Salivary gland anatomy, physiology & diagnostic toolbox
A brief summary of salivary gland anatomy
The parotid gland consists almost entirely of serous acini (cells that produce serous (watery) fluid; see below about physiology). The gland lies in the retromandibular fossa (near the angle of the mandible and in front of the ear) and has three surfaces. Its lateral surface is located subcutaneously and is enveloped in a tight fascia (connective tissue). This fascia is related to the subcutaneous musculoaponeurotic system (SMAS layer: a fairly inelastic layer of fibres and muscles in the deep skin layers of face and neck), with the greater auricular nerve branching anteriorally (in the front) into the skin and to the posterior (to the back) to the lobe of the ear. Its anterior surface wraps around the posterior border of the ramus of the mandible (the part of the mandible rising from the mandibular body, posterior to the molar teeth) and abuts the masseter and medial pterygoid muscles (cheek muscles). The deep surface of the parotid gland is complex and is related to the mastoid process (a space at the base of the skull, behind the ear), the posterior belly of the digastric muscle (small muscle under the jaw), the styloid process (small bone beneath the ear) and its associated muscles and ligaments, and the external carotid artery. Figure 1 shows MRI views of the parotid glands from two different angles.
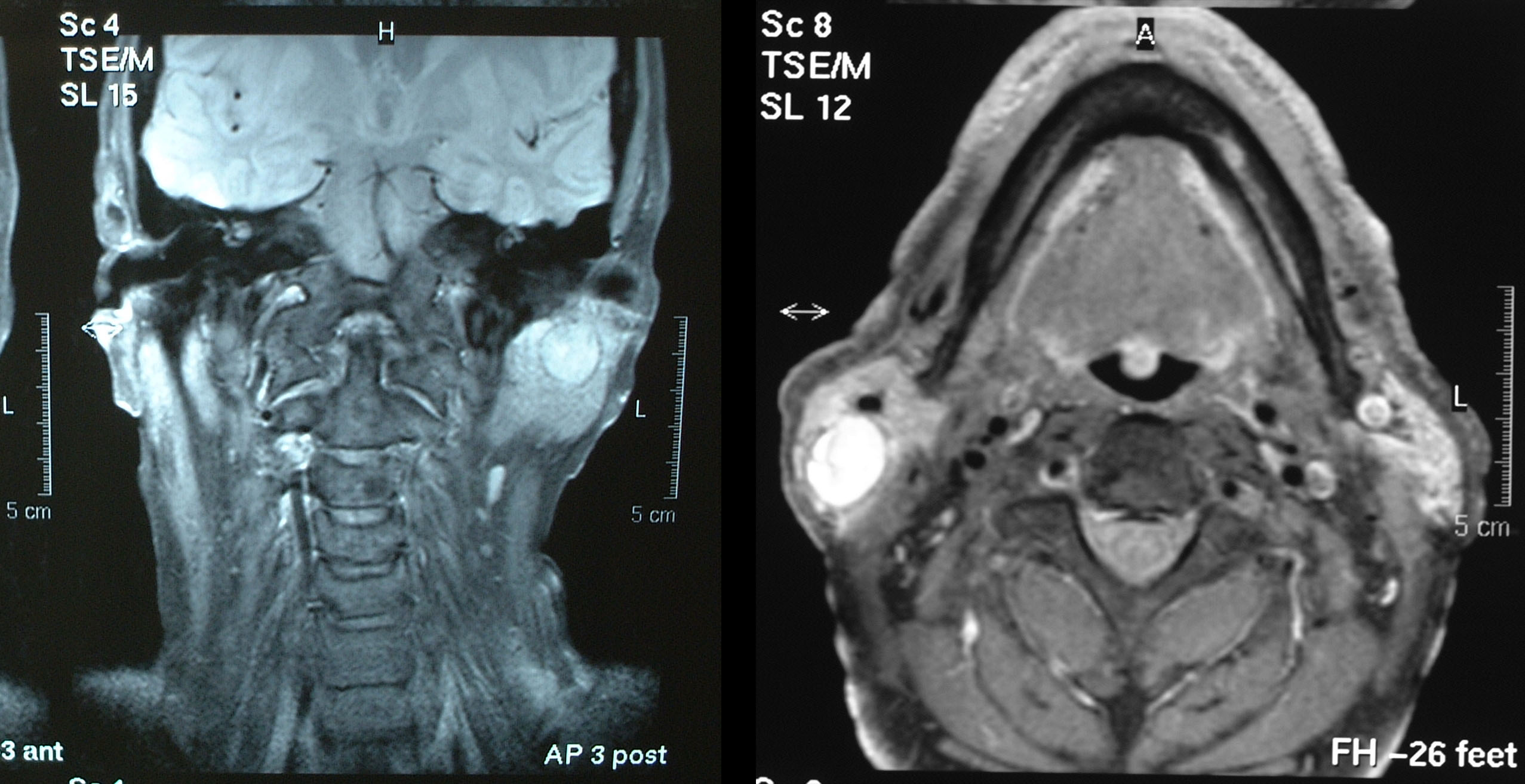
Within the parotid gland, the facial nerve branches into an upper and lower division from which stem the five named major branches. The nerve separates the gland into its superficial and deep lobes (see Figure 2). There is no natural tissue plane here and the nerve should be thought of as being embedded in the substance of the gland. Also within the gland are the retromandibular vein, external carotid artery, lymph nodes and filaments from the auriculotemporal nerve.
A 5 cm duct from the parotid gland lies on the superficial surface of the masseter muscle. It opens into the mouth opposite the second upper molar tooth. It is also known as Stensen’s duct. In about 50 % of people a small accessory parotid lies between the duct and the zygomatic arch (cheek bone).
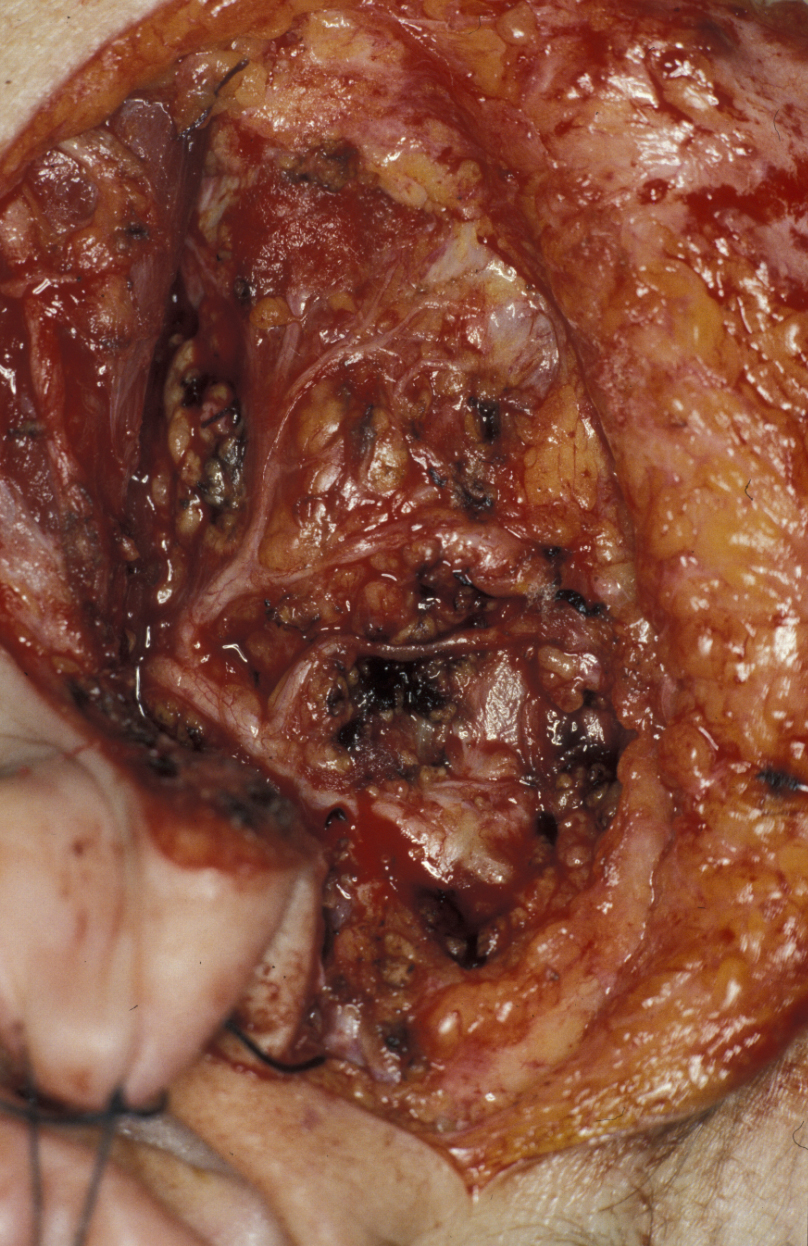
The submandibular gland is a mixed serous and mucinous gland (it produces a mixture of serous and mucus-rich secretion; see below). It is comprised of a large superficial lobe and a smaller deep lobe which is in continuity with the superficial lobe as it wraps around the posterior border of the mylohyoid muscle (running from the mandible down to the hyoid bone (a flat U-shaped bone in the middle-front of the neck). The gland is covered by a fibrous capsule. Figure 3 shows an excised submandibular gland.

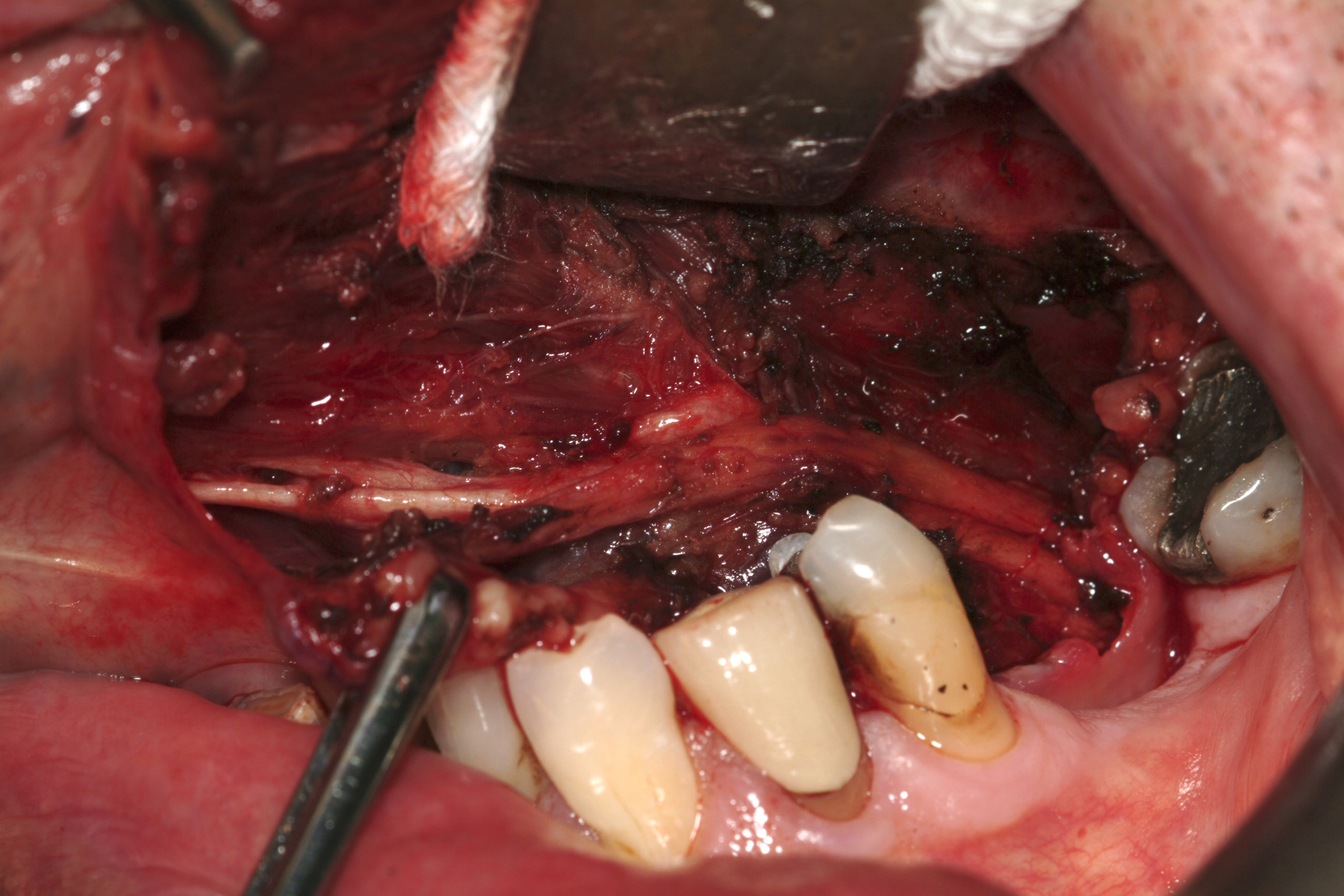
The mandibular branch of the facial nerve is quoted to dip below the lower border of the mandible in 20 % of people. The lingual nerve is intimately related to the submandibular duct (also known as Wharton’s duct) as the duct makes an upward and anterior course into the floor of the mouth. The lingual nerve is attached, by two branches, to the submandibular ganglion which lies in the gland.
The sublingual glands are mucinous glands (producing mucus-rich secretion) which lie on the mylohyoid muscle and are covered superficially by the mucosa (lining) of the floor of the mouth. Rather than one duct, they have several small ducts which open directly into the mouth and also into the submandibular duct. Their intimate relation to the lingual nerve and submandibular duct mean these are potentially at risk of injury during surgery (see Figure 4).
A brief summary of salivary gland physiology
The physiological role of the salivary glands is summarised by their name: the production of saliva. This may sound simple enough but in reality the production and the roles of different kinds of saliva are both complicated and diverse. Generally speaking, saliva is a multi-purpose fluid of variable viscosity. Saliva is mostly water but the small (variable) percentage content of electrolytes, enzymes and other proteins (mainly glycoproteins) makes all the difference to the physiological properties of different types of saliva.
By and large, the main tasks for saliva in humans are to
- maintain oral health
- enable eating
- enable speaking (by keeping the mouth moist)
In some other animals, saliva has further physiological tasks: for example, dogs have very little capacity to cool their body by sweating, so evaporating saliva from the tongue instead of sweating helps in that regard; the electrolytes in saliva provide an important mechanism for buffering and pre-digestion in ruminant animals such as cows and sheep.
In most animals, including humans, the various salivary glands produce different types of saliva for different purposes. In humans these are:
- parotid glands – serous / watery saliva with a high content of alpha-amylase, a protein that helps to break down starch in foods; at rest (that is: when not eating) saliva production in the parotid glands is minimal
- submandibular glands – mixture of watery and viscous saliva; produced at rest
- sublingual glands – predominantly viscous saliva; produced at rest
The autonomic nerve system (not under intentional control) regulates the type and amount of saliva being produced. For example, the presence of food in the mouth and chewing, the smell of food, or just thinking about food can trigger the production of serous saliva from the parotid glands (hence the proverbial mouth-watering food).
The roles and tasks of non-viscous and viscous saliva can be roughly subdivided as follows:
non-viscous saliva from the parotid glands mainly solubilises and breaks down food (in particular starch) and enables taste in this way; electrolytes provide buffering (help regulating and stabilising the pH, that is levels of acidity)
viscous saliva from the submandibular and sublingual glands lubricates foods, helps to form a slippery bolus of food (easy to swallow lump of food) and protects the mucosa from mechanical damage. In addition, the viscous saliva protects teeth: for example, the enzyme lysozyme in viscous saliva is a potent natural antibacterial agent that is essential in protecting teeth against decay. Again, electrolytes provide buffering and also protect teeth against damage, for example from acidic foods.
The diagnostic toolbox for investigating the salivary glands
There is some diagnostic role here for plain X-ray radiographs, in particular in conjunction with taking a sialogram to image the architecture of the ductal system of the salivary glands by using plain X-ray images, enhanced by contrast agent injected locally.
If there is a lump, imaging of the nature of the lump is required. A variety of MRI scans are the best modality. Ultrasound imaging investigations in experienced hands can be quite satisfactory too, as can be CT scans for obtaining more detailed X-ray information.
Fine needle aspiration cytology is usually a simple (but often painful to the patient) procedure and may provide support to a provisional diagnosis if malignancy or a cystic lesion is suspected on imaging.
Open or core biopsy of lumps of the major salivary glands has been decried in the past. This was due to the perceived risk of seeding tumour, in fact no hard data supports this concern. Core biopsy is acceptable and the tissue can be subjected to a variety of immunohistochemical tests which may save the patient from more invasive treatment. Ultrasound scan guided core biopsy of both salivary and cervical (neck) lumps carries the highest level of diagnostic accuracy under trial conditions. Whether that translates into routine clinical practice remains to be seen.
Examination of the constituents of saliva has no role in routine clinical practice.
Methods exist to measure salivary flow rates but their interpretation is difficult and the results, although used in research protocols, have little bearing on clinical practice.