Infection
The theme ‘infection’ is very broad, it would fill a bulky book to deal in any detail just with infections relevant in the head & neck region. Many of these infections and their treatment, for both hard and soft tissues, are described in detail in other sections of our website. We will point the reader to the relevant sections where appropriate.
Accurate diagnosis of infection is important both for treatment and public health management. Prompt identification of the organism causing infection enables the antimicrobial therapy to be specifically directed, which may allow rapid resolution of symptoms and minimises the opportunity for the development of resistant strains of bacteria This requires careful collection of specimens, accurate labelling and adequate clinical details to allow the clinical microbiologist to carry out the appropriate culture and sensitivity testing. In modern clinical practice, especially in a maxillofacial context, treatment of most infections will start immediately based on a ‘best guess’ antibiotics choice, and if necessary can be adjusted or altered lateron. A specimen can be contaminated by normal microflora and, where possible, the sample should be obtained by sterile aspiration, rather than swabbing of the area or a ‘pure’ pus sample collected from a drained abscess. If anaerobic or specific infections, such as tuberculosis, are suspected then designated special sample containers should be used for sample transfer to the microbiology laboratory. Samples should be sent to the laboratory without delay to ensure that culture of any organisms, including strictly anaerobic bacteria, is possible.
Serology (blood tests) can be useful, particularly in the case of viral and mycoplasma infections. It may be possible to identify viral antigens in serum, but it is more common to measure serum antibodies. This can allow the demonstration of a rising antibody titre over several days and thus to monitor response to treatment over time. It can also allow for identification of previous exposure. Unfortunately, it is often an ‘after the event’ diagnosis.
Here we give an overview of acute and chronic bacterial, viral and fungal infections, with links to other sections of the website where necessary.
Bacterial infections
Acute bacterial infections
Pericoronitis most commonly affects the lower third molars. During eruption, the tooth is covered by a flap of gingival (gum) tissue, the operculum. This can result in the formation of a pocket, which may act as a food trap and provide a favourable environment for anaerobic bacteria. The flap can be traumatised by the opposing tooth and become inflamed. The most common symptom is pain associated with a partially erupted tooth. When the operculum is inflamed it may be possible to express pus or food debris from beneath the flap. The degree of systemic upset is variable. There may be trismus (difficulty opening the mouth), lymphadenopathy (swelling of the regional lymph nodes) and spread of infection to the adjacent fascial spaces.
Alveolar osteitis (dry socket) occurs when there is loss of the healing blood clot formed at the time of tooth extraction. This results in a local osteitis (inflammation of the bone) of the extraction socket. It is characterised by a distinctive pain (often described as a toothache getting worse after the tooth has been removed) and an offensive smell; diagnosis and treatment of alveolar osteitis (dry socket) are described in our sections about bone lesions.
Acute periodontal disease (inflammation of soft and hard tissues supporting teeth) is much less common than chronic periodontal disease, which is universal. It is being seen much more frequently in people with impaired host defence mechanisms such as those with human immuno-deficiency virus (HIV) infection (see below). Acute periodontal disease tends to be an exacerbation of underlying chronic periodontal disease.
Necrotising ulcerative gingivitis is a painful and typically spreading, unpleasant inflammation and ulceration of the gums. It is most commonly seen in people who smoke and have poor oral hygiene. It may be more common at times of severe stress. Pain is a prominent feature and may prevent adequate intake of food and fluid. There is usually an offensive odour from the mouth and bleeding from the gingivae (gums) following minimal pressure. The interdental papillae (gums) are initially affected with the rest of the gingivae subsequently becoming involved (see Figure 1). There may be marked loss of periodontal support and consequent loss of teeth. Cancrum oris (noma) is an extreme form with marked soft tissue and bony destruction. It is thought that a mixed bacterial infection (spirochaete and fusiform) is the cause. It is particularly common in the horn of Africa region (for example, Ethiopia) where malnutrition and lack of access to simple antibacterials such as metronidazole are an everyday problem.

A dentoalveolar abscess is usually caused by oral microorganisms that reach the periapical tissues (ligament, bone and other tissue near the apex of a tooth root) via the root canal system or via the periodontal ligament. If the bacteria are sufficiently virulent and/or the host defences compromised, then the infection may give rise to a dentoalveolar abscess.
A dentoalveolar abscess may remain localised or may spread giving rise to a severe cellulitis involving multiple tissue spaces (see Figure 2). The specific signs and symptoms depend on which tissue spaces are involved. A variety of organisms are involved in these infections. There is an increasing recognition of the role of anaerobic bacteria, especially streptococci, in these infections.

Infections of the anterior maxilla (front of the upper jaw) may, rarely, give rise to cavernous sinus thrombosis (formation of a blood clot within the cavernous sinus, a cavity at the base of the brain), a condition which still has a mortality of 30 % in spite of antibiotic therapy. The signs of cavernous sinus thrombosis include proptosis (bulging of the eye), chemosis (swelling of the eyelid), impaired eye movements (ophthalmoplegia) and marked systemic upset.
Acute osteomyelitis is an inflammation of bone of infective origin.
The oral cavities of all animals, including humans, are full of bacteria. Any bite wounds therefore are inoculated with significant numbers of bacteria. This predisposes to infection, particularly if there is a significant injury. The infecting organisms depend on the source of the bite. The most common isolates from infected dog and cat bites are pasteurella species, streptococci, staphylococci, moraxella, neisseria and anaerobes such as fusobacteria and bacteroides. The most common isolates from human bites are staphylococcus aureus, eikenella, haemophilus influenza and beta-lactamase producing oral anaerobes.
Acute salivary gland infections (see Figure 3 for an example of an abscess of the parotid gland), diagnosis and treatment, are described on our pages about salivary gland problems / diagnosis and salivary gland problems / treatment.

Impetigo is a spreading bacterial infection of the superficial layers of the epidermis (outer layer of skin), usually caused by beta-haemolytic streptococci or coagulase-positive staphylococci. It frequently follows minor tissue trauma such as scratching of the skin. Initially there are thin-walled pustules, which spread rapidly circumferentially and burst leaving a crusting wound.
Erysipelas is a superficial cellulitis involving the dermis (thick and dense inner layer of skin) and is most commonly caused by beta-haemolytic streptococci. The lesions spread rapidly and systemic upset is common. Desquamation (shedding of the outer layer) of the skin following resolution of the infection may occur.
Furuncles and carbuncles belong to a variety of conditions caused by staphylococcal infections of hair follicles. Localised superficial infection of a hair follicle is known as folliculitis. If abscess formation occurs, this is known as a furuncle or boil. These are very painful and may require drainage if they do not spontaneously discharge. Multiple adjacent follicles can be involved and if these coalesce this is known as a carbuncle. A furuncle localised to an eyelash is known as stye. These infections frequently recur because of a reservoir of staphylococcus aureus in the nares (nostrils), and eradication of this reservoir is important. Sebaceous and acne cysts may become similarly infected.
Cat scratch disease is caused by bartonella henselae, formerly called rochalimaea henselae. The infection is usually self-limiting, but may last weeks to months. Afipia felis has also appeared to be involved in causation. Regional or solitary lymphadenitis (swelling of lymph nodes) is seen at or near the site of the injury, sometimes with erythematous (red) skin papules. Fever, malaise, and other constitutional symptoms may also occur. In immunocompromised people the infection can disseminate and cause a serious systemic illness.
Only some people recall and report a cat scratch; it is likely that the identical illness can be caused by other animals and even by splinters and thorns bearing the causative organisms. Cats are rarely the carrier. Appropriate serology testing may aid in the diagnosis and management of the infection.
Chronic bacterial infections
There are recurrent (especially in children) and chronic forms of bacterial infections of the salivary glands; these are described on our pages about salivary gland problems / diagnosis and salivary gland problems / treatment.
There is a wide and bewildering range of chronic bacterial (and non-bacterial) forms of osteomyelitis; these conditions are described on our pages about bone lesions / diagnosis and bone lesions / treatment.
Actinomycosis is an infection caused by actinomyces israelii, a common oral commensal (normally non-harmful) bacterium which can, if inoculated into deeper tissues, cause disease. It may be inoculated during trauma such as tooth extraction or fracture of the mandible. Actinomycosis rarely presents as an acute soft tissue swelling (similar to a dental abscess). Pain may be less of a feature than in a simple odontogenic (tooth related) infection. It more frequently presents as a slowly progressive mass, which may not be painful (see Figure 4).

Suppuration (oozing of pus) can occur via multiple tracts. These may resolve, only to recur later. Bone involvement is characterised by deep-seated pain, low-grade pyrexia (fever) and paraesthesia (disturbed sensation).
Serial radiographs may show variable areas of destruction with variable amounts of bone deposition. Diagnosis is by culture of any pus present or biopsy of the involved tissue. Actinomyces are fastidious (fussy) anaerobes and careful, prolonged anaerobic culture needs to be carried out to confirm the diagnosis. Actinomycosis is increasingly thought to be associated with a specific, medication-related form of necrosis of the jaw bone.
Mycobacterial infections, both tuberculosis and atypical mycobacterial infection have become more prevalent in recent years. They are seen in homeless, in chronically malnourished and in immunocompromised people, particularly those with HIV infection. Atypical mycobacterial cervical lymphadenitis (inflammation and swelling of neck lymph nodes) is seen regularly in otherwise healthy children.
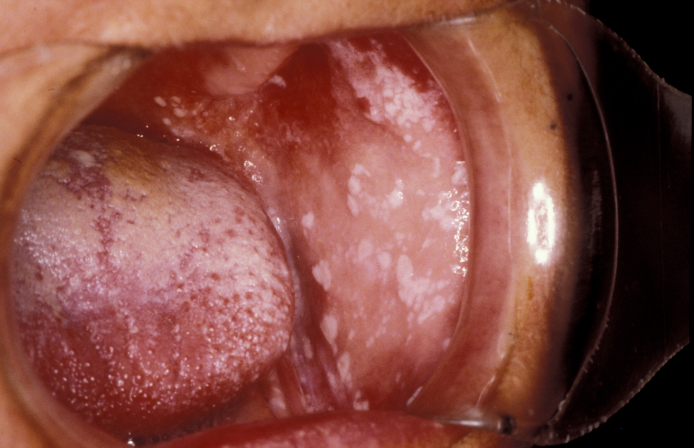
Maxillofacial manifestations of tuberculosis include cervical (neck) lymphadenopathy (in which the lymph nodes may coalesce and give rise to a discharging sinus), chronic oral ulcers, typically of the tongue (see Figure 5) and rarely osteomyelitis. Diagnosis can be difficult and may require multiple bacterial cultures, skin testing, chest X-ray imaging and occasionally biopsy.

It is of immense importance not to confuse the quite common cervical lymphadenopathy of atypical mycobacterial infections (mycobacterium avian-intracellulare complex, mycobacterium kansasii, mycobacterium marinarum) with tuberculosis. These atypical mycobacterial infections do not respond to anti-tuberculosis therapy, rarely show any of the other manifestations of tuberculosis, and are treated quite differently.
Atypical mycobacteria, such as mycobacterium aviium-intracellularae (and many others) may give rise to an isolated, occasionally discharging cervical mass in children (sometimes called a ‘scrofula’ or ‘the king’s evil’: it was believed in the middle ages that the condition could be cured by the touch of the king; see Figure 6) Diagnosis is by culture and microscopy.

Syphilis is a sexually transmitted infection that may have oral manifestations at any point in its natural history. It is caused by the spirochaete bacterium treponema pallidum.
In primary syphilis there is a painless ulcer, known as a chancre, at the site of entry of the infection. This might be at an intraoral site, with the lip, tongue and gingivae (gums) the most common areas. Chancres are highly infectious and may persist for up to a month. Approximately six weeks later secondary syphilis may present intraorally as ‘snail-track’ ulcers of the mucous membrane (lining tissue of the mouth). The infection may become latent for 5 to 10 years. The classic lesion of tertiary syphilis is the gumma (a rubbery, soft growth), which may affect the palate, lips and tongue. Considerable destruction may occur. There can be an associated glossitis (inflammation of the tongue) which may be premalignant (risk of developing a malignant lesion.
Syphilis infection in utero (of the unborn) gives rise to congenital syphilis. As a result, there may be hypoplasia (underdevelopment) of the permanent teeth giving rise to notched, peg-shaped incisors (Hutchinson’s incisors) and rounded first permanent molars (mulberry molars). Gumma formation may cause collapse of the nasal complex and a ‘saddle nose’ deformity. Diagnosis is by serology.
Viral infections
Acute viral infections
A particular type of RNA paramyxovirus causes mumps, most commonly seen in childhood. It is characterised by a painful swelling of the salivary glands, particularly the parotid. It is usually bilateral. There is frequently trismus (difficulty opening the mouth) and halitosis (bad breath). Although mumps is usually self-limiting complications can occur, especially in adults. These include orchitis (inflammation of the testicles), meningoencephalitis (inflammation of the membranes of the brain and adjoining cerebral tissue), myocarditis (inflammation of the heart muscle) and nephritis (inflammation of the kidneys).
Epstein-Barr virus infection most commonly presents as infectious mononucleosis (glandular fever). It is transmitted by contaminated saliva. It is also associated with nasopharyngeal carcinoma , lymphoma and hairy leukoplakia. Infectious mononucleosis is most commonly seen in adolescents and young adults and presents as malaise, sore throat and cervical lymphadenopathy. There may be an associated hepatosplenomegaly (enlargement of liver and spleen). Intraoral examination may show multiple petechiae (red spots from bleeding in the skin; see Figure 7). The condition is self-limiting. In Germany it is sometimes referred to as ‘Pfeiffer’s disease’ and in many countries ‘kissing disease’ because of the mode of transmission.

Cytomegalovirus infection may present as mucosal ulceration or salivary gland swelling in people who are immunocompromised. Diagnosis may require biopsy of the affected tissue and special staining of the specimen.
The class of coronaviruses comprises a large family of RNA viruses and recently a newly emergent species of this type of virus, SARS-COV-2 has caused a pandemic (which at the time of writing, autumn 2020, is far from being controlled and causing immense societal, economic and general health-related burden all over the planet).
Because of this situation, we add a short section here about
- some general properties of coronaviruses;
- the current understanding of transmission paths of SARS-COV-2 and aerosols;
- the current understanding of symptoms of COVID-19.
The large class of coronaviruses are all RNA viruses, with their genome encoded in a single strand of RNA. The many different coronaviruses have several structural features in common (Figure 8). They are typically spherically shaped with a diameter of approximately 120 nm, with an envelope consisting of a lipid (fatty) bilayer, and a set of approximately 20 nm long, petal-shaped spikes at the fringes. These spikes consist of glycoproteins; they are especially relevant for the specific infectivity of a particular type of virus and have relevance in the context of vaccines and monoclonal antibodies). The inside of the coronavirus structure is made up of the RNA genome and one type of nucleocapsid protein.
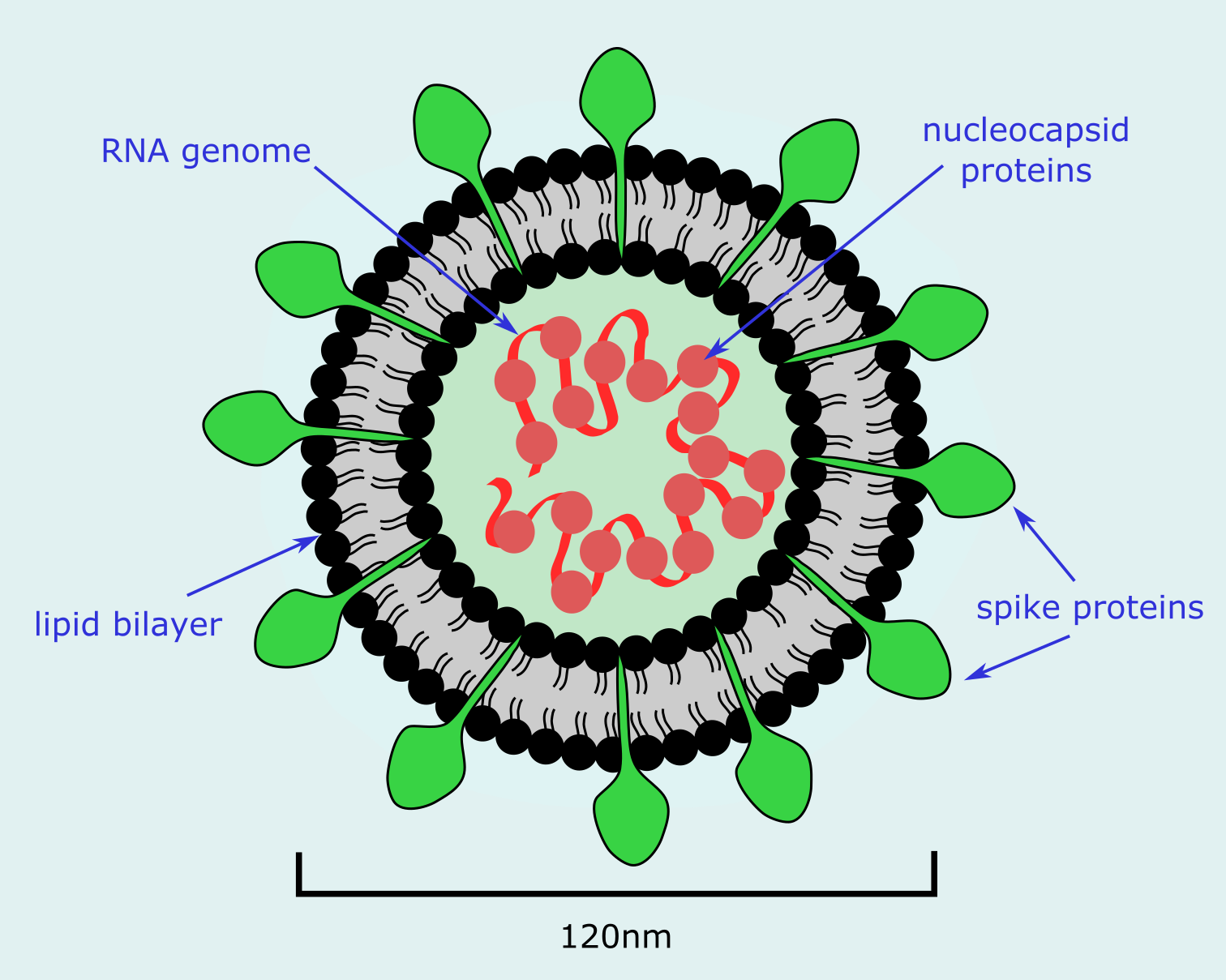
The spikes on the surface of the virus are responsible for attaching to the host cells and infecting them. This fusion of virus and host cells is the main target of the host’s acute immune response. The nucleocapsid protein is thought to regulate aspects of the viral RNA synthesis. Coronaviruses have large, single-stranded RNA genomes. Such large RNA genomes generate diversity of the respective virus family by common mutations, despite some safe-guarding mechanisms to avoid errors in replication. Mutation is important for the ability of any virus to adapt optimally to its sole ‘programmed’ purpose – replicating its RNA (or DNA for some other viruses) by spreading to new hosts. If a virus is highly contagious, it will spread easily. But if it is simultaneously lethal for the host, this will quickly terminate the virus propagation too. From the point of view of a virus, ideally it should be highly infectious but not too lethal for the host, and infection should not produce long-lasting immunity in the host after recovery.
Coronaviruses have an exceptionally large pool of viral hosts. Most animals (including humans) and many plants are susceptible to infections by some type(s) of coronavirus, with a fair amount of cross-species infections documented. As far as humans are concerned, the best-known coronaviruses include those causing the common cold, the group leading to seasonal influenza, in recent years the species causing SARS (severe acute respiratory syndrome) and MERS (middle eastern respiratory syndrome), and most recently SARS-COV-2 causing COVID-19. Most coronaviruses are ‘specialists’, causing characteristic patterns of disease (often respiratory conditions, but neurological and some gastrointestinal conditions are also common). The species and tissue specificity is related to the properties of host cell receptors and the spike proteins on the virus surface. Coronaviruses can replicate in the cytoplasm (the thick liquid inside cells) of many cell types.
The current understanding of the transmission paths of SARS-COV-2 is incomplete. Initially it was assumed that transmission occurs by direct person-to-person droplet infection (similar to the transmission of other coronaviruses causing respiratory diseases) as well as via contaminated surfaces (fomites; SARS-COV-2 has been found to survive on a range of surfaces for considerable periods of time). In that scenario, precautions such as physical distancing, face covers, coughing & sneezing etiquette, and meticulous hand hygiene make perfect sense. In particular, washing hands with soap or detergent is highly effective, as fortunately the lipid bilayer coating of the virus capsule is destroyed by this simple measure. Since the early days of the pandemic it has become increasingly clear that for SARS-COV-2 a further indirect transmission path is relevant: transmission via aerosols; a well-known example of aerosol transmission of a highly contagious virus is rubeola, causing measles. In that respect, suitable mouth and nose covers are an important precaution. This is particularly important as transmission of SARS-COV-2 can occur from asymptomatic carriers, combined with an average incubation period of a week, up to two weeks. It is not straightforward to clearly distinguish these different transmission paths from each other, so for the time being the relative importance of direct transmission by relatively large droplets and indirect transmission by small particles in aerosols is not known. This combination of factors regarding transmission and the initial (perhaps reasonable) assumption that SARS-COV-2 was primarily a respiratory pathogen, underpinned the disastrous responses to the disease COVID-19 in many developed countries.
An aerosol is a suspension of small liquid or solid particles (smaller than 1 μm) in a gas phase (such as air). Such tiny particles can remain suspended over long periods of time and can travel a fair distance in an enclosed space. How exactly such an aerosol ‘cloud’ behaves is determined by external conditions (temperature, humidity, ventilation and gas/air circulation dynamics, gravity, electrical charges) as well as by the properties of the suspended particles (such as size, shape, density, chemical reactions, evaporation and coagulation). If such suspended particles are virus bearing, and the external conditions are suitable to preserve the active virus, then indirect transmission by breathing in aerosol-rich air is a distinct possibility. This mechanism may also be relevant with respect to disease development following infection: such tiny particles can travel deep into lung tissue directly (whereas larger droplets initially will only travel to the nose and throat). A benign application of aerosols is, for example, the rapid delivery by inhalers of very finely dispersed agents to relieve asthma symptoms and to treat other respiratory diseases.
Circumstantial evidence pointing to indirect transmission of SARS-COV-2 via aerosols includes observations of large infection clusters, for example in meat-processing facilities (moist and cold environment), large social gatherings in enclosed spaces (ranging from now infamous après-ski parties to religious ceremonies, singing in a choir, fitness studios and restaurants), and a significantly reduced transmission rate outdoors. Even normal talking and breathing leads to the exhalation of aerosols. However, it is not yet clear which concentration of viable SARS-COV-2 in an aerosol is necessary to cause infection in somebody breathing in the aerosol. Furthermore, the current experimental evidence about SARS-COV-2 concentrations in the air in, for example, hospital settings caring for COVID-19 patients is slightly conflicted.
Where aerosol transmission plays a role, this has implications for precautions in many regards. Ventilation of enclosed spaces is important, as is minimisation of extended meetings in enclosed spaces and/or in close proximity, and optimisation of air conditioning with rapid replacement of air rather than circulating air. Mouth and nose cover plays an important role in this context. Different types of face masks offer differing degrees of protection. Reusable fabric masks and surgical masks mostly reduce the amount of particles, especially larger droplets, in exhaled breath, with surgical masks made of non-woven materials being slightly more efficient. Both mostly protect others rather than the person wearing them and are, thus, most effective if everybody uses them. Medical grade respiratory masks (FFP2 masks) protect the wearer; they are made from dense materials that can filter very small particles when inhaling, including most viruses. These respiratory masks, together with other appropriate personal protective equipment, are necessary for the safe execution of so-called aerosol generating procedures such as many dental and oral surgery interventions, maxillofacial surgical oncological treatment, facial trauma surgery, drainage of cervicofacial infection, surgical airway or intubation. This is well established, and a routine part of such interventions also in ‘normal’ times. Several studies have demonstrated that the risk for clinicians with appropriate personal protective equipment when treating COVID-19 patients is low. This raises some questions as to the wisdom of halting all dental and many other treatments in the UK for many months. In contrast, healthcare workers working in supposedly low(er)-risk environments and not using full personal protective equipment are at much higher risk. This can be easily understood: some infective SARS-COV-2 carriers may be asymptomatic and/or untested and normal speaking and breathing produces aerosols, enough to transmit SARS-COV-2 when in close proximity for extended periods of time.
Initially it was thought that SARS-COV-2 infection leads to a form of respiratory syndrome. In line with this idea, early in the pandemic only symptoms of a persistent cough, shortness of breath and fever were taken as indicative of COVID-19. Whilst these are common, there are other significant symptoms. Oxygen depletion has been observed even in the absence of shortness of breath, a common symptom is loss of sense of taste and smell (anosmia, often severe), and other common symptoms are fatigue and severe headaches, skin rashes and gastrointestinal problems have been reported. It seems that patterns of symptoms in children are different from those in adults, with fatigue, gastrointestinal problems and lack of appetite more common in children (unless they are asymptomatic when infected with SARS-COV-2, which may well be common).
It quickly emerged that COVID-19 does indeed cause severe lung damage (as seen in characteristic MRI scans of the lungs and in post mortem autopsies) but it also became clear that COVID-19 is not restricted to respiratory damage. In particular, it can cause a dysfunctional immune response (cytokine storm, similar to some signs and symptoms observed in sepsis) with widespread clotting abnormalities and multiple thromboses, including strokes. It is highly likely that hypoxia (oxygen depletion) is related to the immune response. Kidney failure is also commonly observed. Severe forms of COVID-19 mostly affect elderly people. It is still unclear why some people get infected and only suffer mild or no symptoms, whilst others suffer severe forms of COVID-19. Some initial genomics investigations of several hundred patients point to a correlation of severe forms with a genetic mutation in these people that causes a lack of interferon synthesis (interferons are messenger molecules that trigger the immune response against viral infections). Intriguingly, in some severely ill people auto-antibodies (antibodies that are wrongly targeting ‘self’) against a particular interferon have been observed. One repeated epidemiological finding is that obesity is a significant risk factor for developing severe COVID-19 symptoms and death. In many other apparent associations, confounding factors have later developed. Many deaths appear to be a form of bringing an end of life that was close nearer by developing COVID-19. Obviously, it will be several years before this can be confirmed with a high degree of certainty.
It is now emerging that following SARS-COV-2 infection, at least in the mid-term many suffer long-lasting effects such as fatigue, persistent shortness of breath, or cardiac problems many weeks after infection and initial recovery (termed ‘long COVID’). It is too soon to see what long-term effects COVID-19 may have and how common these may be. It is also too soon to have robust estimates about mortality rates. But some initial conjectures about adverse outcomes can be had from excess deaths which vary strongly between countries. There are correlations with effective test and trace strategies, with systematic preparedness for pandemics in general, with accessibility of health services, and with the levels of stress some health systems have already been under before the outbreak of the SARS-COV-2 pandemic.
Update autumn 2021 — Since autumn 2020 it has been shown conclusively that the by far predominant pathway for transmission of SARS-COV-2 is by aerosols. This leads to a few simple conclusions:
- it is a very good precaution to wear a FFP2 (or equivalent) mask in all enclosed or crowded spaces; this protects the wearer and everybody around them (simple fabric face covers are ineffective and surgical masks do not protect the wearer);
- optimal ventilation of enclosed spaces is essential to minimise infection risks;
- it is a very good precaution to move as many activities as possible to outdoor spaces.
More evidence has been accumulated that PCR (or LAMP) tests are considerably more accurate than lateral flow (rapid antigen) tests; the latter can have high error rates, especially false positive results. To reduce transmission rates, an effective test and trace system, followed by isolation (and support for people to enable quarantine) is an important mechanism.
More information is being accumulated continuously regarding long-lasting effects of COVID-19 disease (‘long COVID’), including prolonged loss of smell (anosmia) and/or taste (dysgeusia), fatigue, breathlessness, brain fog and other cognitive deficiencies, kidney failure and strokes. The acute phase of COVID-19 is a multi-organ pathological process (in those who are vulnerable). It is now clear that its long-lasting effects (exceeding 6 weeks) are varied and also impact different organs. It is too early to quantify these effects, suffice to say that for the moment there is no effective treatment or cure for ‘long COVID’.
With vaccinations having started in many parts of the world early in 2021 and very large numbers of people having recovered from a SARS-COV-2 infection, over the past year it has become clear that immunity both from infection and the current vaccines does wane over time, with noticeably reduced immunity approximately six months after infection or vaccination. Over time more people have been re-infected and in keeping with ever increasing numbers of vaccinated people, the numbers of infections in vaccinated people continuously increase (break-through infection). This is to be expected as no vaccine is 100 % effective. At the time of writing, it seems clear that vaccination does not completely break transmission of SARS-COV-2 but greatly reduces it. Vaccination is highly effective at avoiding serious disease from infection in the vast majority of vaccinated people.
Secondary bacterial or fungal infections during or after treatment for serious cases of COVID-19, especially in conjunction with prolonged ventilation, high doses of corticosteroids and diabetes have been reported. A particularly serious form of a life-threatening, secondary fungal infection, mucormycosis, has been reported mostly on the Indian subcontinent.
Whilst not absolutely conclusive, all existing evidence (mostly from genetic finger printing) is very strongly supporting the view that the SARS-COV-2 wildtype is not a man-made pathogen. However, it remains unclear where and how the virus entered a human infection chain (with the most likely course of events being early transmission from an animal host to humans (a zoonotic infection); in line with the observation that numerous animal species are susceptible to infection with SARS-COV-2, although inadvertent transmission from laboratory has not and cannot be completely excluded). Having a large reservoir of potential host species is one of the reasons why at the moment it seems unlikely that SARS-COV-2 can be completely eradicated any time soon.
The past year has also seen the emergence of a number of virus variants of interest (new but not of clinicopathological significance) and concern (of significance). Those virus variants of concern are problematic because of increased transmission and slightly reduced protection by vaccines that were all designed based on the properties of the original SARS-COV-2 wildtype.
Chronic viral infections
Herpes virus infections are infections caused by a group of DNA viruses and are all characterised by a capacity for latent infection and subsequent reactivation, particularly at times of stress or immunocompromise. The herpes virus family (human herpes virus) include: herpes simplex, varicella-zoster, Epstein-Barr, cytomegalovirus and Kaposi’s sarcoma virus.
Herpes simplex infection is the most common herpes infection, with most people exposed to it by puberty. Most initial exposures are symptomatic. Primary infection can be manifest as a gingivostomatitis (painful gum inflammation), with vesicles, ulcers and oropharyngeal (sore mouth and throat) pain (see Figure 9).

This is often misnamed as ‘teething’ in children, primary infection tends to be more troublesome if it occurs in adult life. Treatment of the initial infection is symptomatic. Following the initial infection, the virus travels to the regional ganglia (clusters of nerve cells that form part of the sensory and autonomous nervous system). From here reactivation is common. In the maxillofacial region these reactivations are seen as mucosal (lining of the mouth) and labial infections (cold sores, canker sores). A prodrome (early symptom) of tingling is common. These lesions are uncomfortable, unsightly and highly contagious. Diagnosis is usually clinical although viral culture and cytology are possible. The infection is transferable to the genitals and vice versa.
Primary varicella-zoster infection gives rise to chickenpox. This is a common contagious disease of children. The symptoms are fever, malaise and a rash, which spreads rapidly from the trunk to the head, neck and extremities. The rash gives way to vesicles and papules. These can involve the oral cavity and make eating and drinking difficult. The infection tends to be self-limiting and complications such as pneumonia and encephalitis are uncommon.
The varicella-zoster virus remains latent in the sensory ganglia and it may reactivate in later life or if someone becomes immunocompromised. This is known as herpes zoster or shingles. Following a painful initial period, vesicles appear which typically have a dermatomal distribution along the divisions of the trigeminal nerve (see Figure 10). The vesicles typically heal over a three week period. Pre-, peri- and post-herpetic neuralgic pain is common and troublesome.

There are a number of viral infections with potential for complicating surgical treatments. Hepatitis B is one of several viral infections which can complicate surgical treatment. The hepatitis B virus is a DNA virus which can be spread by sexual contact or inoculation, particularly in association with intravenous drug abuse. It can be present in saliva as well as in all other bodily fluids. There is a long incubation period, so unwitting infection as a result of inoculation during surgical treatment can occur. This is why the use of universal precautions is so important. Signs and symptoms of hepatitis B infection include: malaise, abdominal discomfort, anorexia and jaundice. Diagnosis is by serology, with detection of the surface antigen (HbsAg) indicating current infection. Liver function tests will show elevation of the enzymes of the transaminase series. Chronic infection with persistence of the infectious state occurs in approximately 5 % of cases. The development of cirrhosis and hepatocellular carcinoma can complicate infection. A vaccine against Hepatitis B is available and all healthcare workers should avail themselves of it.
Hepatitis C is an increasing public health problem. Transmission is similar to hepatitis B infection although hepatitis C is arguably even more easily transmissible, with the highest rate of infection among intravenous drug users. There is no vaccine currently available although some promising treatments have recently been developed. Approximately 20 % of infected people will develop cirrhosis and may require liver transplantation.
There are approximately 34 million people world-wide living with the human immunodeficiency virus (HIV), a blood-borne RNA virus which is spread by sexual contact, or by inoculation with infected blood or blood products. It can complicate oral and maxillofacial surgical treatment both because of the cross-infection risk and because of the oral infection manifestations, some of which may be the first manifestations of the condition and may lead to the diagnosis being made. There is a 2 to 6 week incubation period followed by an episode of flu-like illness. There is then usually a period of persistent generalised lymphadenopathy before the disease enters its latent phase, which may last several years. During the latent phase there is an increase in the viral load and reduction of the CD4 lymphocyte count. Eventually, if untreated with combination anti-retroviral drugs, the lymphocyte reduction will give rise to symptoms and the development of the acquired immunodeficiency syndrome (AIDS). The availability of treatment in various countries and sectors of the world is one of the distinguishing features of the disease in modern times.
Oral conditions associated with HIV/AIDS include: oropharyngeal candidiasis (see below), hairy leukoplakia (see Figure 11), Kaposi’s sarcoma (lesions of the skin or oral mucosa), necrotising gingivitis (see above), periodontitis (see above) and the development of carcinomas or lymphomas (usually non-Hodgkin’s type) and enlargement of the parotid glands.

Infected patients who have reached a stage of significant immunocompromise (extremely rare nowadays in the developed world) may present with severe dentofacial sepsis. The removal of the source of infection may be difficult but is essential. Patients with HIV/AIDS are at risk of bacterial infection during treatment. Prophylactic antibiotics should be used. Universal precautions should be used to prevent transmission of infection but this is hardly unique to HIV.
Fungal infections
Acute fungal infections
Candidiasis (sometimes referred to as candidosis) infection is caused by candida, a yeast-like fungus commonly found in the oral cavity. Candida albicans is most commonly cultured and associated with disease. It is more commonly isolated in smokers, in people with xerostomia and those on broad-spectrum antibiotics or steroids, particularly inhaled steroids. Underlying systemic disease such as diabetes can predispose patients to systemic candidiasis. Candidiasis is sometimes known as the disease of the diseased.
Symptoms include discomfort (often described as burning), altered taste and altered smell. Dysphagia (difficulty swallowing) may be present in oral candidiasis. Pseudomembrane formation is common (see Figure 12) and is characterised by the fact that the plaque can be removed by rubbing, leaving a bleeding site.
An erythematous form may be seen in which painful red areas are present in the absence of plaques. A hyperplastic form may be seen in denture wearers, as may angular cheilitis (inflamed fissures in the corners of the mouth) in which an associated staphylococcus aureus infection may be present. The hyperplastic form of candidiasis if candida hyphae are seen microscopically to invade the soft tissues may give rise to a possibly premalignant leukoplakia.
Diagnosis is largely clinical. Culture alone cannot be relied upon as candida is a common commensal microorganism. Biopsy confirmation may be required in cases of hyperplastic candidiasis. There are less common candida strains (candida dublensii) which are resistant to standard antifungal treatments.