Botulinum toxin alpha
Botulinum toxin is a highly poisonous substance. It is produced by a commonly occurring bacterium, clostridium botulinum (a Gram-positive, anaerobic rod). Botulinum toxin is a powerful paralytic neurotoxin. There are several different types of botulinum toxin but the one most commonly used for medical purposes is botulinum toxin alpha (sometimes called botulinum toxin A).
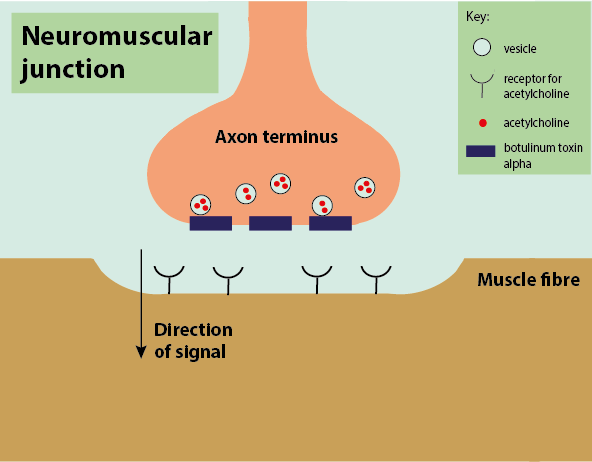
All botulinum toxins work by inhibiting the release of the ubiquitous neurotransmitter acetylcholine. Acetylcholine is an excitatory neurotransmitter that works at the neuromuscular junction. When acetylcholine is released by motor neurons, it activates the muscle. When acetylcholine is blocked, the muscle cannot be activated, so the muscle is paralysed (Figure 1). The main mechanism by which botulinum toxins block acetylcholine is by preventing its release from the vesicles at the neuronal endings.
Botulinum toxin also reduces or inhibits the release of inflammatory mediators such as calcitonin gene-related peptide (CGRP; a potent peptide acting as a vasodilator and involved in nociception (pain sensation); CGRP is thought to have role in in the pathophysiology of migraine), glutamate and substance P (another neurotransmitter peptide). This effect of botulinum toxin is likely to be due to its inhibitory action on both voltage-gated sodium and calcium channels in nerve endings. In this way it influences pain transmitters in both peripheral and central nervous system sites, and is also thought to cause an increase in GABA (γ-aminobutyric acid, an inhibitory neurotransmitter) release.
Botulinum toxin has many medicinal uses, including applications in the maxillofacial surgery context. Generally, it is probably best known for its cosmetic uses, such as reducing the appearance of lines and wrinkles (‘chemical facelift’, ‘botox’) all over face, chin and neck. For this temporary ‘fix’ to work, precise understanding of the anatomy of the mimetic muscles in the face and neck region is essential. Botulinum toxin is administered locally by injection(s) to the target muscle(s) or gland(s).
Botulinum toxin plays a significant role in the management of a many different conditions, including:
- strabismus (problems with coordination and synchronisation of eye movements; this was historically the first medical application of botulinum toxin);
- blepharospasm (involuntary tight closure of eyelids);
- dystonias (neurological movement disorders, affecting movement of the mandible (lower jaw) and temporomandibular joint (jaw joint), causing trismus (restricted mouth opening));
- spasticity (muscles continuously contracting causing painful stiffness and tightness; for example, hemifacial spasms, or spasms of neck muscles following radiotherapy treatment in the head and neck region);
- chronic migraine and other forms of headaches;
- chronic and neuropathic pain conditions, including post-herpetic neuralgia, trigeminal neuralgia and post-traumatic forms of neuralgia;
- bruxism (teeth/jaw clenching);
- hyperhidrosis (excessive sweating);
- achalasia (dysfunction of the oesophagus (gullet) muscles, leading to dysphagia (difficulty with swallowing));
- hypersalivation (excessive production of saliva);
- gustatory sweating (excessive sweating in regions of the face; can occur following surgery to the parotid gland).
The muscle paralysis and relaxation caused by botulinum toxin injections typically lasts for 8 to 16 weeks. Whilst the affected nerve endings are preserved, the blockage of acetycholine release is irreversible. Recovery of the function of the neuromuscular junction and muscles occurs by the growth (‘sprouting’) of new nerve endings and synapses. Botulinum toxin injections are generally well tolerated, with few adverse effects. However, botulinum toxin alpha has some tendency to migrate away from the injection site by diffusion through tissue layers. If that happens, temporary problems with speech, dysphagia (swallowing) and breathing may occur after injection in certain areas of the head and neck region.