Neuropathies
Nerve damage
Contents
- The nerves in the head and neck region
- Cranial nerve I, the olfactory nerve
- Cranial nerve II, the optic nerve
- Cranial nerve III, the oculomotor nerve; cranial nerve IV, the trochlear nerve; cranial nerve VI, the abducens nerve
- Cranial nerve V, the trigeminal nerve
- Cranial nerve VII, the facial nerve
- Cranial nerve VIII, the vestibulocochlear nerve
- Cranial nerve IX, the glossopharyngeal nerve
- Cranial nerve X, the vagus nerve
- Cranial nerve XI, the accessory nerve
- Cranial nerve XII, the hypoglossal nerve
- Cervical spinal nerves
- The most common maxillofacial neuropathies
Below we give an overview of properties and functions of the nerves in the head and neck region, together with a brief summary of consequences and dysfunction following damage to these nerves, and the most common causes of damage. We conclude this section with a summary of the most common maxillofacial neuropathies.
The nerves in the head and neck region
The human body has 12 pairs of cranial (skull) nerves, originating from the brain and upper spinal cord. In addition, there are 8 pairs of cervical (neck) spinal nerves, originating from the cervical part of the spinal cord.
Given the role of the brain as the control centre of the body, it is not surprising that the head and neck region is particularly rich in nerves, nerve bundles and groups of nerves that are involved in the regulation and delivery of a large proportion of body functions, as diverse as sense of taste, heart rate, digestive system, or shoulder movement. The cranial nerves can be broadly subdivided into sensory nerves, motor nerves, or a combination of both modalities.
The brain as the body-control centre requires two-way traffic of information. Some cranial nerves deliver information from the body to the brain; this afferent (incoming) mode is delivered by sensory nerves, reporting from skin and internal organs, as well as about sight, sound, balance and taste. Other cranial nerves deliver instructions from the brain to the body; this efferent (outgoing) mode is carried out by motor nerves and activates skeletal muscles, autonomic muscles such as the heart muscle, the smooth muscles of the gut, and the muscles of the many, highly specialised structures in the head & neck region (derived from the pharyngeal arches in developmental terms). Some cranial nerves carry out both sensory and motor functions.
There is an intricate network of task sharing between groups of cranial and cervical nerves to accomplish some of the fiendishly complicated processes that are necessary for the smooth functioning of a living body. Given the many different functions of cranial and cervical nerves and the high density of these nerves in the head and neck area, it will not come as a surprise that these nerves, their wellbeing as well as all kinds of damage and repair to them, are a prominent topic in maxillofacial surgery. It will also not be a surprise that there is a bewildering range of neuropathies related to these two groups of nerves.
There is obviously some overlap with neurology as well as with many other medical specialties and thorough diagnosis is essential. It is important to ascertain that signs and symptoms are indeed caused by problems of the nerve(s), rather than by a functioning nerve in conjunction with a failure to process signals in the brain or a muscle-related problem.
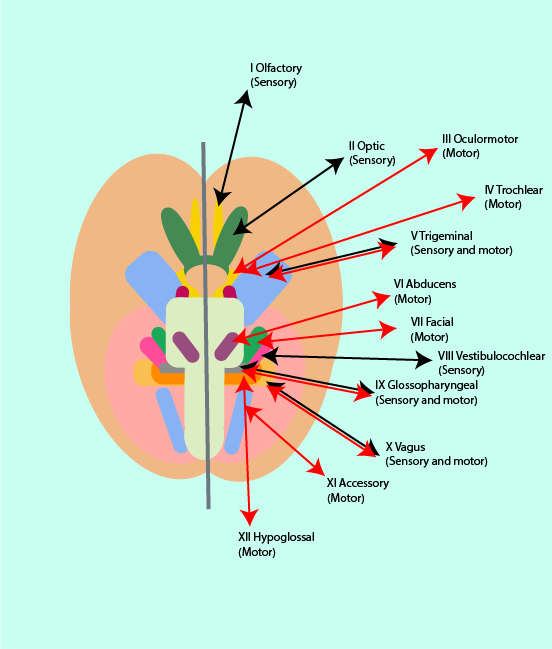
Having said all of the above, some form of orderly discussion of this topic is desirable. Anatomy is a medical specialty with a particular tendency to classification and ordering in the description of complicated systems. For the following discussion, we adopt the anatomical approach to bringing some order to the theme of cranial and cervical nerves. The anatomical approach is to simply number the twelve pairs of cranial nerves according to their origin from the base of the brain (see Figure 1) I to XII. The eight pairs of cervical nerves originate from the spinal cord through the spaces between vertebrae; the cervical nerves are numbered from top to bottom 1 to 8. The cervical nerves originating from the bottom part of the cervical spinal cord (C5 to C8) have several functions overlapping with functions of some of the thoracic (chest region) spinal nerves, while C1 to C4 have some overlap in location and function with some of the cranial nerves.
In order to reach their destinations and target areas, the cranial nerves need to escape from the bony confinement of the skull. This happens either by a nerve passing through a small hole (a foramen) in the bone, or by a nerve travelling inside a hollow bony tube. These bony tubes may host more than one nerve branch as well as some blood vessels. While having a delicate structure protected by bone seems sensible, having it surrounded by something which does not expand creates many of the problems associated with the nervous system.
Cranial nerve I, the olfactory nerve
Type and function
The olfactory nerve is a sensory nerve. It is the shortest of the cranial nerves as it only travels from its origin (see Figure 1 above) to the nose where it provides for the sense of smell. Small volatile (odour) molecules enter the nasal cavity when inhaling. These molecules are sensed by a very large number of special olfactory receptor neurons in the many fibres of the olfactory nerve. The olfactory receptors are embedded in the mucosa (lining) of the nose where an initial response is triggered that leads to further signal transmission through the olfactory nerve to the brain. There the signal cascade is interpreted as the rich experience of smell.
Consequences of damage
are the inability to smell (anosmia) or a distorted sense of smell (parosmia), usually contributing to an overall distortion or lack of taste (because the perception of flavour is the result of complex combined smell and taste contributions).
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include
- trauma to the head, such as fractures of facial bones;
- infections such as infections of the respiratory tract or meningitis;
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant maxillofacial region;
- primary neurological pathology (that is something specific to the central or peripheral nervous system, such as multiple sclerosis (central) or a nerve sheath tumour (peripheral). This can apply to all the mentioned nerves.
Cranial nerve II, the optic nerve
Type and function
The optic nerve is a sensory nerve and is considered a part of the central nervous system (the brain) because some of its properties make it distinct from the other cranial nerves and akin to brain cells. The optic nerve enables vision. Its function involves picking up signals from photoreceptors in the retina (a region in the back of the eye that is equipped with light-sensitive molecules that trigger neural signals) which it transmits to the region of the brain responsible for processing of visual information (the visual cortex). There is a blind spot in the eye where the optic nerve exits the eye. The optic nerve of a human is made up of typically more than a million of nerve fibres.
Transmission of visual information by the optic nerve to the brain includes information about colour, contrast and brightness, as well as two reflexes. One of the two reflexes is the light reflex which regulates the synchronised constriction of the pupils of both eyes as a function of light intensity; the other reflex is the accommodation reflex that adjusts the acuity of vision as a function of distance / closeness of looking at objects by adjusting the lens.
Consequences of damage
include a range of different patterns of vision losses, both temporary and permanent, sudden or slowly developing. Vision loss can be blindness in one eye (monocular) or both eyes (bilateral). It is also possible that partial vision loss in one or both eyes occurs. This can take different forms, such as loss of vision in the outer half of the visual field of both eyes (bitemporal hemianopia), or loss of half of the visual field on the same side of both eyes (homonymous hemianopia).
There may be painful inflammation of the optic nerve with loss of central vision. Swelling and oedema affecting the eyes can give rise to a range of different vision problems.
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
mostly include systemic conditions such as multiple sclerosis or diabetes mellitus, or conditions affecting the central nervous system (for example stroke) or exposure to high-energy radiation, as well as specific ophthalmic (eye) conditions (such as glaucoma) and unknown causes (idiopathic).
In a more maxillofacial-focussed context, common causes include
- trauma to the head, such as fractures of facial bones;
- infections such as infections of the head and neck region, abscesses or cavernous sinus thrombosis;
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant head and neck region; for example, glioma of the optic nerve or a tumour of the pituitary gland, or compression due to swelling within the orbit (eye socket);
- primary neurological pathology.
Cranial nerve III, the oculomotor nerve; cranial nerve IV, the trochlear nerve; cranial nerve VI, the abducens nerve
Type and function
The oculomotor (III), the trochlear (IV) and the abducens (VI) nerves are all motor nerves; the three nerves together orchestrate the movements of the eyes in a coordinated fashion. Most of the eye’s movements are controlled by the oculomotor nerve (III), including constriction of the pupil, accommodation and opening of the eyelid. The trochlear (IV) and abducens (VI) nerves each control one specific muscle for eye movement: the trochlear nerve innervates the muscle responsible for rotational eye movement (superior oblique muscle), the abducens nerve innervates the muscle responsible for lateral eye movement (lateral rectus muscle).
Consequences of damage
to one, some or all of the three cranial nerves III, IV and VI affect the movement of the eyeball(s) in several ways. Almost always some form of double vision (diplopia) will occur. Damage to the oculomotor (III) nerve can cause a lack of coordination and synchronisation of the eye movements (strabismus), drooping of the upper eyelid (ptosis) and dilated pupils, in general the eye appears ‘down and out’. Damage to the trochlear (IV) nerve causes diplopia on looking down. Damage to the abducens (VI) nerve causes diplopia on looking sideways and may give rise to jerky involuntary eye movements (nystagmus).

Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include systemic conditions such as multiple sclerosis, or other brain lesions.
In a more maxillofacial-focussed context, common causes include
- trauma to the head, such as fractures of facial or skull bones. The abducens nerve is particularly vulnerable to damage by fractures of the petrous temporal bone. Curiously most double vision following maxillofacial trauma, particularly to the cheekbone and eye socket complex, is due to local mechanical trapping of muscle or inhibition of movement caused by scarring within the periorbital fat;
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant head and neck region, or by aneurysms (bulging) of the internal carotid artery (the carotid arteries are the pair of large arteries along the neck providing blood supply to the head, brain, eyes, and other structures);
- primary neurological pathology.
Cranial nerve V, the trigeminal nerve
Type and function
The trigeminal nerve (V) is the regionally (in the head and neck region) most extensive of the cranial nerves. It has both motor and sensory functions for the face and the mouth. It is split into three main branches: i) the ophthalmic nerve (V1), ii) the maxillary nerve (V2), and iii) the mandibular nerve (V3). V1 and V2 are purely sensory branches of the trigeminal nerve, V3 has motor and sensory functions.
The ophthalmic nerve V1 provides sensation to the skin, mucosa and sinuses of the upper face and scalp. After it exits the skull via the superior orbital fissure (cleft in the skull bones in the back of the eye socket), it separates into three branches: the frontal nerve, the lacrimal nerve, the nasociliary nerve. Between them these three branches provide sensory innervation for the forehead and scalp, the sinuses and the nasal cavity, upper eyelid, cornea and iris, the back (dorsum) of the nose, the lacrimal glands (glands producing tears; parasympathetic function of nerve fibres of V1 form a part of the tear-secretion regulation). The innervation of the cornea by V1 supports the corneal reflex (blinking triggered by touching the surface of the eye) by transmitting information to the brain, the facial nerve (VII; see below) activates the corneal reflex.
The maxillary nerve V2 provides sensation mostly to the mid third of the face. After exiting the skull, it divides into numerous sensory regional branches with further sub-branches. These numerous branches and sub-branches provide sensory functions to the lower eyelid, the lower back of the nasal cavity, the cheeks and sinus of the upper jaw, the side of the nose, the upper palate, the upper lip, teeth and gingiva (gums).
The mandibular nerve V3 innervates the muscles involved in biting and chewing, and some of the many muscles needed for swallowing, in addition to its sensory functions. It has several sub-branches which together provide sensation to the skin in the lower third of the face, the teeth and gums (gingiva) in the lower jaw and the front part of the tongue (but not including taste sensation in that region; this is carried by a branch of the facial nerve (VII; see below)) and the floor of the mouth.
The auriculotemporal nerve branch of V3 innervates the outer ear, earlobe, outer ear canal and the middle ear, as well as the temple. The buccal branch of V3 provides sensation to the buccal mucosa (the cheek inside the mouth) and to the 2nd and 3rd molar teeth. The inferior alveolar nerve branch of V3 has both motor and sensory functions. Part of it innervates the mylohyoid and some of the digastric muscles (in the neck), which are necessary for swallowing. Another part of the inferior alveolar nerve branch of V3 travels through some bony tunnel inside the mandibular (lower jaw) bone and provides sensation to the teeth in the mandible. At the front of the mandible, it exits the bony tunnel of the mandible through a small hole (the mental foramen). From there it is known as the mental nerve and supplies sensation to the lower lip and chin. The lingual nerve branch of V3 is a sensory nerve branch and provides sensation to the front two thirds of the tongue and the floor of the mouth.
The mandibular nerve carries motor fibres to various muscles in the head and neck. It innervates the muscles of mastication (chewing): the masseter, media and lateral pterygoid, temporalis and tensor tympani muscles, as well as some of the muscles required for swallowing (mylohyoid and anterior belly of digastric, tensor veli palatini muscles).
The trigeminal nerve itself does not carry any fibres of the autonomic (involuntary) nervous system but such nerve fibres from other cranial nerves hitchhike on the various branches of the trigeminal nerve to a common destination:
- the chorda tympani branch of the facial nerve (VII; see below) travels with the lingual branch of the mandibular nerve and provides taste sensation to the front of the tongue, then it branches further to innervate the submandibular and sublingual salivary glands where it contributes to the saliva-secretion regulation;
- the auriculotemporal branch of the trigeminal nerve provides passage for the autonomic nerve fibres of the glossopharyngeal nerve (IX; see below) for innervation of the parotid salivary gland where it forms part of the saliva-secretion regulation;
- autonomic fibres of the facial nerve (VII; see below) travel with the maxillary branch of the trigeminal nerve to the lacrimal glands and the nasal mucous glands where these fibres contribute to the glands’ secretion regulation.
Consequences of damage
to the trigeminal nerve are as varied as the different functionalities of this nerve; signs and symptoms depend on the location and cause of the damage. Signs and symptoms of damage include absent corneal reflex, absent or distorted sensation in the areas supplied by the sensory functions of the trigeminal nerve, weakness of the muscles of mastication (chewing muscles). Damage to a peripheral branch of the trigeminal nerve may be more specific, according to the specific functionalities of the branch. An example is the initially numb area over the cheek when a fractured cheekbone presses on the infraorbital nerve lying in the eye socket. The entire area below the eye and extending to the side of the nose, lip and gums may be numb. Over time, if the compression is removed by returning the bone to its proper position, the numbness may gradually vanish, become an irritating sensation which never quite goes away (although one can become used to it), or even get worse. It really is unpredictable.
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
generally include brain lesions (strokes and/or tumours in several areas of the brain, especially near the brainstem, affect the trigeminal nerve), multiple sclerosis and diabetes mellitus.
In a more maxillofacial-focussed context, common causes of damage to the peripheral section of the trigeminal nerve include
- trauma to the head, such as fractures of the skull base;
- trauma caused by oral or maxillofacial surgical interventions; classically damage to sensation of the lip or tongue in operations to remove wisdom teeth, or move the lower jaw (sagittal split osteotomy);
- compression by tumour growth (malignant as well as non-malignant masses in the relevant head and neck region including schwannoma, metastasis, tumours in the nasopharyngeal area), or by aneurysms (bulging) of the internal carotid artery (the carotid arteries are the pair of large arteries along the neck providing blood supply to the head, brain, eyes, and other structures), or cavernous sinus thrombosis;
- infections such as maxillary sinusitis, abscesses;
- autoimmune conditions such as Sjögren’s syndrome;
- primary neurological pathology, trigeminal neuralgia being a classic.
Cranial nerve VII, the facial nerve
Type and function
The facial nerve (VII) has both motor and sensory functions. It first follows a fairly complicated path in the skull, passing very close to the inner ear, before it enters its extracranial (outside the skull) path, there running just to the front of the outer ear. Intracranially (inside the skull) it divides into three branches: the greater petrosal neve (provides innervation and regulation to mucous and lacrimal glands), the nerve to stapedius (motor function for the stapedius muscle, small muscle of the middle ear), and the chorda tympani (sensory innervation, sense of taste in the front part of the tongue and innervation to the submandibular and sublingual salivary glands). The chorda tympani hitchhikes on the lingual nerve (trigeminal nerve, V; see above) toward the base of the tongue before continuing toward the submandibular and sublingual salivary glands. The lingual nerve provides sensation to the front two thirds of the tongue, the chorda tympani fibres provide taste sensation for this part of the tongue.
The main branch of the facial nerve runs through the parotid (salivary) gland, where it divides into five sub-branches: temporal, zygomatic, buccal, marginal mandibular and cervical branches. These five motor branches innervate the facial muscles that are responsible for facial expression. The facial nerve is embedded in the parotid gland tissue but does not innervate the parotid gland. The gland is innervated by the glossopharyngeal nerve (IX; see below). Several more motor nerve branches emerge: the posterior auricular nerve (serving muscles of the outer ear), the nerve to the posterior belly of the digastric muscle and the nerve to the stylohyoid muscle (muscles in the neck, involved with swallowing, speaking and breathing).
Consequences of damage
to the facial nerve are diverse. Given its multiple functions and anatomical paths, the signs and symptoms depend on the location and cause of the damage. Intracranial lesions of the facial nerve affect both its motor and sensory functions, extracranial lesions only affect its motor functions.
Intracranial lesions lead to paralysis or severe weakness of the muscles of facial expression. In addition, there may be sensitivity to sound, loss or distortion of taste, reduced salivary and / or lacrimal secretion, distorted sensation. Extracranial lesions lead to paralysis or severe weakness of the muscles of facial expression.

Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
- to the intracranial section of the facial nerve include lesions of the middle ear, such as infection, iatrogenic (surgery to the middle ear), or compression by tumour growth (malignant as well as non-malignant space-occupying growth);
- to the extracranial section / branches of the facial nerve include pathology of the parotid gland (surgery, infection, tumour), infection of the nerve (herpes zoster infection in particular), idiopathic (unknown cause), including Bell’s palsy (the most common lesion of the facial nerve);
- there may be general underlying conditions such as multiple sclerosis, diabetes mellitus, borreliosis (Lyme disease, which is increasing in frequency), or Guillain-Barré syndrome (autoimmune condition affecting the peripheral nervous system).
Cranial nerve VIII, the vestibulocochlear nerve
Type and function
The vestibulocochlear nerve is a purely sensory nerve. It consists of two strands of nerve tissue, vestibular and cochlear fibres. The vestibular part of the nerve reports balance information to the brain, the cochlear part transmits hearing information, in the form of amplitude and frequency of sound waves, from the ear to the brain.
Consequences of damage
to the vestibulocochlear nerve include hearing loss, vertigo (loss of balance, dizziness), distorted sense of motion and motion sickness, nausea, tinnitus (ringing noise in the ear), reduced sense, or loss, of equilibrium in the dark.
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include
- primary neurological pathology: acoustic neuroma (a benign tumour of the vestibulocochlear nerve);
- fracture of the skull base or other major trauma to the head;
- inflammation of the nerve (vestibular neuritis), unknown origin but possibly associated with reactivated herpes simplex infection;
- noise damage, far more common than one would expect;
- compression by space-occupying growth, including Paget’s disease;
- Ménière’s disease (a condition affecting the inner ear, cause unknown).
Cranial nerve IX, the glossopharyngeal nerve
Type and function
The glossopharyngeal nerve has various different motor and sensory functions, including some special functions. Its various branches provide sensory functions to the mouth and throat (including the tonsils and parts of the carotid artery), the back part of the tongue (including taste sensation for this part of the tongue), the middle ear and the Eustachian tube (connects the middle ear with nose and throat). Its motor function is to innervate one of the muscles in the pharynx required for swallowing (the stylopharyngeus muscle). In addition, the glossopharyngeal nerve has a special function in that it provides autonomic (involuntary) parasympathetic innervation to the parotid salivary gland and thus is part of the saliva-flow regulation system. It is connected with the auriculotemporal nerve (a cervical spine nerve; see below) in approaching the parotid gland. One of the branches of the glossopharyngeal nerve serving the back of the mouth and throat is closely linked with the vagus nerve(X; see below). This relationship of the two nerves is functionally important: the glossopharyngeal nerve provides the sensory (afferent) information for the gag (and vomiting) reflex to the brain, the (efferent) motor instruction from the brain for the gag reflex is carried by the vagus nerve to the back of the tongue / throat.
Consequences of damage
to the glossopharyngeal nerve include the loss of the gag reflex and specific swallowing difficulties, loss of sensation (anaesthesia) in the back of the mouth and throat, and/or problems with speech. Often problems arise from damage to both the glossopharyngeal and vagus (X; see below) nerves, or from damage to the vestibulocochlear (VIII; see above) and the glossopharyngeal nerves. A sign and symptom of damage to the glossopharyngeal nerve may be glossopharyngeal neuralgia (intermittent pain at the base of the tongue and palate).
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include brainstem lesions (in particular ischaemic stroke), Parkinson’s disease (where tremor can affect the muscles in the throat), a range of motor neuron diseases.
In a more maxillofacial-focussed context, common causes include
- trauma to the head, such as skull base fractures or fractures of the styloid process (protrusion of the temporal bone);
- primary neurological pathology, such as neuroma;
- infection such as skull base osteomyelitis;
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant head and neck region, for example malignant tumour of the tonsil.
Cranial nerve X, the vagus nerve
Type and function
Similar to the glossopharyngeal nerve (IX; see above) also the vagus nerve has a diverse range of functions. It extends far beyond the head and neck region all the way to the abdomen and travels furthest of all cranial nerves. Most of its fibres are sensory (thus reporting status and condition to the brain) but some of its fibres also execute instructions from the brain locally. The various branches of the vagus nerve provide sensory functions by innervating the skin of the outer ear canal (the auricular nerve), the mucosa in the throat as well as sampling visceral sensation from heart, lungs and digestive tract. A special sensory nerve function is the provision of taste sensation at the root of the tongue. In its motor function, it innervates most of the muscles of the soft palate, the pharynx (upper throat) and the larynx (lower throat). It further innervates the smooth muscles of the windpipe, lungs and digestive tract and is involved in the regulation of the heartbeat. It mediates the gag reflex (together with the glossopharyngeal nerve (IX), see above) and the cough reflex.
The pharynx and larynx muscles innervated by the vagus nerve are necessary to start the swallowing process and for the production of speech sounds. The vagus nerve plays a major role in the regulation of the heart rate by reducing and maintaining the rate at rest. In the gastro-intestinal system the vagus nerve branches in this region stimulate secretion of the various glands (including sweating and acid production in the stomach) and contraction of smooth muscles in the digestive tract.
Consequences of damage
to the vagus nerve often are the effects of combined damage to include the glossopharyngeal nerve (IX; see above) and accessory nerve (XI; see below). Given the many functionalities of the vagus nerve, signs and symptoms of damage to it are manifold and varied, ranging from pain in the mouth to accelerated rate of heart beat and increase in blood pressure, to breathing problems, to hoarse voice and general difficulties with swallowing and speech. Signs and symptoms of vagus nerve damage depend on the exact location of the damage.
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include brain lesions, metabolic disorders (such as diabetes mellitus or vitamin B12 deficiency), degenerative conditions such as motor neurone disease, or multiple sclerosis.
In a more maxillofacial-focussed context, common causes include
- trauma to the head, such as skull base fractures;
- iatrogenic from procedures such as thyroid or carotid surgery;
- compression or invasion by tumour growth (malignant as well as non-malignant masses) not just in the head and neck region, including for example metastasis from lung and other chest malignancies;
- primary neurological pathology, such as nerve sheath tumour (schwannoma).
Cranial nerve XI, the accessory nerve
Type and function
The accessory nerve is a motor nerve. It has dual character in terms of its anatomical origins; this two-component view is the traditional anatomical description of the accessory nerve. The main part of the accessory nerve is made up of nerve fibres that stem from cervical spinal nerves C1 to C5 (see below). The smaller cranial part of the accessory nerve travels with the glossopharyngeal (IX) and vagus (X) nerves (see above) on exiting the skull. An alternative anatomical view considers the cranial part of the accessory nerve as a part of the vagus (X) nerve, and the accessory nerve itself is then seen as a purely cervical spinal nerve (see below).
Independent of its systematic anatomical descriptions, the accessory nerve innervates two muscles of the neck: the sternocleidomastoid muscle (running along the side of the neck) and the trapezius muscle (large muscle of the back, extending to head and neck). The accessory nerve in conjunction with these two muscles enables extension, lateral flexion and rotation of the neck, as well as elevation and rotation of the scapula (shoulder blade) related to abduction of the arm.
Consequences of damage
to the accessory nerve are difficulties with moving head, neck and shoulders, a limited range of motion, weakness and shoulder pain. Over time with long-standing nerve damage, the sternocleidomastoid and trapezius muscles may weaken. This can lead to a non-symmetrical neckline.

Common causes of damage
include
- trauma to the neck region; the accessory nerve is vulnerable to such damage;
- most common cause is iatrogenic, resulting from surgical procedures such as neck dissection or lymph node biopsies in the neck region, or other surgery to the neck;
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant neck region;
- primary neurological pathology.
Cranial nerve XII, the hypoglossal nerve
Type and function
The hypoglossal nerve is a motor nerve, it innervates all the tongue muscles with one exception (the palatoglossus muscle which is controlled by the vagus nerve (X), see above; as an alternative view, fibres of the hypoglossal nerve may be seen as intermingled with the vagus nerve). A branch of the hypoglossal nerve connects with a branch of the first cervical spinal nerve, C1 (see below). The hypoglossal nerve connects to the tongue from the bottom region of the floor of the mouth and travels through otherwise densely innervated areas that are also rich in blood vessels.
The mostly voluntary and some involuntary functions of the tongue are necessary for speech, swallowing and manipulation of food in the mouth (formation of a bolus, ready to swallow). The clearing of saliva from the mouth is the predominant involuntary function, as well as some acquired functions for speech and articulation – which are specific to particular sounds in different languages.
Consequences of damage
to the hypoglossal nerve are difficulties with speech (slurred speech), chewing and swallowing (dysphagia) as well as disturbed sensation of the tongue (dysaesthesia). Over time additional weakness of the tongue muscles may develop, such atrophy (wasting away) of the tongue musculature can add to the signs and symptoms of damage to the hypoglossal nerve. Often, the tongue cannot be moved symmetrically and will deviate to the affected side.
Depending on the cause, the signs & symptoms may be temporary or permanent, and may range from mild to severe.
Common causes of damage
include systemic conditions such as multiple sclerosis, or brain lesions and stroke, and motor neurone disease; damage to the hypoglossal nerve is rare.
In a more maxillofacial-focussed context, common causes include
- trauma to the head, such as fractures of facial or jaw bones, in particular condyle fractures (fractures of the top part of the lower jaw bone). Because of the path of the hypoglossal nerve and its proximity to other functionalities and structures, it is rare that this nerve is damaged in isolation;
- surgical procedures can damage the hypoglossal nerve. In its path to the tongue it may very rarely be damaged during submandibular gland excision or neck dissection. The hypoglossal nerve may be used in surgical reconstruction attempts to restore function to a severely damaged / paralysed facial nerve (VII, see above);
- compression by tumour growth (malignant as well as non-malignant masses) in the relevant head and neck region;
- primary neurological pathology.
Cervical spinal nerves
The cranial nerves I to XII each have predominantly individual character, despite some degrees of ‘task sharing’ and occupying shared spaces. The cervical spinal nerves have individually identifiable roots – where they originate from the spinal cord through the spaces between vertebrae – but they form more integrated networks of cooperative nerve actions. Such an integrated network is called a plexus. The cervical spinal nerves can be grouped into two such branched functional networks: the cervical plexus formed by the spinal nerves C1 to C4; the brachial plexus formed by the spinal nerves C5 to C8. We include a brief description of the cervical spinal nerves because of their functional overlap and intermixing with some of the cranial nerves.
Cervical spinal nerves C1 to C4; the cervical plexus
The branches of the cervical plexus C1 to C4 mostly serve the head and neck region, with both motor and sensory functions. The motor components innervate muscles of the neck, back and the diaphragm (the major muscle which serves to inflate the lungs; innervated by branches from C3, C4 and C5). Branches of C1, together with parts of the hypoglossal nerve (cranial nerve XII; see above) innervate several smaller muscles required to move the hyoid bone (a small bent bone in the neck, supporting the tongue). This is an essential function for speech and swallowing. The cervical plexus is also closely connected with the accessory nerve (cranial nerve XI; see above).
The sensory components of the cervical plexus generally provide sensation to the skin of the upper chest, neck, ear and scalp. More specifically, branches of C2 and C3 form the greater auricular nerve which travels upwards, provides sensation to parts of the outer ear and the skin over the parotid gland, and is interconnected with the auricular branches of the vagus nerve (X; see above) and the facial nerve (VII; see above).

Cervical spinal nerves C5 to C8; the brachial plexus
The brachial plexus formed by C5 to C8, plus the first of the spinal nerves of the thorax, T1, is a complicated network of major and minor branches. It provides both motor and sensory functions to the upper limbs (arms and hands / fingers).
Consequences of damage
to the brachial plexus include lack of, or distorted sensation (dysaesthesia) in the shoulder, arm or hand as well as weakness of the muscles in these structures, extending to paralysis in severe cases. Severe damage to C4 and C5 can cause breathing difficulties. Damage to the cervical plexus leads to distorted sensation in the areas innervated by this plexus, as well as difficulties with speech and swallowing when the motor branches of C1 are damaged.
Common causes of damage
include a herniated disc or trauma to the neck (from injury or surgery).
In a more maxillofacial-focussed context, common causes include
- surgical procedures such as parotidectomy (excision of the parotid gland) or neck dissection, leading to altered sensation of the earlobe and surrounding area.
The most common maxillofacial neuropathies
Neuropathies in a maxillofacial context are an extremely broad theme, in several regards. There is much overlap with conditions that are commonly referred to as facial pain syndromes, including some treatment options as well as common limitations to the management of many of these conditions. Furthermore, the whole spectrum of severity of neuropathies needs to be kept in mind. The range covers minor nuisances from temporarily slightly disturbed or reduced sensation (minor cases of dysaesthesia), to severe and lasting forms of dysaesthesia (sensory nerves), or severe, painful and lasting signs and symptoms of damage to motor and/or sensory nerves.
Both the ability (and willingness) to cope with lasting, sometimes life-changing disturbances varies strongly between individuals, including mood and mental health aspects. Not only general resilience is individually very different, also the perception of pain varies widely between individuals; one person’s unbearable pain is somebody else’s modest disturbance. In fact, it is not well understood why pain perception varies so widely; in part this may be attributed to the fact that it is not really possible to objectively determine degrees of pain or discomfort.
Neuropathies commonly encountered in maxillofacial surgery include damage to
- Cranial nerves III, IV, VI: superior orbital fissure syndrome; rare and usually of traumatic origin. The superior orbital fissure is a cleft in the skull bones forming the eye socket (at the back of the eye socket), a fracture of this bony structure can cause damage to some or all of the nearby cranial nerves III, IV, VI.
- Cranial nerve V: trigeminal neuralgia, a genuine idiopathic (unknown origin) change in the nerve’s cell membranes producing electric-shock like pain in short intense bursts. This disorder may be seen a little bit like epilepsy in reverse; this is the reason why carbamazepine and other anticonvulsant agents serve both diagnostic and treatment purposes.
- Cranial nerve V: damage to the lingual nerve (part of the mandibular branch of the trigeminal nerve (V3)) by surgical removal of third molars (wisdom teeth) or other oral & maxillofacial surgery. In the majority of cases the damage is a temporary and relatively minor nuisance, but there is a minority of cases where the damage is more severe and permanent.
- Cranial nerve V: damage to the inferior alveolar nerve (part of the mandibular branch of the trigeminal nerve (V3)), usually by trauma (such as fracture of the mandible) or surgery but also by compression from bone lesions such as cysts, or other voluminous growth.
- Cranial nerve V: damage to the mental nerve (the name of the inferior alveolar nerve after it exits its bony channel along the mandible through the mental foramen (a small hole in the front part of the mandible)), under normal conditions indistinguishable from other alveolar nerve injury but arising from damage to the mental branch of the nerve, usually from trauma or surgical interventions.
- Cranial nerve V: damage to the infraorbital nerve (part of the maxillary branch of the trigeminal nerve (V2)) typically causing altered sensation after cheekbone fracture or orbital (affecting the eye socket) surgery.
- Cranial nerve VII: damage to the chorda tympani branch of the facial nerve causes taste disturbances; a potential complication of surgery to the middle ear.
- Cranial nerve VII: Bell’s palsy (paralysis is often temporary), a neurological condition of the facial nerve, cause unknown but viral infections (herpes zoster (shingles)) and immune system dysfunction have been considered. Onset is typically sudden, with a typical asymmetrical facial appearance caused by the paralysis of the facial muscles innervated by the (motor) nerve.
- Cranial neve VII: Ramsey-Hunt syndrome (also known as herpes zoster oticus), a paralysis of the facial nerve with vesiculation (blisters and a red rash) around the ear on the affected side. The condition occurs when an outbreak of shingles affects the facial nerve near the ear, it causes a painful rush, facial paralysis and hearing loss on the affected side.
- Cranial nerve VII: Melkersson-Rosenthal syndrome is a rare neurological condition which causes recurring facial paralysis alongside fissuring of the tongue and swelling of the upper lip and face. The cause is not known but genetic origin has been discussed.
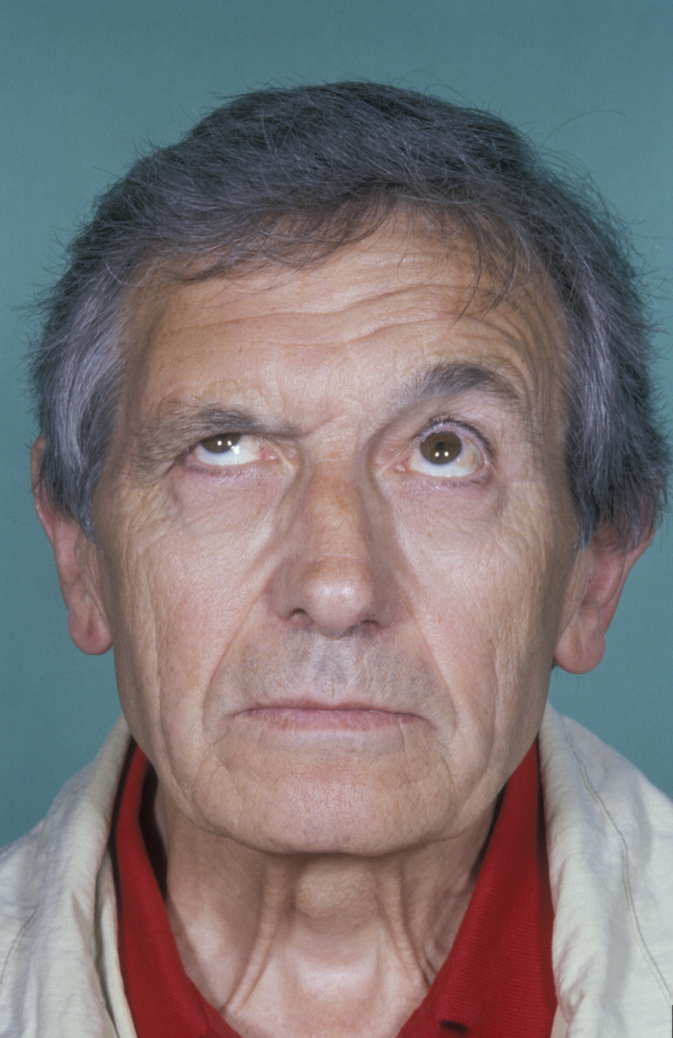
- Cranial nerve VII: direct tumour invasion (malignant as well as non-malignant growths), trauma and surgery can all cause paralysis of the respective branch of the facial nerve. These conditions are known as lower motor neuron paralysis where the function of the whole nerve is affected. These paralyses are different from upper motor neuron paralyses which originate from a central (brain) lesion such as a stroke, where the motor nerve supply to the forehead is maintained to a degree. An example of a complete lower motor neuron paralysis is shown in Figure 6.
- Cranial nerve VIII: damage to the vestibulocochlear nerve, causing hearing and balance problems; this is typically more in the realm of ear, nose and throat (ENT) surgery and clinic.
- Cranial nerves IX, X: damage to the glossopharyngeal and vagus nerves (the pharyngeal plexus) iatrogenic from surgical procedures or by compression, causing swallowing difficulties.
- Cranial nerve XI: damage to the accessory nerve leading to limitation of movement of the shoulder and neck on the affected side; this damage is usually caused by trauma or surgery, for example following neck dissection or other neck surgery.
- Cranial nerve XII: damage to the hypoglossal nerve causing deviation of the tongue to the affected side and weakness of the tongue; either caused by central nervous system (brain) lesions such as stroke, or (rarely) by surgery deep in the neck or floor of mouth, or as an extremely rare complication of excision of the submandibular (salivary) gland.
- Cervical plexus: altered sensation over the skin of the neck on affected side, most commonly numbness over the ear lobe and surrounding skin.