Jaw disproportion
Contents
Common orthognathic surgical procedures
The removal of third molars (wisdom teeth) prior to the orthognathic surgery is commonly performed in order to avoid poor splits. The presence of third molars during sagittal split osteotomies (see below) is not associated with an increased frequency of unfavourable fractures. Concomitant third molar removal in sagittal split osteotomies also decreases proximal segment inferior alveolar nerve (nerve running in a hollow tube in the mandible) entrapment, but only slightly increases overall operating time.
Mandibular procedures
Ramus Surgery
The mandibular ramus is the upward pointing part or the mandible, behind the lower teeth. Most mandibular corrective procedures in some way involve osteotomies (bone cuts) to this part of the mandible.
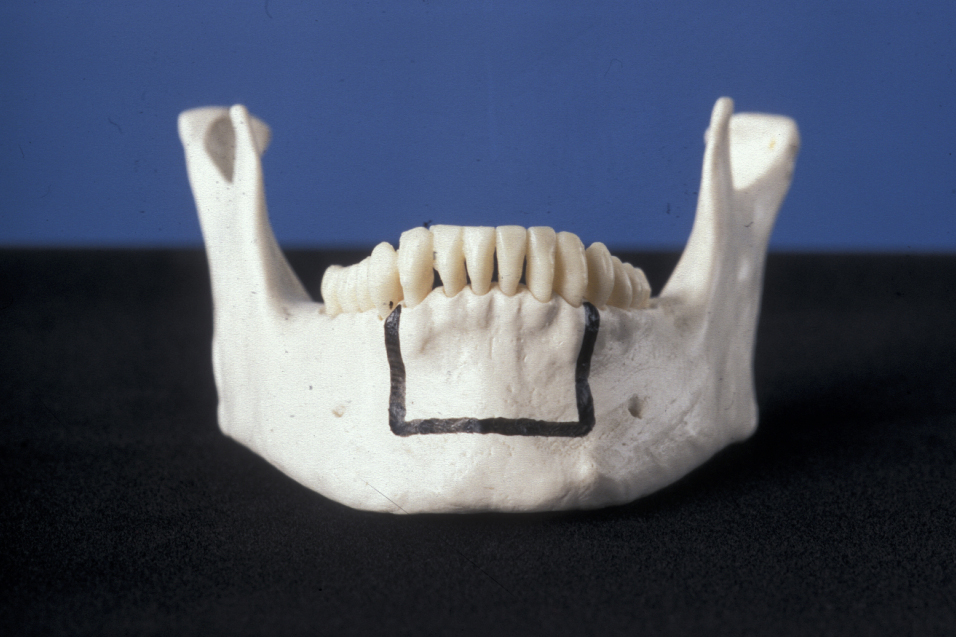
Bilateral sagittal split osteotomy (BSSO) is one of the most commonly performed and versatile mandibular procedures. Figure 1 shows the bone cuts involved.

The bilateral sagittal split osteotomy can be used for backward or forward correction of the mandible in isolation, or in combination with a maxillary osteotomy (see below). It is usually performed under general anaesthesia. It was originally described by Trauner and Obwegeser in 1957. The procedure has since undergone numerous modifications.
Even when there are large advancements, bone grafting is rarely required due to the long bony interface between the two fragments. Indications for its use include mandibular advancement, mandibular setback, and correction of asymmetry. It is contraindicated in ramus hypoplasia, narrow lateral to medial ramus thickness and in severe asymmetries.
There are several advantages and disadvantages to BSSO.
Advantages:
- the mandible can be advanced, set back or rotated in an axial plane to allow correction of asymmetry;
- rigid fixation can be employed, allowing early mobilisation of the mandible and easier management of the airway;
- healing is rapid with predictable bony union;
- good stability.
Disadvantages:
- unfavourable mandibular splitting may occur, such that rigid fixation is impossible;
- an incidence of inferior alveolar nerve damage which can lead altered sensation of the lower lip. Although this is usually temporary, permanent loss can occur. Interestingly, lingual nerve problems are rarely encountered.
Vertical subsigmoid osteotomy (VSS) is a relatively simple and rapid osteotomy (Figure 2).

VSS can be approached either extra- or intraorally. However, for intraoral VSS specialised equipment is required, although this is not unusual in most centres in the developed world. The procedure involves making a vertical cut from the sigmoid notch to the angle of the mandible/antigonial notch. In essence, a large condylotomy is performed to allow the mandible to be set back. The main indication for VSS is for mandibular setback when the movements are small. It can be a good alternative to the BSSO (see above). Larger movements may require coronoidectomies (further bone cuts to remove the coronoid process of the ramus of the mandible). VSS can be used to correct asymmetries where the mandible is set back on both sides. It cannot be used for mandibular advancements unless bone grafting is also used.
VSS has several advantages and disadvantages.
Advantages:
- rapid and easy procedure;
- excellent for small setbacks.
Disadvantages:
- without the specialist equipment for intraoral rigid fixation (right-angle drills and screwdriver), intermaxillary fixation is required for about six weeks;
- difficult to control condylar position;
- extraoral approach (which does allow fixation) will leave visible scars;
- bony union may take longer to achieve;
- in correcting asymmetries, if one fragment needs advancement when it was anticipated it would require a setback, VSS has no flexibility.
Inverted-L osteotomy is a relatively rare operation in most practices (Figure 3).

Inverted-L osteotomy is very similar to VSS in its approaches, indications, contraindications, advantages and disadvantages. It is said that ramus elongation or advancement can occur if the inverted-L osteotomy is used in conjunction with a bone graft. Occasionally rigid fixation is possible.
There are several general and specific complications of ramus surgery.
General complications:
- bleeding;
- infections;
- non-union or delayed union;
- malunion.
Specific complications:
- nerve damage;
- unfavourable splitting;
- condylar distraction (condylar sag);
- relapse, both early and late;
- temporomandibular joint (TMJ; jaw joint) dysfunction, oedema, haemarthrosis;
- tooth extrusion;
- periodontal problems.
Mandibular segmental procedures
These operations are designed to alter dentoalveolar segments. The indications for these operations are probably reducing as orthodontic treatment can manage most problems.
Anterior subapical osteotomy (Köle procedure) is performed anterior to the mental foramina, usually from canine to canine (Figure 4).
Vertical osteotomies are placed interdentally and are joined by a horizontal cut below the apices of the teeth. An obvious prerequisite is space between teeth to allow instrumentation without damage.
Posterior subapical osteotomy and total subapical osteotomy are very difficult procedures with very few indications. The inferior alveolar nerve and vessels are at great risk, along with the tenuous blood supply and risk to the tooth root apices. These procedures have little to recommend them.
Genioplasty procedures are used to move the chin. The chin can be moved forwards, backwards, rotated, reduced or increased in height (Figure 5).
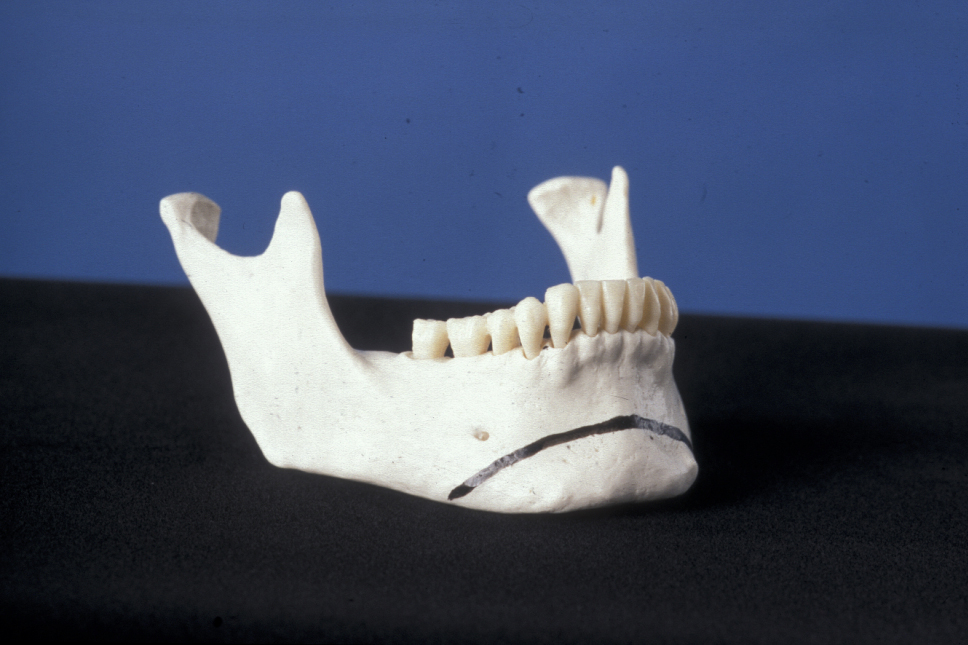
Genioplasty can be performed with a mandibular procedure or secondarily. These operations are not without risks (such as mental nerve damage), which must be born in mind especially when genioplasty is combined with BSSO (see above). If combined with a sagittal split osteotomy, the genioplasty is performed after the BSSO. It is easier if intermaxillary fixation is maintained while the genioplasty is carried out.
Alloplastic augmentation (with a range of bone filer materials) is advocated because of its simplicity and lesser degree of postoperative pain, oedema and ecchymoses (bruising) which leads to a faster recovery. Occasionally, patients who present for aesthetic chin surgery do not have a severe dentofacial deformity and have class I occlusion and retrogenia (receding chin). These patients desire an increase in chin projection, which can be accomplished with an alloplastic implant or a sliding osseous genioplasty. Implants are suited for small advancements on the order of 4 to 5 mm, usually as part of a face-lift procedure. The sliding osseous genioplasty can be used for shorter as well as longer advancements and it is especially suited for vertical height alterations. The implants are susceptible to infection, more so than the hardware used in osseous genioplasty. Migration and deep bony erosion are complications unique to these implants. Erosion can be limited by placing the implant low over the thicker cortex of the inferior mandible, having at least 9 cm of surface area of the base of the implant to disperse pressure, and by placing at a minimum the central position of the implant superficial to the periosteum.
Maxillary Procedures
Maxillary deformities will occur in anteroposterior, transverse, and vertical planes. The maxillary Le Fort I osteotomy is a versatile procedure which can address all these problems. Thus, once mobilised, the maxilla can be repositioned in any plane. The stability of these moves is variably predictable.
The maxilla can also be segmented allowing levelling, narrowing or widening of the upper arch. The approach is via a horseshoe buccal vestibular incision. Preservation of the palatine vessels is thought by some surgeons to be essential, but many operators ligate these vessels or us diathermy if required, with no apparent compromise to the vascularity of the maxilla.
The bony cuts for Le Fort I osteotomy are a straight line starting a few millimetres above the floor of the pyriform aperture continuing backwards just above the tooth root apices to the zygomatic buttress and back to where they contact the pterygoid plates (Figure 6).
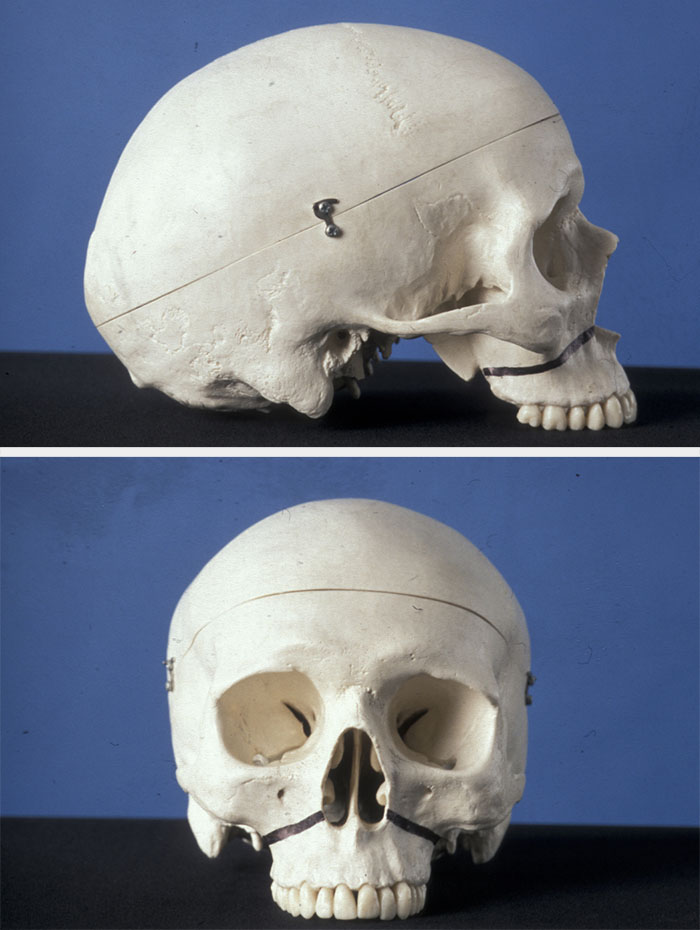
This Le Fort I design tends to slope downwards from front to back; thus in moving the maxilla forward, it will tend to move upward as well. Similar cuts are made along the lateral nasal walls (medial wall of maxillary sinus), and the nasal septum is freed from the nasal surface of the palate (nasal floor). Pterygoid disjunction is finally performed before down fracture of the maxilla. Variations to these cuts are described, but they are essentially variations on a theme. Some operators step the lateral cuts in the buttress region with a vertical cut (5 to 10 mm in length), with the horizontal cut then continuing backward to the pterygoid region. This is done in an attempt to prevent the unwanted upward movement. The step also gives a vertical reference point in forward repositioning. The heights of the bony cuts are only limited by the position of the infraorbital nerve. If this is carefully preserved, then even the infraorbital rims can be advanced (Kufner’s modification).
Another variation is the horseshoe osteotomy, which can be done as part of a standard Le Fort I procedure or as a definitive osteotomy. It is indicated in superior movements, especially when attempting to gain a large impaction.
With the advent of modern orthodontic techniques, segmental surgery is seldom indicated.
There are several general and specific complications of maxillary orthognathic surgery.
General complications:
- bleeding; this can be a major problem in maxillary surgery;
- infection;
- non-union.
Specific complications:
- relapse, more likely to occur with downward movements;
- maxillary settling due to inadequate stabilisation, it is a posterior or vertical movement;
- condylar distraction (sometimes called condylar sag);
- nerve injury, nearly always temporary and affecting the infraorbital nerves;
- avascular necrosis - an unmitigated disaster!
Segmental procedures are employed when one or more teeth plus, of course, the supporting alveolus need to be moved and orthodontic correction cannot (for whatever reason) be achieved. Tunnelled approaches via limited incisions to preserve blood supply to the tooth/bone segments are used. This technique makes visualisation and fixation difficult.
The Wassmund-Wunderer procedure allows movement of the upper anterior teeth en bloc. This can reduce an increased overjet, close a small anterior open bite and increase or decrease incisor show. Schuchardt described a posterior segmental osteotomy based on similar principles.
The maxilla can be segmented as part of a Le Fort I osteotomy. The posterior segments can be similarly mobilised as described by Schuchardt.
Surgically assisted rapid palatal expansion (SARPE) is a useful adjunct to either orthognathic surgery or orthodontics alone for maxillary expansion. If the maxilla is significantly hypoplastic in a lateral dimension, it is not possible to expand it orthodontically in order to correct a buccal crossbite. In nongrowing persons, one option is SARPE. This involves making osteotomy cuts (but not fracture and mobilisation) to allow orthodontic expansion by a fixed rapid maxillary expansion (RME) appliance. The extent of the bone cuts varies but should involve the lateral wall of the maxilla and often a mid-palatal split. Separation of the pterygoid plates may sometimes be performed. The fixed RME is expanded at a rate of 0.25 mm twice per day.
Some soft tissue procedures are a common part of orthognathic surgical approaches. These include
- alar base cinch suture (to control the alar base width, which nearly always increases);
- V-Y closure (to reduce lip shortening);
- inferior turbinectomy (reduction of these structures will allow impaction of the maxilla and may prevent postoperative nasal obstruction).
Relapse
Relapse can be defined as movement of osteotomised fragments back to their original positions. There are many factors that are associated with post-treatment relapse, many of which can be anticipated in advance. Good planning and an experienced team can minimise problems and take steps to avoid or limit relapse.
The University of North Carolina has followed up almost 1500 patients who had received surgical repositioning of the jaws for a minimum of 1 year after surgery, with over 500 of these patients reviewed for at least 5 years. This identified highly stable, stable, and problematic procedures.
Highly stable procedures:
- maxilla upward;
- mandibular advancement;
- genioplasty.
Stable procedures:
- maxillary advancement;
- two-jaw surgery for the correction of class II (maxilla up, mandible forward) class III (maxilla forward, mandible set back) conditions.
Problematic procedures:
- isolated mandibular setback;
- maxilla downward;
- widening of the maxilla.
For ease of discussion the factors involved can be broadly classified as surgical, orthodontic and patient-related factors.
Surgical factors
- Size of movement. Movement of the mandible greater than 8 to10 mm, or maxilla 6 mm forwards.
- Direction of the movement. The most stable movements are an advancement smaller than 6 mm in the mandible and impaction in the maxilla. The least stable movement in the mandible is thought to be a setback, and the least stable movement in the maxilla is either a maxillary setdown or expansion.
- Inadequate fixation.
- Distraction of the condylar heads out of the glenoid fossa; this leads to immediate relapse. It should be corrected immediately unless of course the patient is placed into intermaxillary fixation postoperatively, in which case it will be recognised when the fixation is released, which may be too late!
- Poor planning.
- Movements which put the muscle attached to the fragments under tension. This can occur in large movements, and relapse will tend to occur gradually.
Orthodontic factors
- Extrusion of teeth.
- Soft tissue forces such as endogenous tongue thrust, which leads to recurrence of an anterior open bite.
- Tooth movement into a zone of muscle imbalance, which leads to relapse on removal of the appliances.
- Poor planning.
Patient-related factors
- Poor compliance.
- Anterior open bite due to soft tissue factors such as endogenous tongue thrust.
- Cleft lip and palate. It is often difficult to advance the maxilla more than 6 mm without using distraction techniques because of dense scar tissue from multiple surgical procedures, and relapse often occurs.
Surgery for obstructive sleep apnoea (OSA)
Sleep-disordered breathing is increasingly recognized as a potential cause of medical morbidity, with obstructive sleep apnoea (OSA) the most common form of sleep-disordered breathing. It is now appreciated that OSA occurs in a significant number of people, beyond the stereotypical Pickwickian syndrome (obese) person.
In simple terms OSA results in episodes of hypoapnoea/apnoea during sleep resulting from loss of muscle tone of the tongue and pharyngeal musculature which leads to airway obstruction. Oxygen desaturation occurs as a result of this obstruction, and the resulting hypoxia stimulates breathing to correct the hypoxia (at the price of disrupting sleep). This cycle can be repeated literally hundreds of time a night in severe cases and can give rise to symptoms of excessive daytime sleepiness, which can lead to poor concentration and impaired performance. The cycles of hypoxia can have an adverse effect on many physiological functions and may contribute to the development of cardiovascular problems such as hypertension. The severity of sleep apnoea is classified by the numbers of aponeas and/or hypoapnoeas occurring per hour.
Hypoapnoea: a transient reduction (but not complete cessation) of breathing for more than 10 seconds.
Apnoea: complete cessation of breathing for more than 10 seconds.
The apnoea hypoapnoea index (AHI) indicates the number of apnoea and hypopnoea episodes per hour of sleep.
These are measured in a controlled manner during a sleep study, known as polysomnography. This study also looks at the lowest oxygen saturation during hypoapnoeic/apnoeic episodes and limb movements. The results are interpreted by a sleep medicine specialist.
Accepted criteria for severity of OSA based on AHI, calculated during polysomnography are:
mild: AHI 5 to 14
moderate: AHI 15 to 29
severe: AHI 30 or greater.
The Epworth Sleepiness Scale (ESS) is a self-administered survey with which patients score their likelihood of dozing off during a number of daytime scenarios. It is used to assess the impact of sleepiness (which may be secondary to OSA) on daily life.
It is worth remembering that although many healthcare funders (including the UK NHS) exclude ‘simple snoring’ from treatment, even snoring without apnoeic events has a disruptive and potentially destructive effect on many relationships and sleeping arrangements. There is a demonstrated relationship with ESS and measures of relationship harmony.
Management of diagnosed OSA can be divided into medical and surgical management.
The mainstay of medical management is continuous positive airway pressure (CPAP). This involves the patient wearing a special face mask during sleep through which air is provided at an adjustable pressure. This provides a ‘pneumatic splint’ which overcomes the pharyngeal soft tissue collapse and keeps the airway patent. It is considered the standard against which other treatments for OSA are measured but is often poorly tolerated.
In cases of mild to moderate OSA a mandibular positioning appliance can be made by a dentist to position the mandible forward. This has the effect of bringing the tongue muscle insertions forward and helps increase the resting muscle tone, helping to relieve the obstruction.
Surgical management of OSA seeks to relieve obstructions at the level of the obstruction. The sites of obstruction can be nasopharyngeal, oropharyngeal and hypopharyngeal. Accurate determination of the site of obstruction may be challenging. Nasopharyngoscopy is typically used to look for the site of obstruction but is not fully diagnostic. Lateral cephalograms are also commonly used, but they provide a two-dimensional image of what is a four-dimensional situation.
Surgical management of OSA may be directed at soft tissue or the facial skeleton. Surgery on the facial skeleton is based on the techniques of orthognathic surgery. The term telegnathic (‘move the jaws a long way’) surgery has been used to describe the skeletal surgery for OSA. The common procedures used are genioplasty (genioglossal advancement) which is typically done in conjunction with another hard or soft tissue procedure, and maxillomandibular advancement (MMA) which is basically a bimaxillary advancement osteotomy, with or without genioplasty. MMA has been demonstrated to provide enlargement of the retrolingual airway and some advancement of the retropalatal airway. As such it has the capacity to relieve obstructions at multiple levels. The surgery may be done without presurgical orthodontics in many cases, although in some cases orthodontic setup may allow for a greater skeletal movement (the typical goal is to get 10 mm or more of mandibular advancement). There is a mounting body of evidence that MMA is effective and stable. It is increasingly being used as a first line treatment for management of OSA in patients who are unable/unwilling to use CPAP.