Salivary gland problems
Contents
Developmental disorders
Significant developmental disorders of the salivary glands are rare. Agenesis (absence) of one or more salivary glands has been described.
Heterotopic salivary tissue (salivary tissue occurring where it shouldn’t be) most commonly occurs in intra- and peri-parotid lymph nodes. It is of significance clinically when it presents as a mass, draining sinus, or neoplasm (newly formed). Stafne’s bone cavity occurs when heterotopic salivary tissue indents the mandible. The cavity is seen as a well corticated (with a hard, outer bone layer) radiolucency at the angle of the mandible below the inferior alveolar nerve canal.
Accessory (additional) salivary tissue adjacent to the glands is so common as to be normal.
Cystic disease may be developmental or acquired. Developmental cysts of the salivary glands are rare, the most common of these being the lymphoepithelial (consisting of lymphocytes and epithelial cells) cyst of the parotid gland.
Obstructive disease
Obstructions occur commonly in many of the body’s glands, including the salivary glands. The ductal system of the major salivary glands may be blocked by calculi (stones), mucus (thick secretions) or strictures (narrowing or other limitations).
Approximately 80 % of salivary calculi occur in the ductal system of the submandibular glands. This is due to the greater length of the duct, its upward course and the thicker mucus secreted by the submandibular glands. There will usually be a history of painful, recurrent swelling in the submandibular region, particularly associated with eating or the anticipation of eating (pre-prandial swelling). Plain (X-ray) radiography will usually demonstrate a calculus in the duct (see Figure 1), or in the junction of the duct and gland or the gland itself (see Figure 2).
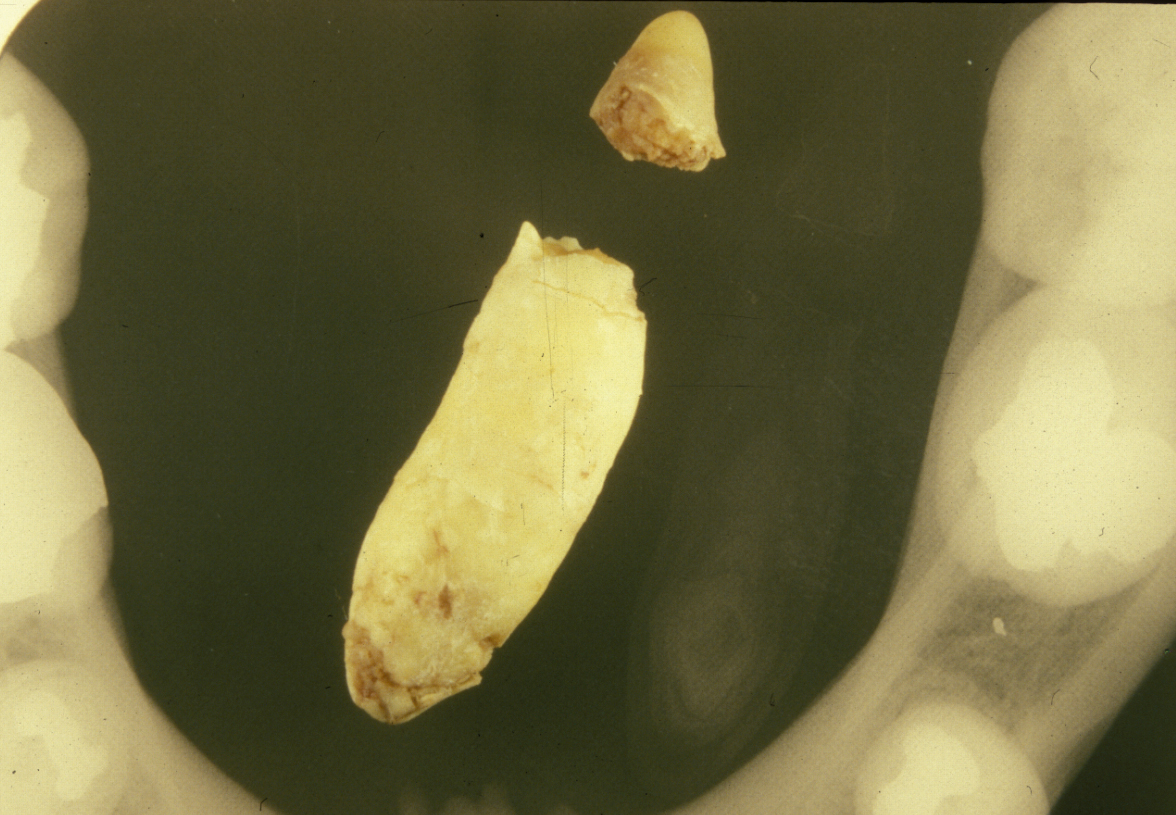

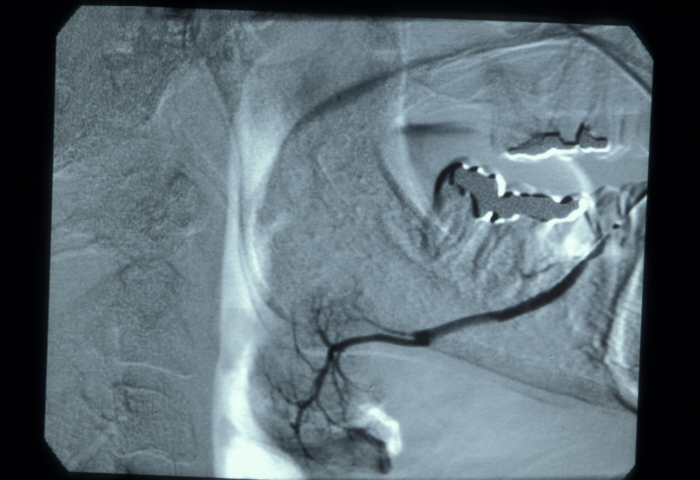
In the duct, a calculus is date shaped, at the junction of duct and gland it is comma shaped and in the gland it is round. Should a calculus not be visible on plain X-ray images, a sialogram is required which may demonstrate a radiolucent stone, a mucus plug or a stricture in the duct (see Figure 3).
Alternatively, a history of less severe symptoms with chronic obstruction can result in a fibrosed (scarred) gland. In either case there may be an acutely infected swollen gland. It is often the case that the submandibular gland will have suffered irreversible damage from a severe infection.
10 % of calculi occur in the parotid duct. Of these only 10 % are visible on plain (X-ray) radiographs. The substance obstructing the parotid may sometimes be inspissated (thick) mucus rather than a frank calculus. It may pass out as a string of jelly-like material, followed by relief of the symptoms. The parotid gland survives acute infective episodes much better than the submandibular gland.
The remaining 10 % of calculi occur in the sublingual and minor salivary glands.
Infections
Acute bacterial sialadenitis (inflammation of a salivary gland)
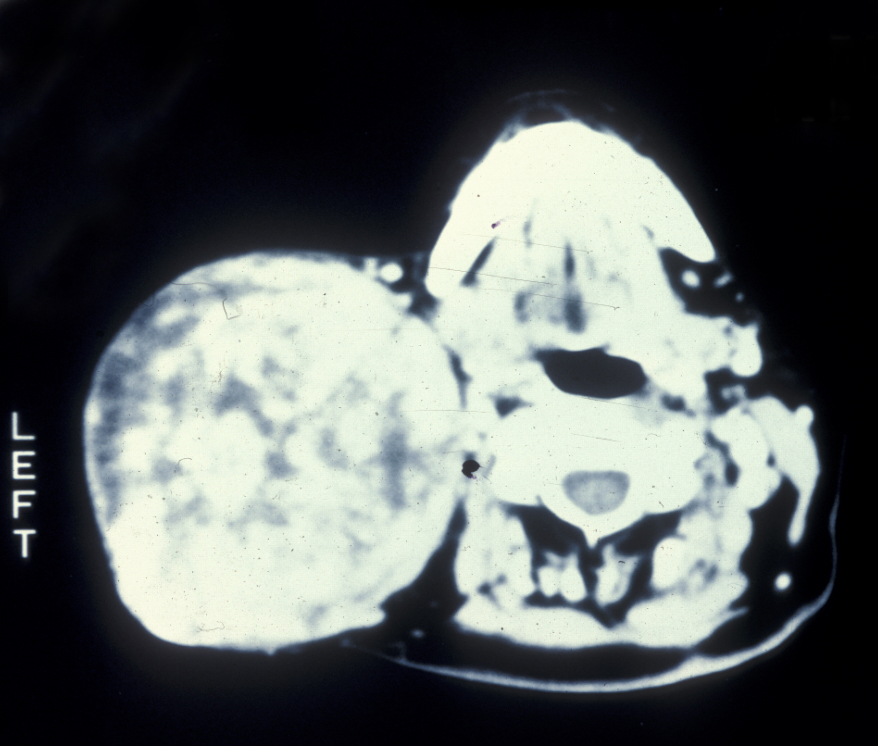
Now relatively rare, this condition usually affects the parotid gland. It is microbiologically different from infected obstructive sialadenitis (usually seen in the submandibular gland (see above) but also parotid). Classically it occurred in postoperative patients who were dehydrated. It still occurs in older patients who are dehydrated and debilitated but underlying Sjögren’s syndrome (see below) nowadays is a more frequent cause. There will be a swollen, erythematous (red skin), painful gland, often accompanied by systemic malaise (see Figure 4). Staphylococcus aureus is the usual organism, streptococci and other anaerobic bacteria are also frequently cultured.

Pus may be discharging from the papilla (see Figure 5). If not, the gland should be milked to obtain pus for microbiology. Abscess formation may be a (rare) sequela (develop as a consequence of the initial condition).

Following recovery from the acute phase a sialogram will be required to investigate any underlying abnormality and often this is therapeutic due to the mechanical irrigation with an antiseptic (the contrast agent usually contains iodine).
Chronic bacterial sialadenitis
This condition tends to affect the submandibular glands (probably due to the more viscous secretion being more difficult to clear than that of the parotid gland, and the propensity for calculi to form in the submandibular duct; see Figure 6).

Chronic bacterial sialadenitis usually occurs in a gland that has had a history of an acute infective or obstructive episode.
Viral sialadenitis
There are several viruses which can affect the salivary glands. By far the most common is the mumps virus (a paramyxovirus). Mumps is usually a disease of childhood. There is acute swelling of the salivary glands, particularly the parotid glands, which are involved in 70 % of cases. The other glands may be affected less frequently. Immunity is lifelong but mumps may occur in non-immune adults. In males the testes are involved in 20 % of cases, resulting in sterility in 1 %.
The cytomegalovirus (a virus belonging to the group of herpes viruses) affects the salivary glands in congenital cytomegalic inclusion disease. The seriousness of the involvement of other organs overshadows any clinical impact of salivary involvement.
Sjögren’s syndrome
Sjögren’s syndrome is an autoimmune disease characterised by a dry mouth (xerostomia) and dry eyes. It occurs most commonly in middle or old age, with women being affected ten times as often as men. When a dry mouth and eyes occur in isolation it is termed primary Sjögren’s syndrome. When these symptoms occur in combination with a connective tissue disease it is termed secondary Sjögren’s syndrome. It is of interest that the ocular (eye) and oral (mouth) symptoms are usually more severe in primary Sjögren’s syndrome. The most commonly associated connective tissue diseases are rheumatoid arthritis and systemic lupus erythematosis. Of those patients with rheumatoid arthritis, 15% report symptoms consistent with secondary Sjögren’s syndrome; for those with systemic lupus erythematosis the figure is 30 %.
A subjective feeling of a dry mouth may occur before changes are clinically evident and at this stage there may be no ocular symptoms. Early ophthalmological assessment is a good idea to check for the potentially sight compromising keratoconjuctivitis sicca (dry eye syndrome). As the salivary flow decreases the mucosa (lining of the mouth) takes on a dry and shiny appearance, with loss of papillae of the tongue. Diffuse non-painful parotid swelling is uncommon but 30 % of patients will give a history of such swelling.
There are various diagnostic tests. The medical history is important and a convincing history in the presence of an established connective tissue disease makes further investigation unnecessary. The mainstay of investigation is detection of autoantibodies (most clinicians would test for rheumatoid factor, anti-Ro and anti-La factors). If blood tests are unhelpful and further diagnostic information is required, then salivary gland biopsy may be performed. This entails removing five minor salivary glands from the lower lip. The histological findings of periductal lymphocytic infiltrate (T-cells), duct ectasia (dilation) and acinar atrophy (deteriorated acinar (secreting) cells) are characteristic of Sjögren’s syndrome. The lymphocytic infiltrate progresses with the disease and eventually replaces the salivary tissue. Lymphoma (malignancy of the lymph nodes) formation is more likely than random occurrence in those with Sjögren’s syndrome and this risk is greater in primary Sjögren’s syndrome. The increased risk of lymphoma formation should be borne in mind should a lump develop in the parotid glands.
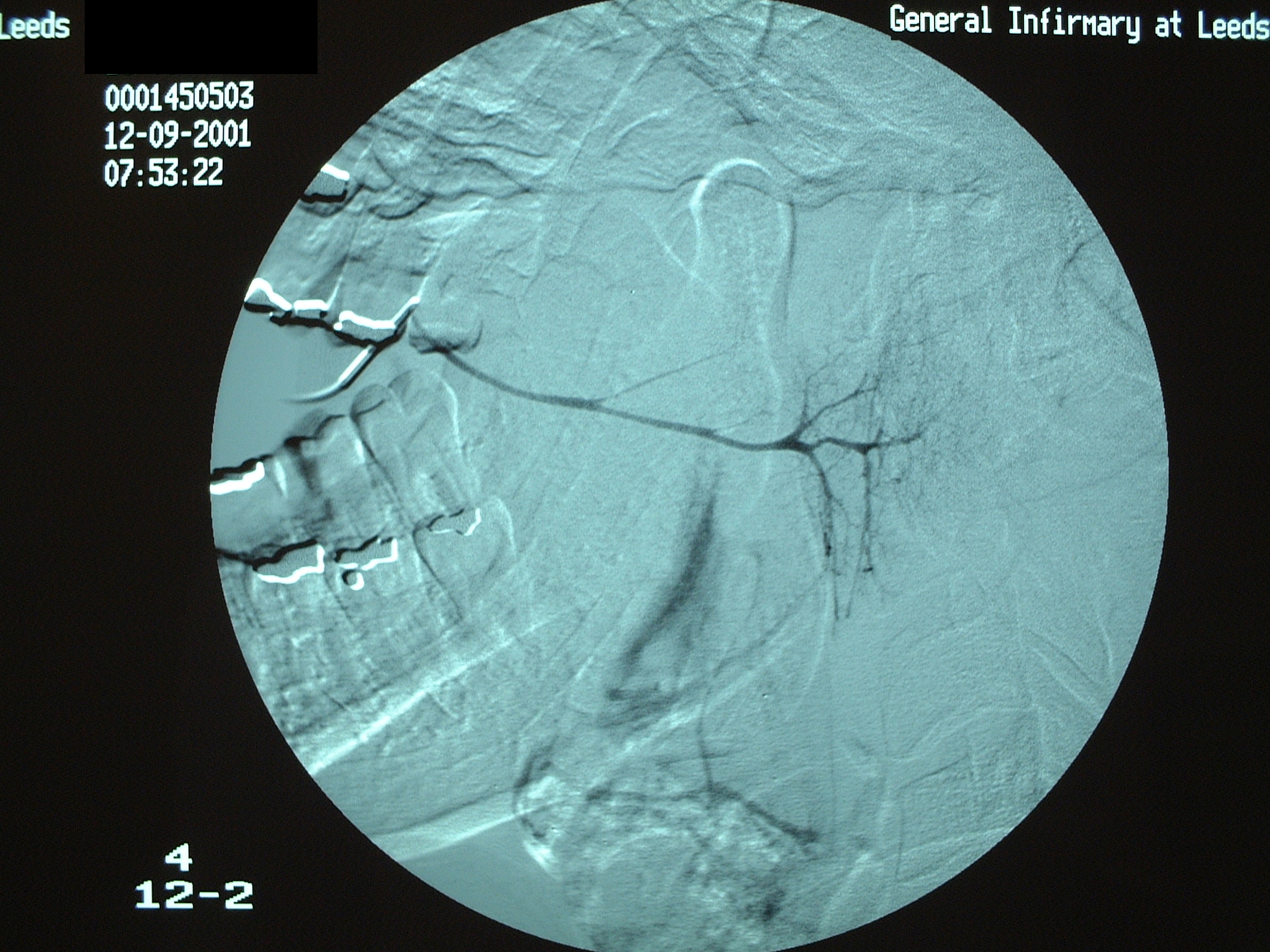
In those cases with a history of parotid swelling a sialogram will show a characteristic ‘snowstorm’ appearance of punctate sialectasis (spots of dilation of ducts) in Sjögren’s syndrome (see Figure 7). Decreased tear secretion can be measured objectively using small strips of paper placed in the lower eyelid (Schirmer’s test).
Sjögren’s syndrome has been internationally classified as is summarised in Table 1 and Table 2:
|
|
For primary Sjögren’s syndrome In patients without any potentially associated disease, primary Sjögren’s syndrome may be defined as follows:
For secondary Sjögren’s syndrome In patients with a potentially associated disease (for instance, another well defined connective tissue disease), the presence of item 1. or item 2., plus any two from among the items 3., 4. and 5. may be considered as indicative of secondary Sjögren’ syndrome. Exclusion criteria:
* Numerals refer to content of Table 1 |
Salivary neoplasms – benign tumours
There is a huge and bewildering range of salivary neoplasms; see Table 3.
|
The majority of salivary gland tumours have no clearly defined cause although Warthin’s tumour (lymphadenoma) is associated with smoking.
Presentation of virtually all these tumours is that of a slow growing mass (see Figure 8).
The majority of salivary gland tumours are benign, malignant tumours of the salivary glands are very rare.
Pleomorphic salivary adenoma is the most common (benign) tumour of the salivary glands, 75 % of pleomorphic salivary adenomas occur in the parotid gland and the vast majority of those are in the superficial lobe. These tumours are thought to arise from duct and myoepithelial cells. They occur in equal proportion in men and women. The average age of presentation is around 40 years but they may present over a wide age range. The pleomorphic epithet (characteristic) arises from the mixed fibrous, myxoid, cartilaginous and epithelial components. Although benign, the pleomorphic salivary adenoma is poorly encapsulated and requires excision with a small margin of normal tissue.
There are many other benign tumours of the salivary glands, most of which are uncommon. Of note is the adenolymphoma (Warthin’s tumour) which can be bilateral in up to 10% of patients. It is the only salivary gland tumour with an association with smoking and can sometimes vanish after FNAC (fine needle aspiration cytology), aspiration or enucleation despite being ‘multifocal’ which raises questions as to the true nature of this ‘tumour’.
Miscellaneous conditions
Necrotising sialometaplasia is a non-malignant condition of salivary gland tissue which clinically can appear to be a malignant tumour. It is a rare condition and occurs more commonly in men, usually in their 30s and 40s. The most common area is the palate and it presents as an ulcer. It has a short clinical course, with the ulcer appearing over a period of up to two weeks or so. This short history is a clue to diagnosis. Biopsy is mandatory to exclude carcinoma. Histopathologically the biopsy can be just as difficult to differentiate from cancer as the clinical appearance. The lesion heals by secondary intention (without intervention) in two to three months. More rapid healing can be obtained by excision with a small rim of normal mucosa and placement of a dressing plate with an obtundant (pain reducing) dressing.
Drooling is almost never caused by excess saliva production (which itself is unusual) as the saliva can simply be swallowed. Drooling is usually due to poor neuromuscular control of the lips or neck and head. The significance and severity of drooling varies widely, ranging from a temporary reaction to inflammation by teething in toddlers to severe effects in neurological conditions such as Parkinson’s or motor neuron disease.
Sialadenosis is enlargement of the salivary glands. It usually occurs in the parotid glands and may be idiopathic (unknown cause) or associated with diabetes mellitus, alcoholism, drugs or pregnancy.
Sarcoidosis is a reaction of the immune system, most likely triggered by inflammation. It leads to the formation of granulomas (multiple small lumps). This condition can occur everywhere in the body, it most commonly affects skin or lungs but may also affect the salivary glands, usually the parotids. If associated with lacrimal gland swelling, chorioretinitis (inflammation of the retina) and cranial nerve involvement it is termed Heerfordt’s disease.