TORS, trans-oral robotic surgery
The basics of robotic surgery
The motivation underpinning the development of robotic surgery approaches, in head & neck surgery as well as in other surgical specialties, is straightforward. Where a robotic instrument seems well placed to outperform the human hand & eye of a top-performing surgeon, a case can be made to attempt improvements by means of robotics. Improvements could be as varied as reduced operating times, reduced blood loss, shorter recovery periods, improved outcome in terms of disease-free survival in the surgery of malignant tumours, improved quality of life and better functionality after resection (and reconstruction, where applicable).
The means to achieve meaningful such results follow some straightforward design principles. These design principles are best considered as ‘inspired by nature’, a common engineering approach to the design of complicated instrumentation.
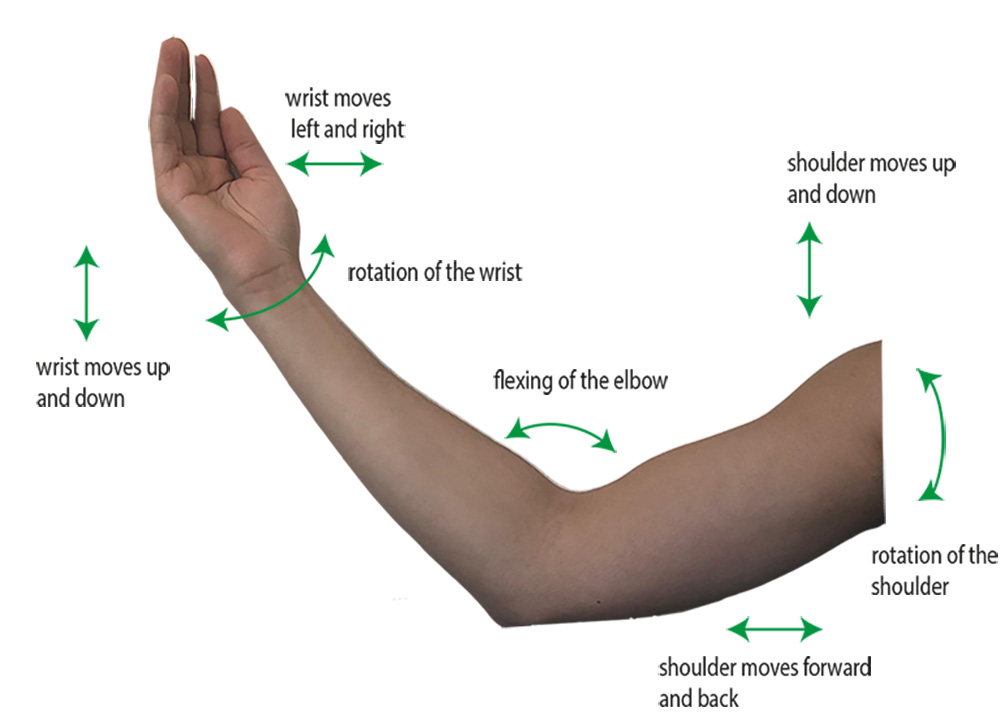
Any instrumentation / tool that has to be capable to carry out complicated manipulations has to take full advantage of the degrees of freedom of movement in the three-dimensional world (Figure 1).

Clever combination of amplitudes, directions and combinations of these types of motions enable every conceivable motion in three-dimensional space. The human arm (Figure 2) is well designed by nature to provide such degrees of motional freedom for the fabulous tool attached to it, the hand. The human arm has a great set of joints and suitable dimensions combined for this enabling purpose.
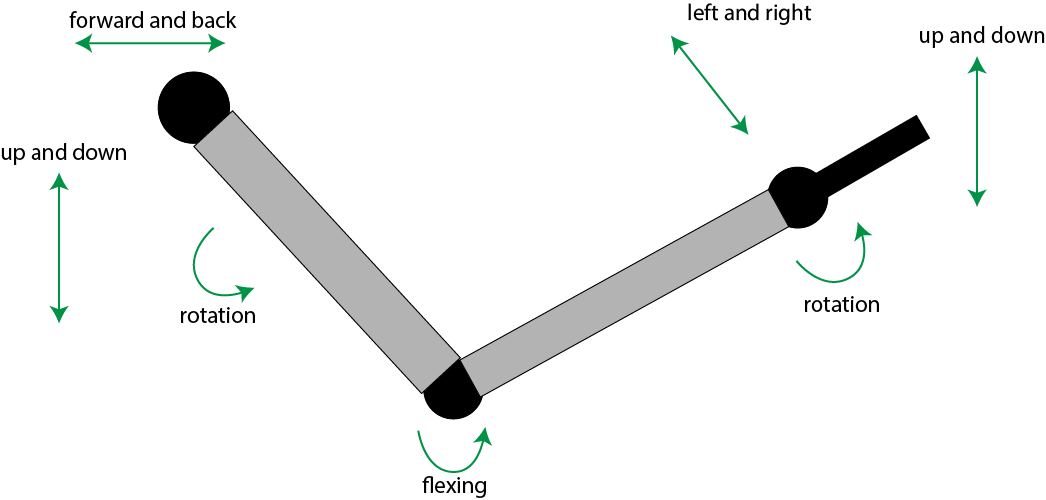
A robotic arm (Figure 3) typically copies these natural design principles to an extent, in order to achieve similar levels of dexterity.
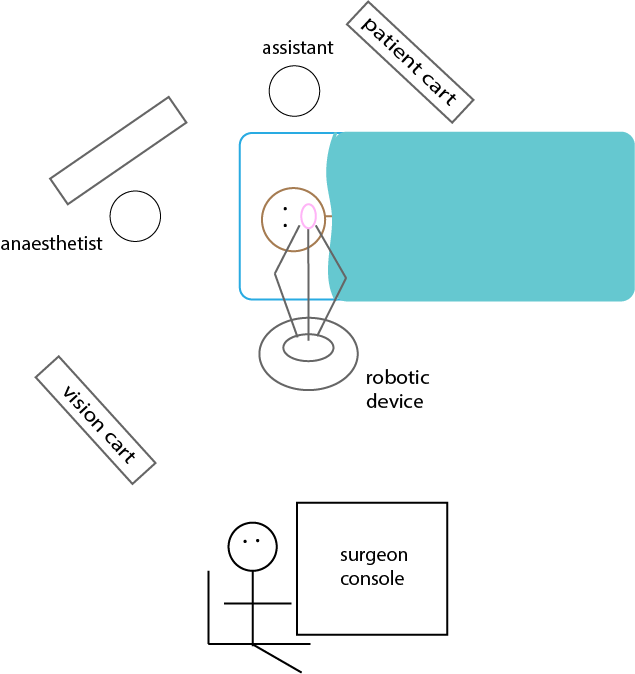
A surgical robot typically is comprised of three robotic arms; one arm equipped with a high-definition three-dimensional imaging camera, the other two arms carrying surgical instruments. The overall surgical set-up has three main components (Figure 4):
- a console for the surgeon to control the robotic arms;
- the robotic devices as such;
- a high-definition, three-dimensional visualisation system.
Different degrees of active / passive control of the devices during surgery can be implemented, from fully programmed robotic operation with little active involvement by the surgeon, to the robotic tools being completely controlled by the surgeon, and variations between these two extremes.
As far as oral and maxillofacial surgery is concerned, potential benefits of transoral robotic surgery (TORS) include
- stable three-dimensional, high-resolution vision of the surgical site;
- transoral access to otherwise difficult-to-access areas;
- improved preservation of functionalities (swallowing and speech);
- reduced morbidities and faster recovery;
- high-precision operation.
Disadvantages of current TORS approaches include
- lack of haptic feedback during surgery, both kinaesthetic and tactile;
- cost and non-optimised soft- and hardware for the requirements of oral and maxillofacial surgery;
- extensive training needs;
- insufficient evidence base for the advantages and disadvantages of TORS for a range of different oral and maxillofacial conditions.
The state of affairs for transoral robotic surgery in oral and maxillofacial surgery in 2019
At the time of writing (2019) transoral robotic surgery (TORS) is not a widely established, or fully evaluated surgical technique in oral and maxillofacial surgery. However, the number of applications is steadily increasing and some (selected) potentially beneficial applications for TORS technology seem to emerge. It should also be noted that the robotic hard- and software used to date was not specifically designed for transoral surgery and employs outdated hard- and software in general. With the advent of robotic designs more suitable for the specific requirements or oral and maxillofacial surgery, the evaluation of potentially beneficial applications of TORS may shift in the future.
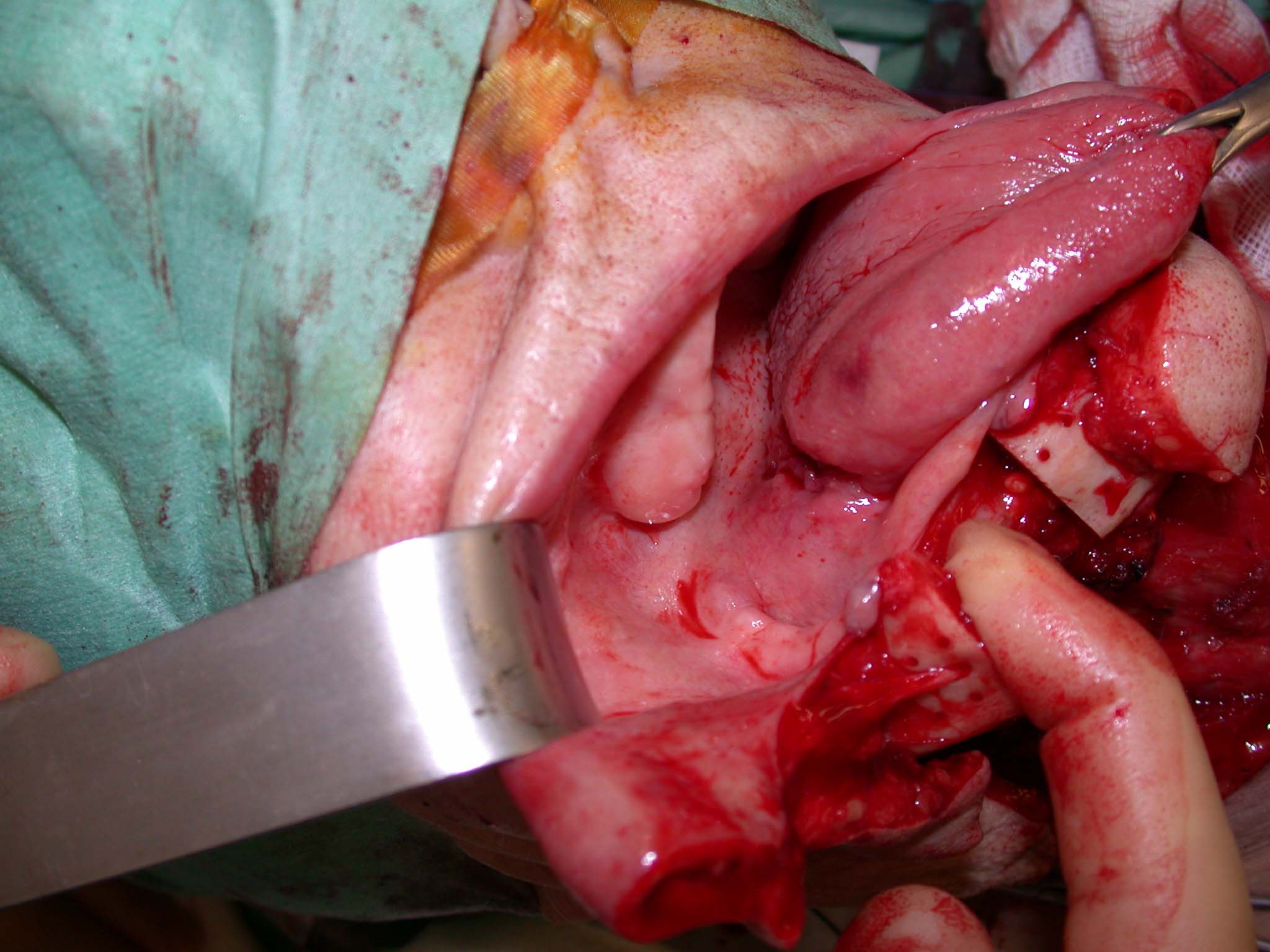
The oropharyngeal region (the region between the soft palate and the back of the root of the tongue, and surrounding areas and structures) is notoriously difficult to access by conventional surgical methods. Slightly restricted access to this area may be possible from the neck, or it may be necessary to create access by a labiomandibulotomy (Figure 5). This approach permits moving the mandible sideways, after splitting lip and mandible, to allow open access. Unfortunately, this access method is associated with serious morbidities in many cases, including dysphagia, impaired speech, fistulae, malocclusion, a range of chronic pain syndromes and disfigurement, resulting in compromised quality of life. It is, therefore, not surprising that surgical interventions in the oropharyngeal region have been identified as candidates for exploration of transoral robotic surgery as an alternative with potential to reduce complications and long-term adverse effects of treatment(s). Another potential application of TORS methodology in hard-to-reach spaces is gaining access to some (metastatic) lymph nodes in the back of the pharynx, an important aspect in the surgery of some oropharyngeal (for example, tonsillar) and thyroid malignancies.
These considerations are true irrespective of resections in the oropharyngeal space to treat primary tumours, or as salvage surgery after recurrence. For large resections, some form of robot-assisted reconstruction may have its merits too.
Further motivation to develop surgical treatment schemes with fewer and less severe morbidities stems from the fact that in particular HPV-positive oropharyngeal malignancies tend to have excellent prognoses. As these tumours tend to afflict younger people, considerations of long-term outcomes, functionalities and quality of life issues have become an even more important aspect of treatment planning. At the other end of the spectrum, with invasive salvage surgery, possible dependency on tube feeding and/or tracheostomy in a palliative setting with limited life expectancy, maintaining as much quality of life for as long as possible is a similarly important consideration.
Unsurprisingly, to date there have been no major randomised controlled trials in oral and maxillofacial surgery to compare TORS approaches with outcomes achieved by conventional treatment protocols; both radiotherapy / chemoradiotherapy schemes and open surgery. An increasing body of literature is beginning to provide reports on smaller-scale evaluations and observations based on consecutive case series with reported long-term outcomes.
There is growing evidence that TORS as the primary treatment modality for early stage oropharyngeal malignancies provides superior functionality and quality-of-life outcomes in comparison with radiotherapy (including intensity modulated radiotherapy schemes), with very similar oncological results. TORS methodology has been shown to reduce the occurrence of positive surgical margins and may be an important stepping stone in so called recent ‘de-intensification’ strategies in the treatment modalities of especially HPV-positive oropharyngeal malignancies in non-smokers. The picture becomes less clear in treatment protocols where postsurgical adjuvant radio- or chemoradiotherapies are necessary. These modalities may well negate the potential benefits of TORS in terms of fewer treatment-related morbidities. Some retrospective studies demonstrate that oncological outcomes and recurrence-free survival periods for HPV-positive as well as HPV-negative oropharyngeal malignancies following primary TORS treatment compares favourably with these results achieved by primary radiotherapy. Accelerated postsurgical recovery and shorter hospital stays have been reported for TORS. Strangely, however, there do not seem to be in-depth studies comparing directly the outcomes of TORS and conventional surgical methods, where these are the only modalities employed.
In summary, the old and often repeated statement ‘more information is needed’ in the conclusions of so many publications definitely applies here. TORS has to demonstrate its merits in properly designed studies (not necessarily trials, due to small numbers) and to live up to the design claims of improved robotic performance over that of the human hand & eye. Even for much better established robotic surgery approaches in other parts of the body, for example in prostate surgery, the evidence in favour of robotic surgical methods is not quite as clear as is sometimes claimed.
Improved hard- and software to make robotic approaches better adapted to manoeuvres in small, dark cavities such as the mouth, in the near future may well shift the goal posts as far as TORS is concerned. A considerate judgment of the merits of TORS also needs to take into accounts the immense costs associated, in terms of hardware purchase and hardware maintenance as well as in terms of extensive training needs. The latter is not a negligible quantity as it includes not only learning steps to use hard- and software of any robotic tools, it also requires a re-learning of anatomy in an inside => out way, as opposed to the normal outside => in anatomy concept of a surgeon.