Facial appearance
Below we discuss in a little more detail the background to some commonly performed procedures in purely aesthetic facial surgery:
- rhytidectomy (face lift, of which there are many different varieties)
- blepharoplasty (addressing puffy or sagging upper and/or lower eyelids, related: brow lift)
- otoplasty (improving the appearance of prominent ears (‘bat ears’))
- rhinoplasty (a range of corrections to the nose)
- genioplasty (movement or reshaping of the chin)
- miscellaneous procedures.
Rhytidectomy
Rhytidectomy, or facelift, addresses the sagging skin and wrinkles of ageing. The elasticity of skin diminishes with age as collagen weakens. Collagen is the main stabilising and structure providing protein component in tissues such as tendons or skin. A facelift does not restore the collagen production in an ageing body to that of a young body but it can make the visible effects of weakening collagen less visible, at least temporarily.
The areas of the face addressed by rhytidectomy are essentially the lateral (side) face and neck (jowl), bilaterally extending to the cervical (neck) midline. Cervicofacial (neck & face) rhytidectomy is considered one operation, but it can be separated into its neck and face components. A facelift is often a two-part procedure:
- one for the lower face and jowls,
- one for the midface.
The upper face, less commonly discussed, also needs to be addressed.
A stable successful rhytidectomy should be directed towards deeper connective tissue layers as well as skin. A skin-only facelift may relapse in as short a time as six months.
There are probably more variations on the ‘facelift’ than on any other single procedure with a principal single outcome. The operation ranges from endoscopic through minimally invasive, mini to deep plane and subperiosteal (situated under the periosteum, the connective tissue enveloping bones) lifts. The most common tried and tested approaches are the classical skin-only lift (‘mini facelift’, which does not address the temporal (temple) region or the platysma (broad sheet of muscle stretching from the collarbone to beneath the jaws)) and the SMAS lift.
The superficial muscular aponeurotic system (SMAS) is a subcutaneous (under the skin) tissue. Its sagging and ageing causes the skin to sag and slacken as well. A SMAS lift addresses the lower part of the face and aims to reduce the visible effects of sagging in the midface, loose skin and fat (under the chin and jaws), hollow cheeks. A SMAS lift greatly reduces relapse by providing a robust component that can be fixed in a less temporary fashion than a skin-only facelift. A large area addressed by rhytidectomy is the neck, and platysmal plication (tucking and tightening of the platysma muscle) may be performed at the same time.
Blepharoplasty
Puffy or sagging eyelids are common complaints. Accurate diagnosis is essential. The complaint of sagging upper eyelids is often due to sagging of the eyebrows as opposed to excess tissue in the upper lid. In this situation the treatment is a brow lift first (see below) and then possibly an upper blepharoplasty. In assessing the lids, the appearance of bagginess may be due to skin or fat or both. The word blepharoplasty was first used by Karl Ferdinand von Gräfe (a surgeon from Warsaw, pioneering plastic and reconstructive surgery) in 1818 to describe a procedure for repairing defects in the eyelids secondary to tumour excision.
The eyelids are one of the first structures of the face to develop structural changes due to ageing. Ageing results in changes in elasticity of the orbital septum, the tarsus and the orbicularis muscle. Clinically the loss of elasticity of these components of/near the eyelid leads to excess skin, wrinkles, pseudo-herniation of orbital fat, baggy and tired looking eyes. Changes in the skin are further characterised by development of pigmentary anomalies. Because skin quality is not altered by blepharoplasty, adjunctive therapies such as dermabrasion, chemical peeling or laser skin resurfacing may need to be incorporated into rejuvenation strategies (see below). Blepharoplasty will not on its own treat malar bags (swollen pads between lower eyelids and upper cheek) or the tear trough deformity (deep hollow under the eyes).
Lower lid blepharoplasty
The formation of bags under the eyes has more to do with problems with periorbital (around the eye) fat than skin. If fat requires removal this should be minimal and is achieved as much by diathermy to make it shrink as by excision. Excessive fat removal can lead to a sunken appearance, which is difficult to correct. Skin removal should be minimal.
Upper lid blepharoplasty
In contrast to the lower lids, upper lid bagginess is largely due to excess skin (although see brow lift below). An assessment as to the amount to remove may be made by pinching the skin of the lid until the eye starts to open. This is the minimum that should be removed. In addition to skin removal a small amount of muscle may need to be removed. As with the lower lids there may be a small amount of fat herniation which may require reduction but there is no lateral fat pad (this is the lacrimal gland and it should be left well alone).
Brow lift
The eyebrows may become ptotic (drooping) with age resulting in lateral crow’s feet and hooding with concomitant overactivity of the forehead musculature with rhytid (wrinkle) formation. The brow lift aims to address this. There are several brow lift techniques the choice of which is determined, largely, by the height of the forehead. The distance between the upper edge of the eyebrows and the hairline should be approximately 5 cm. This may be lengthened or shortened by a particular brow lift, and this should be borne in mind when planning.
Otoplasty (pinnaplasty)
The arterial blood supply of the ear arises from the superficial temporal and the posterior auricular arteries. Its sensory supply is from the auriculotemporal, great auricular and vagus nerves. The auricle (the visible part of the outer ear, also referred to as pinna) is fully formed at birth. It reaches 85 % of its final size by the age of three and is virtually adult size by six years.
Bat ears can be a source of misery for children due to teasing at school.
They are characterised by an excessive angle between the pinna and the skull, congenital absence of an antihelix (part of the pinna, a stretch of cartilage) or a combination of both. Again proper evaluation of the exact problem is required. The problem may be caused by the pinna with an absence of an antihelix, or the conchal bowl (bowl-shaped inner part of the outer ear) creating an excessive concho-occipital angle (angle with the lower back part of the skull).
There is a variety of surgical techniques to address problems with prominent ears.
Rhinoplasty
Rhinoplasty is one of the most demanding techniques in aesthetic surgery. As with all of the topics discussed in this section, evaluation of the problem is critical. The nose consists of skin, fibro-fatty connective tissue, hyaline cartilage and bone. As a rule, rhinoplasty can address problems related to cartilage and bone but it cannot alter the skin of the nose, which can vary from paper thin to thick and fleshy with many sebaceous glands.
The nose should be assessed with a view to maintaining the aesthetic balance and characteristics of the face. For example, mandibular retrognathism (a too small lower jaw) may make a perfectly acceptable nose appear large, but this will be in proportion following a mandibular advancement procedure.
The nose should be examined from all angles including above and below. The various components to assess are tip projection, supra tip break, dorsal hump, nostril symmetry, septal deviation and skin quality.
There are vast arrays of incisions that may be used in performing a rhinoplasty; however, there are essentially two approaches, open or closed. The closed approach remains the most popular and involves intranasal incisions. An open rhinoplasty will leave a small scar across the columella (tissue that separates the nostrils), a closed rhinoplasty will not.
If the nasal tip needs to be addressed this can mean
- increasing of the tip projection,
- decreasing of the tip projection,
- increasing of the tip rotation,
- decreasing of the tip rotation.
Genioplasty (movement or reshaping of the chin)
Genioplasty is movement of, or reshaping, of the chin. There are a number of approaches to this operation, usually depending on the training of the surgeon. Conventional genioplasty is an orthognathic procedure. Genioplasty may aim to reduce or augment the bulk of the chin, or to correct asymmetries.
Variations on the advancement genioplasty have become popular in the treatment of obstructive sleep apnoea. The concept has an evidence base and relies on the advancement of the genial attachments of the tongue musculature.
Augmentation genioplasty by implants is used by some surgeons. This may involve synthetic materials as implants (silicone elastomers, coral (as a substitute for a bone graft) and other synthetic materials) or the patient’s own bone. Almost inevitably, the aesthetic result using the patient’s own bone is superior to that using synthetic materials.
Miscellaneous procedures and conditions
Facial rejuvenation destroys the very superficial layer of the skin (‘chemical peeling’; different chemical agents will affect the skin to different depths). This can be carried out using chemicals such as glycolic acid, trichloroacetic acid or phenol. A similar effect can be achieved with a CO2 laser. After healing the finer rhytids (wrinkles) will have disappeared.
Dermabrasion works in much the same way as the rejuvenation procedures but uses a large bur to smooth rough areas of skin or scarring. It is particularly useful for severe skin damage such as the results of bad acne.
Fillers such as collagen and hyaluronidase solutions, sometimes combined with local analgesia are used to fill out subcutaneous hollows, either deep such as the nasolabial folds (‘smile lines’), or tiny such as labial rhytids (multiple small wrinkles around the lips). Sometimes a temporary solution to traumatic or acne scarring.
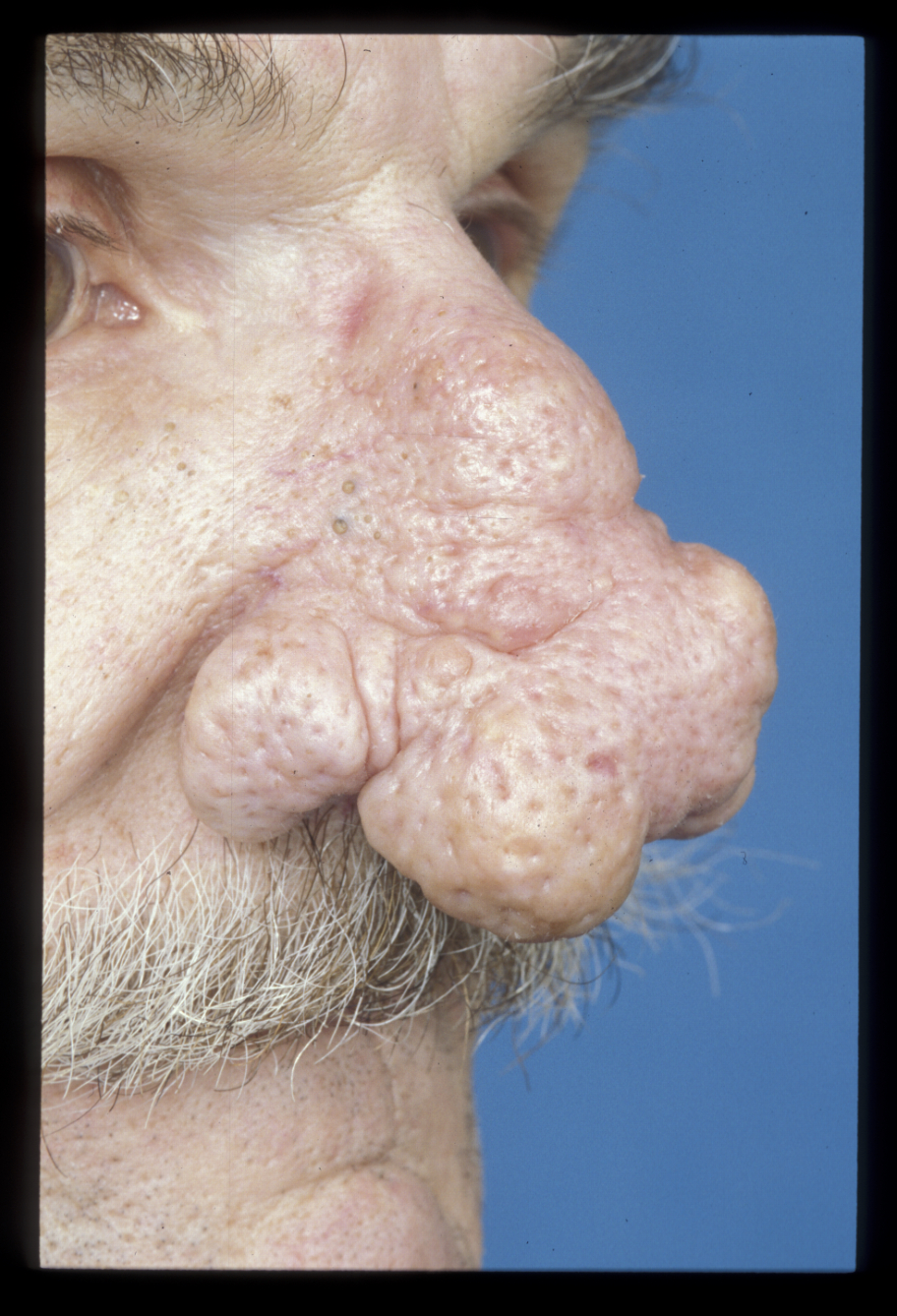
Rhinophyma is a condition caused by an overgrowth of sebaceous glands in the nasal skin (see Figure 1). The perception that it is due to excessive alcohol intake is erroneous. It can be quite dramatic in appearance but is relatively easily treated. The tissue can either be excised or dermabraded (see above). Mechanical removal may be used in conjunction with a CO2 laser. The tissue should be sent for histology as basal cell carcinoma may mimic benign rhinophyma.
Botulinum alpha toxin prevents acetylcholine release at the neuromuscular junction, paralysing the muscle. Its use is widespread, particularly for the treatment of rhytids. Rhytids are formed at right angles to the direction of pull of the underlying musculature. Paralysis of these muscles with botulinum toxin decreases the wrinkling present and can prevent future rhytid formation.
The botulinum alpha toxin solution is injected into the muscles in the affected area, most commonly the forehead, the glabella, and the crow’s feet. In the forehead, the injection should be at least 1 cm above the eyebrow to prevent unwanted ptosis (sagging of the eyebrow). The injection sites should not be massaged as this makes the solution dissipate unpredictably. The patients (or clients) should remain upright for 4 hours and not undertake strenuous exercise that day. Otherwise, it is a remarkably safe procedure. The effect can be variable but will usually last six months to a year. Repeated injections over time may have a more permanent effect. Paralysis of facial muscles is a potential unwanted effect.
Botulinum alpha toxin also is useful in treating bleopharospasm (involuntary twitching or contraction of the eyelid, masseteric hypertrophy (enlargement of the masseter (cheek) muscle; see Figure 2), temporalis hypertrophy (painful enlargement of the temporalis (chewing) muscle leading to soft tissue swelling of the temple; see Figure 3) and Frey’s syndrome (redness and sweating on the cheek in conjunction with eating / salivation; usually an unwanted effect of surgery of or near the parotid gland).

