Pentoxifylline
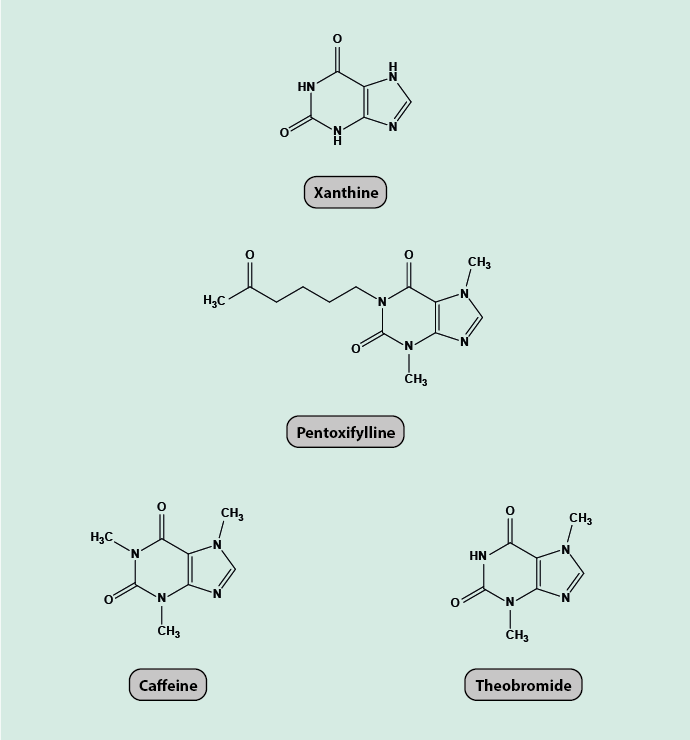
Pentoxifylline belongs to a class of chemicals known as xanthines (Figure 1). A number of xanthine derivatives naturally occur in range of body tissues, some mildly stimulating agents such as caffeine and theobromine (component of chocolate) also belong to this class of chemicals.
The only licensed medical use of pentoxifylline is for the treatment of peripheral arterial disease (intermittent claudication). In clinical dose, the substance has been shown to have effects on the rheology of blood and some properties of platelets and their aggregation behaviours, mainly associated with reduction of the fibrinogen (a protein involved in blood coagulation) concentration in plasma leading to lower blood viscosity. Despite several decades of established use of pentoxifylline to treat peripheral arterial disease, only relatively poor-quality evidence exists supporting this indication.
A number of re-purposing and off-license uses of pentoxifylline continue to be reported. In particular, a broad range of conditions with fibrosis (scarring) of connective tissue as a common feature have been treated with pentoxifylline. This is the area that brings this drug into a degree of relevance to oral and maxillofacial surgery, particularly in relation to osteoradionecrosis.
As stated in a recent review (2016), the molecular biology underlying the various effects associated with pentoxifylline remain murky. The most common explanation points to a role of pentoxifylline as a non-specific inhibitor of the enzyme phosphodiesterase (for example, caffeine is such a non-specific inhibitor). This enzyme is important for the hydrolysis of cAMP (cyclic adenosine monophosphate) to AMP, an important signalling molecule for numerous cellular functions. However, this effect is only observed in vitro at concentrations approximately 1000 times higher than in clinical plasma concentrations. The majority of cell biology experiments on pentoxifylline were all carried out at these unphysiological, high concentrations. Accordingly, any conclusions drawn from such experiments cannot be directly applied to the clinical properties of pentoxifylline (but unfortunately have been quoted as relevant for such circumstances).
Another much quoted effect of pentoxifylline (or its metabolites) is that it lowers the plasma concentration of inflammatory cytokines (messenger molecules), such as TNF-α (tumour necrosis factor α). Again, these observations are based on concentrations higher than those of clinical relevance.
Pentoxifylline is heavily metabolised when ingested or injected, with varied bioavailability for different methods of delivery. Therefore, it may not be unreasonable to ascribe some of the properties of the substance to its metabolites. For example, one of the metabolites (M1) has been shown to inhibit platelet aggregation and to increase blood flow. Such findings suggest that any conclusions drawn about properties and working mechanisms of pentoxifylline would need to consider carefully different forms of administration (oral or intravenous) and dosage, rather than making global conjectures. In addition, obviously the effects of all of the active metabolites would need to be studied, separately and in combination.
In summary, the working principles of pentoxifylline under physiological conditions remain frankly unclear.
We discuss pentoxifylline here because it is one of the three components in the so called ‘triple therapy’ (or PENTOCLO), a controversial medication scheme promoted for the treatment of osteoradionecrosis. Osteoradionecrosis is a severe long-term (lifelong) risk following radiotherapy in the head & neck region. The cocktail of drugs consists of pentoxifylline, tocopherol and clodronate. The argument to include pentoxifylline in the cocktail is based on its assumed anti-inflammatory properties and its known effects on blood rheology. The evidence base about the working principles of this medication scheme and the related hypotheses about the pathology of osteoradionecrosis are conflicted. It is worth mentioning that in the UK the National Institute for Health and Care Excellence (NICE) only recommends PENTOCLO / ‘triple therapy’ for the treatment of osteoradionecrosis of the jaws in the framework of clinical trials but not otherwise.