can be relevant for maxillofacial treatment planning and prescription of medications because all anticoagulant (and antiplatelet) medications have in common that they interfere with many other medications and foods, as well as increasing the risk for bleeding.