Broken bone
Fracture
Fractures are caused by accidents and trauma in general. Trauma is a leading cause of death and disability particularly in the young. One of the real advances in health care over the last 25 years has been the standardised approach to severe trauma, originally modelled on the American College of Surgeons Advanced Trauma Life Support (ATLS) principles. While there are some variations worldwide, this system allows everyone who has been trained in it to ‘speak the same language’ in establishing priorities in both identifying and simultaneously treating acute life threating injuries.
For that reason this section first concentrates on that general trauma-care system. Later on we describe some of the specialist techniques in maxillofacial trauma that are either adjuncts to ATLS or relevant to maxillofacial trauma in the acute setting (much of it can be handled semi-urgently).
Principles of trauma care (Advanced Trauma Life Support, ATLS)
Modern trauma resuscitation is based on the Advanced Trauma Life Support course for doctors (ATLS), devised and updated by the American College of Surgeons Committee on Trauma. This system has established an accepted international reputation as the gold standard for trauma resuscitation.
It follows a logical sequence of care which is designed to maximise the efficiency of assessment of the trauma victim, as well as provide priority ranking of potential, life threatening problems and simultaneous resuscitative interventions. The sequence of ATLS is as follows:
Preparation
This is divided into a pre-hospital phase essentially limited to first aid in the field of injury. A matching system for paramedics and field physicians exists (Pre-Hospital Trauma Life Support; PHTLS). Triage, which is a sorting of patients based on the urgency of need of treatment and the available resources to provide that treatment, may be carried out both pre-hospital or in hospital. This is based on the principle that the most severely injured patient requires the more urgent treatment, and the less injured patient can receive treatment after a slight delay using the ABC’s described below.
The second phase of preparation is the in-hospital phase in which the patient has been brought to the hospital where he/she can be managed according to the extent of injury.
Primary survey
This is the rapid but thorough assessment of patient treatment priorities based on their injuries, their vital signs and the injury mechanism. It follows the ABC's of trauma care and identifies life-threatening conditions by adhering to the sequence:
A - Airway maintenance with cervical spine protection.
B - Breathing and ventilation with maximum flow oxygen.
C - Circulation with haemorrhage control.
D - Disability; neurological status assessment.
E - Exposure/environment control, completely undressed patient but hypothermia prevented.
A – Airway maintenance with cervical spine protection
After ensuring personal safety, the airway is assessed by looking, listening and feeling for air movement. Grunting, snoring or absence of breath indicates an obstructed airway. Talking, swearing or screaming, conversely indicates a patent airway. This rapid assessment should include inspection for foreign bodies and facial, mandibular or tracheal/laryngeal fractures that may result in airway obstruction.
Measures to establish a patent airway, if needed, should be instituted while protecting the cervical spine (loss of airway kills fastest but creating a quadriplegic in the process does not help the patient). Initially manually clearing the airway and the chin lift or jaw thrust manoeuvre (see below) is recommended, and may be reinforced in the unconscious patient with an oral airway or, in the rousable patient, a nasopharyngeal airway. These airway adjuncts do not secure the airway (that requires a secured, cuffed tube in the trachea) but may be adequate until a secure airway can be safely achieved by nasal, oral or surgical intubation. A reduced level of consciousness or blunt injury above the clavicle (collar bone), in a polytrauma patient (a patient with multiple injuries) carries a 10% risk of cervical spine injury. Immobilisation in the neutral position minimises the risk of further morbidity.
B – Breathing and ventilation
Airway patency alone does not ensure adequate ventilation: adequate gas exchange is required to maximise blood oxygenation and carbon dioxide elimination. Ventilation requires adequate function of the lungs, chest wall and diaphragm. Each component must be examined and evaluated rapidly. If the patient is not breathing adequately, immediately remediable problems e.g. tension pneumothorax (collapsed lung), displaced tube or cardiac tamponade are addressed. If there is no effort or adequate effort at self-ventilation then manual or mechanical ventilation must be started. High flow oxygen needs to be given in any case (with reservoir bag if by facemask).
C – Circulation with haemorrhage control
Obvious external bleeding is stopped by direct pressure. Two wide-bore intravenous cannulae are established, to take blood and give a fluid challenge (2 litres of warmed Hartmann’s solution (solution of sodium, potassium and calcium chloride, plus sodium lactate). Ringer’s solution (sodium lactate solution) and normal saline (sodium chloride solution) are more commonly quoted than Hartmann’s in the US).
Pulse, respiratory rate and blood pressure are monitored. All trauma shock is initially managed as haemorrhagic shock until proven otherwise. Possible bleeding in the chest, abdomen and pelvis are explored. In the case of maxillofacial trauma, fractures of the midface (Le Fort I, II and III) can lead to torrential haemorrhage and, rarely, immediate specialist maxillofacial resuscitation is needed (see below).
Despite the evidence, particularly from recent warfare experiences and in common use in UK emergency departments, giving tranexamic acid (medication to stop or prevent bleeding) as an infusion has not yet translated into ATLS protocols.
D – Disability and neurological evaluation
A rapid neurological evaluation is performed to assess the patient's level of consciousness, pupillary size and reaction. The Glasgow Coma Score is the international gold standard.
E - Exposure/environment control
Special effort must be made to avoid the patient developing hypothermia during the early stages of trauma care. Exposure (removing clothing to ensure no other injury is missed) is carried out in a warmed environment.
Secondary survey
This does not begin until the primary survey (ABCDE) is completed, resuscitation has been successful, and the patient is demonstrating normalisation of vital functions. It is essentially a head to toe evaluation which looks at head injury, cervical spine and neck injury, chest injury, abdominal injury, perineum and rectal/vaginal injury, musculoskeletal injury, peripheral neurological injury and also maxillofacial injury. Assessment of maxillofacial trauma is part of the secondary survey when it is not compromising the airway or leading to significant haemorrhage. If the maxillofacial trauma is compromising the patient’s airway or causing significant haemorrhage, then this is noted in the primary survey and acted upon. Many lives have been saved by health care workers who have stuck rigidly to this tried and tested methodology.
Specialist maxillofacial resuscitative techniques
This is initially based on airway preservation and adequate ventilation in order to maintain oxygenation and prevent hypoxia (decreased partial pressure of oxygen) and hypercarbia (increased partial pressure of carbon dioxide). These factors are critical in managing the trauma patient, especially if a head injury has been sustained. Maxillofacial trauma demands aggressive airway management. High impact trauma to the mid face produces fractures with displacement and oedema which will obstruct the nasopharynx, oropharynx and hypopharynx. Facial fractures may be associated with haemorrhage, increased secretions and dislodged teeth causing additional problems in maintaining a patent airway. Fractures of the mandible, especially bilateral body fractures may cause loss of normal tongue support, leading to the tongue falling backwards and blocking the airway. Airway obstruction can also result as post-traumatic oedema develops rapidly. The problem can be exacerbated if the patient is in a supine position (lying on the back; the position favoured in ATLS resuscitation) because secretions, blood and the abnormally heavy tongue can fall to the back of the mouth.
A patient’s refusal to lie down may be demonstrating difficulty in maintaining their airway or handling secretions. This should not be presumed to be uncooperative in the first instance. This creates a dichotomy between allowing the patient to maintain their own airway in an upright position and securing the airway in the supine position. Common sense, in conjunction with clinical judgement and proceeding are the solution.
Airway maintenance techniques
Even in non-trauma patients with decreased consciousness the tongue may fall backwards and obstruct the hypopharynx. This form of obstruction can be corrected by a chin lift or jaw thrust manoeuvre. The airway can then be maintained with an oropharyngeal or nasopharyngeal airway. These manoeuvres must always be done with in-line immobilisation of the cervical spine if the cervical spine has not yet been cleared of any injury by clinical and radiological methods and an appropriately trained individual.
Chin lift: the fingers of one hand are placed under the mandible which is gently lifted upward to bring the chin forward, while the thumb of the same hand lightly depresses the lower lip to open the mouth. The thumb may be placed behind the lower incisors to help pull the chin forward. The chin lift manoeuvre should not hyperextend the neck. This manoeuvre is useful for the trauma victim because it does not risk compromising a possible cervical spine fracture or converting a fracture without cord injury into one with cord injury.
Jaw thrust manoeuvre: this is performed by grasping the angle of the mandible, one hand on each side and displacing the mandible forward. When this method is used with the facemask or an anaesthetic bag valve device, a good seal and adequate ventilation can be achieved.
Oropharyngeal airway: an oral airway is inserted into the mouth behind the tongue. The preferred technique is to insert the tube upside down and then rotate it over the back of the tongue. The device lifts the tongue forward off the hypopharynx and allows air to pass through the lumen of the oropharyngeal airway.
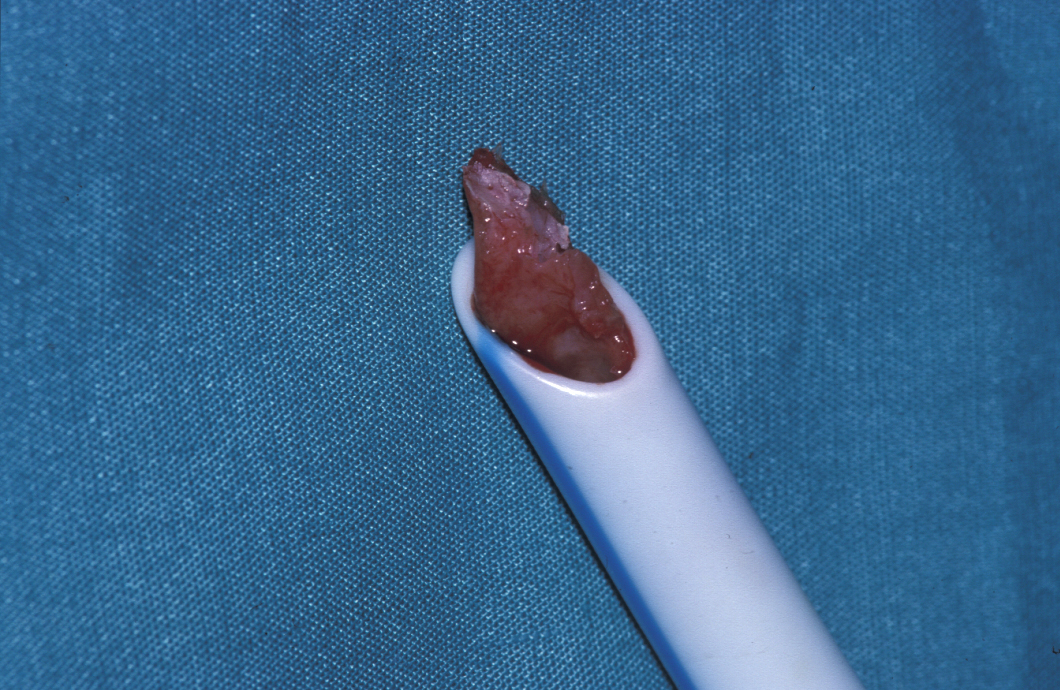
Nasopharyngeal airway: this is inserted into one nostril and passed into the posterior nasopharynx. Beware obstruction of this (or any) tube (see Figure 1). This airway is better tolerated in the conscious patient.
Needle cricothyroidotomy: there are common misconceptions about this technique. It does NOT secure the airway. It does maintain some form of airway which can allow insufflation of the lungs and preserve life for about 30 mins, until a secure airway (below) is achieved. It is performed by inserting a wide bore intravenous cannula (12 or 14 gauge) through the cricothyroid membrane (above cricoid cartilage and below thyroid cartilage). Aspiration confirms if it is in the trachea. It is next connected to oxygen at 12-15 L/min via a Y connector or by cutting a hole in the tubing. Occluding the hole for 1 sec allows to “inflate” the lung, then turning the oxygen off for 4 sec allows the lung to deflate.
These are all merely temporary airway maintenance techniques and do not represent a definitive airway. A secure airway has not been obtained until an endo-tracheal tube has been placed with the cuff inflated and the tube secured. The tube is connected to some form of high flow oxygen (12-15 L/min). If a patient has difficulty in breathing either mechanical obstructions (pneumothorax, tamponade) need to be removed or assisted ventilation (Ambu bag, ventilator) provided.
Definitive airways
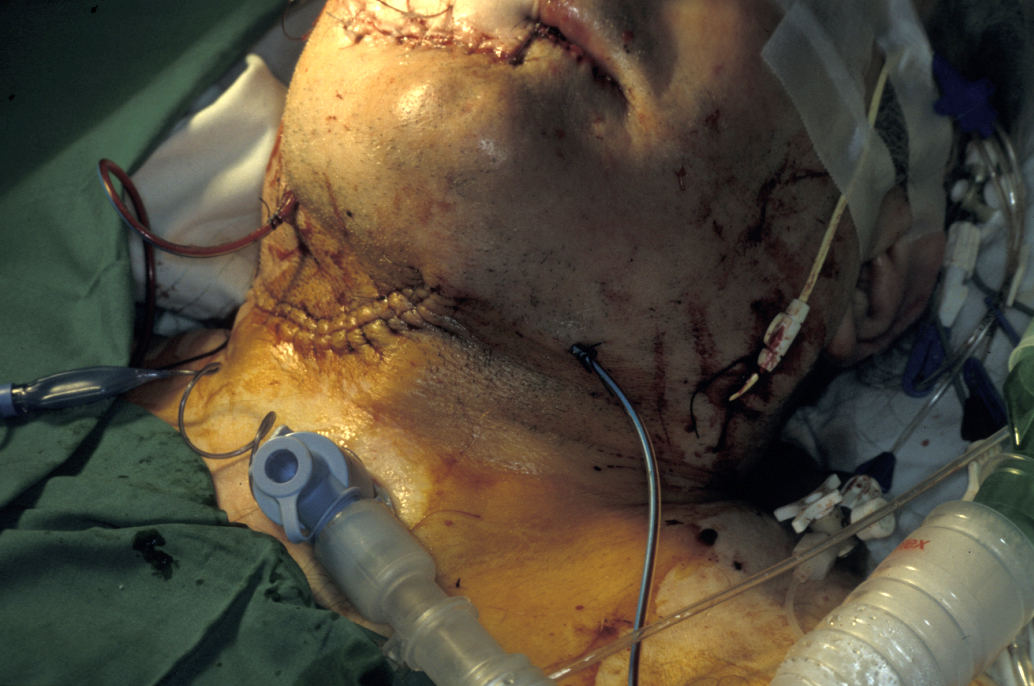
These are of three varieties: orotracheal tube, nasotracheal tube, and surgical airway (cricothyroidotomy or tracheostomy; see Figure 2).
A definitive airway is required if the patient is going to undergo surgical correction of facial fractures and have treatment of other associated injuries. It is also indicated if the patient is destined to spend a long time recovering from head injury, or requires a prolonged period of artificial ventilation in an intensive care unit. Orotracheal and nasotracheal intubation are specialised techniques, best performed by those trained and experienced in them. Hypoxia can result while inexperienced personnel attempt to place these tubes.
Cricothyroidotomy: this is an emergency procedure and can be done in the field, accident and emergency setting, or ward setting as long as the surgeon has the ability to perform the procedure. This involves making a cut through the skin and the cricothyroid membrane and introducing a cuffed tracheostomy tube (size 6) into the trachea to allow oxygen delivery.
Tracheostomy: this is not an ‘emergency’ surgical airway and should not be done in the acute trauma airway emergency setting. It requires controlled operating theatre equipment and lighting to ensure a successful procedure. It takes longer and involves displacement or incision of more structures. Tracheostomy involves incising the skin, dissecting fat to expose the strap muscles and separating them. The thyroid gland is identified and either displaced or the isthmus (part of the thyroid gland) ligated and divided. A hole in the trachea in the region of the second to fourth cartilaginous rings is created either as a slit (in children) or by cutting out a circle of trachea or creating an inferiorly based flap (Bjork flap) and passing a tube into the tracheal lumen.
End tracheostomy is the stoma created when a laryngectomy is performed and is quite different from these temporary airway operations.
Specific maxillofacial emergencies
Laryngeal injuries
The larynx is a semi-rigid structure made up of the hyoid and several cartilages interconnected by fibrous tissue. This framework is lined by mucosa, which can become grossly swollen following injury. In young patients, the larynx is elastic and tends to flex and spring back to its normal position rather than fracture following traumas. The epiglottis may become avulsed. In older patients the cartilages become calcified and fractures are more likely. Rarely the trachea can be avulsed. This is usually fatal at the time of injury.
Flow varies according to Poiseuille’s law (flow is proportional to the radius of tube to the power of 4), which means that only small changes in the radius are necessary to significantly affect the flow of air through it. This is seen particularly after thermal inhalation where oedema of the whole upper respiratory tract results in rapid reductions in airflow. Early intubation is often necessary.
Causes of obstruction include:
Blunt injuries
- Road traffic accidents.
- Sports (e.g. contact sports, martial arts)
- Assaults
Penetrating injuries
- Knife wounds
- Firearms
- Shrapnel (including human body parts common with improvised explosive dvices or suicide bombs)
Thermal injuries
- Inhalation of smoke, hot air or steam
- Blast injury
Clinical features include:
- Dyspnoea
- Stridor (high-pitched breathing sound)
- Pain
- Localised tenderness
- Hoarse voice
- Dysphagia
- Surgical emphysema
- Displacement of the larynx
Management
Rapid identification is essential as patients can quickly deteriorate if the airway is not secured. This is particularly the case in burns victims. With minor injuries, humidified air and steroids may be all that is required. However, these patients must be kept under close observation and frequently reassessed. Major disruption needs the airway securing. This can be done either by intubation, cricothyroidotomy or tracheostomy. Surgical repair may be required in:
- Tracheal injuries.
- Laryngeal displacement or disruption.
- Excessive swelling of the laryngeal soft tissues.
- Most cases of surgical emphysema.
Vision threatening injuries
Eye injuries are commonly associated with damage to the upper midface; in some studies up to 90% of patients had some form of ocular injury. However, in the vast majority of cases these are relatively minor and require no treatment. The term vision threatening injuries refers to those injuries which, if untreated, rapidly result in loss of sight. These are relatively rare but are reported in up to 10% of patients who have had “significant” facial injuries (panfacial injuries, high velocity injuries, gunshot wounds).
The three common vision threatening injuries are:
- Retrobulbar haemorrhage (now considered part of orbital compartment syndrome).
- Penetrating ocular injuries.
- Optic nerve compression.
Diagnosis is usually straight forward but these can be missed in the unconscious or uncooperative patient. The eye must be inspected but care must be taken not to press on the globe in case there is a penetrating injury. Visual-evoked potential is an experimental method of evaluating the visual pathways which has shown much promise. However, it does not identify any specific causes.
Retrobulbar haemorrhage (orbital compartment syndrome caused by bleeding): Bleeding and gross swelling behind the eye may occur following trauma (or surgery) to the orbit, which is effectively a rigid, closed “box”, with the globe forming one of its “walls”. Any swelling will therefore result in raised pressure behind the eye, resulting in compression and spasm of the ciliary vessels. In addition, the eye itself becomes pushed forward (proptosed). This combination results in compressive effects on the vasa nervorum of the optic nerve, creating direct neurological damage which can quickly become irreversible. Retrobulbar haemorrhage is rare, with a reported incidence of around 0.3%. It commonly occurs within a few hours of the injury, although cases presenting up to five days following injury have been reported.
Signs may include:
- Proptosis
- Opthalmoplegia
- Chemosis and pain
- Relative afferent papillary defect (RAPD; this can indicate either optic nerve or severe retinal disease)
- Papilloedema
- Raised intraocular pressure
- Lack of central retinal artery pulsation
- Pale optic disc (late sign)
- Cherry red macula.
Blindness is believed to occur due to spasm of the optic and retinal blood supply secondary to a high tamponade pressure, the difference between this condition and the “benign” retrobulbar bleeding seen in 2% of cataract extractions is thought to be due to location and tamponade pressure.
Retrobulbar haemorrhage requires immediate surgical decompression if vision is to be restored. This simply involves removal of all sutures in the area in operated patients. In trauma patients who have not yet been operated on, an incision around the eyelid is made to allow access to the lateral canthal ligament (an area of denser fascia). This is incised and released to allow blunt dissection, passing behind the periorbita to enable decompression of the haematoma.
When unavoidable delays in surgery are present, short term measures include:
- Dexamethasone, 8mg intravenously
- Acetazolamide (carbonic anhydrase inhibitor, reduces production of aqueous humour) 500 mg intravenously and then 1000mg orally over 24 hours
- Mannitol 100 ml 20% infusion (doses for standard 70kg adult without medical contraindications)
- Lateral canthotomy and cantholysis – this involves division of one of the supporting ligaments attaching the eyelids to the orbital rim. It can be carried out under local anaesthesia. This provides a little “breathing space” by allowing the eye to pop forward and reduce the pressure in the orbit.
Optic nerve compression: displaced fractures which involve the orbital apex (panfacial, skull fractures) can sometimes press on the optic nerve. Often those structures passing through the superior orbital fissure are also traumatised, resulting in the orbital apex syndrome. The management for this is controversial and involves either surgical decompression or high dose steroids. In cases where there is direct impingement of the optic nerve by bone or other penetrating fragments, removal of these rarely results in an improvement in visual acuity. In cases where there is no identifiable hard tissue, surgery can be positively harmful and medical reduction of swelling is more appropriate.
Penetrating Neck Injuries
These are often very dramatic in appearance, but in many cases may miss vital structures. Penetrating injuries deep to the platysma muscle (a superficial muscle in the front of the neck) should not be explored under local anaesthesia in an emergency room setting.
When assessing patients with neck wounds, the following structures need to be considered, depending on the point of entry and direction.:
- Major vessels (carotid artery, internal jugular vein)
- Lung apex
- Upper airway
- Oesophagus
- Vagus nerve
- Phrenic nerve
- Thyroid gland
All penetrating foreign bodies should be left in situ until the patient is anaesthetised and has secure intravenous access. Surgical removal can be then undertaken in an operating theatre. Generally this is by directly reversing the path of insertion but with wide visualisation and access to surrounding vital structures.
Specialist maxillofacial techniques for arresting haemorrhage
There are a small number of cases when exsanguinating haemorrhage from facial fractures requires direct intervention in the primary survey. It is usually due to bleeding from the nose or maxillary fractures.
Nasal bleeding can be dealt with by bilateral anterior and posterior nasal packing, using specially designed inflatable catheters (Brighton balloons, Epitek catheters, Rapid Rhino) or urinary catheters in the postnasal space with a conventional anterior nasal packing.
Bleeding from the maxilla can be arrested by manual reduction and immobilisation with a conventional dental rubber mouth prop.
Temporary splinting of open fractures can be achieved with the ‘bridle wire’, which is a direct wire ligature passed around teeth on either side of a fracture and tightened by twisting clockwise.