Hard tissue necrosis
Signs and symptoms of osteonecrosis of the jaws (ONJ)
The signs and symptoms of osteonecrosis of the jaws (ONJ) include exposure of necrotic bone, ulceration and mucosal (soft tissue in the mouth) necrosis without healing tendencies, accompanied by pain. Depending on the underlying cause, acute symptoms may include swelling, infection or abscess, mucositis, trismus, disturbed sensation. Over time an oro-cutaneous fistula may develop from chronic infection, a pathological fracture of the mandible may occur, teeth may be lost and pieces of necrotic bone (such a piece is called a sequestrum) may be shed, usually through the mucosa.
Even where the underlying cause of ONJ is not a specific infection, the affected areas frequently carry a high load of microbial agents and sometimes show a shift to more specific and pathologic cultures.
The destruction of bone by osteonecrosis of the jaws makes severe ONJ a debilitating condition, leading to serious functional impairment of speech, chewing and eating in general with a background of often intractable chronic pain.
Osteoradionecrosis (ORN)
In spite of improved modulated radiotherapy irradiation schemes, osteoradionecrosis (ORN) remains the most important long-term complication of radiotherapy applied to the head & neck region (apart from further damage such as xerostomia (dry mouth), distorted taste, dysphagia (difficulty with swallowing), reduced mobility of the tongue. The location of the tumour necessitating radiotherapy, as sole treatment modality or after surgery, as well as the radiation dose are correlated with the occurrence and severity of ORN. The risk is increased with higher total dose, larger fraction dosage and larger irradiated volumes,
ORN may occur many years after completion of radiotherapy treatment. This is likely related to the lasting increased vulnerability to the oral mucosa to even minor irritation. After irradiation the risk for soft tissue necrosis of the oral mucosa remains high. For example, ill-fitting dentures can represent an ongoing irritation and thus an increased risk for the development of necrosis.
95 % of ORN occurs in the mandible (the lower jaw bone). It is often associated with extractions of teeth in a previously irradiated mandible. The general dental practitioners and restorative dentistry specialists have an important role in preventing this complication.
ORN can be defined as irradiated bone which becomes devitalised and exposed through the overlying skin or mucosa without healing for three months, without recurrence of tumour.
After clinical examination and taking of a dental panoramic tomography (DPT) image, mandibular ORN cases can be classified as follows (Notani classification):
- ORN confined to the dentoalveolar (immediately surrounding teeth) bone;
- ORN limited to dentoalveolar bone or mandible above the inferior dental canal (hollow tube inside the mandibular bone, housing nerves and blood vessels), or both;
- ORN involving the mandible below the inferior dental canal, and/or pathological fracture, and/or skin fistula.
There are several theories attempting to explain the pathophysiology of ORN.
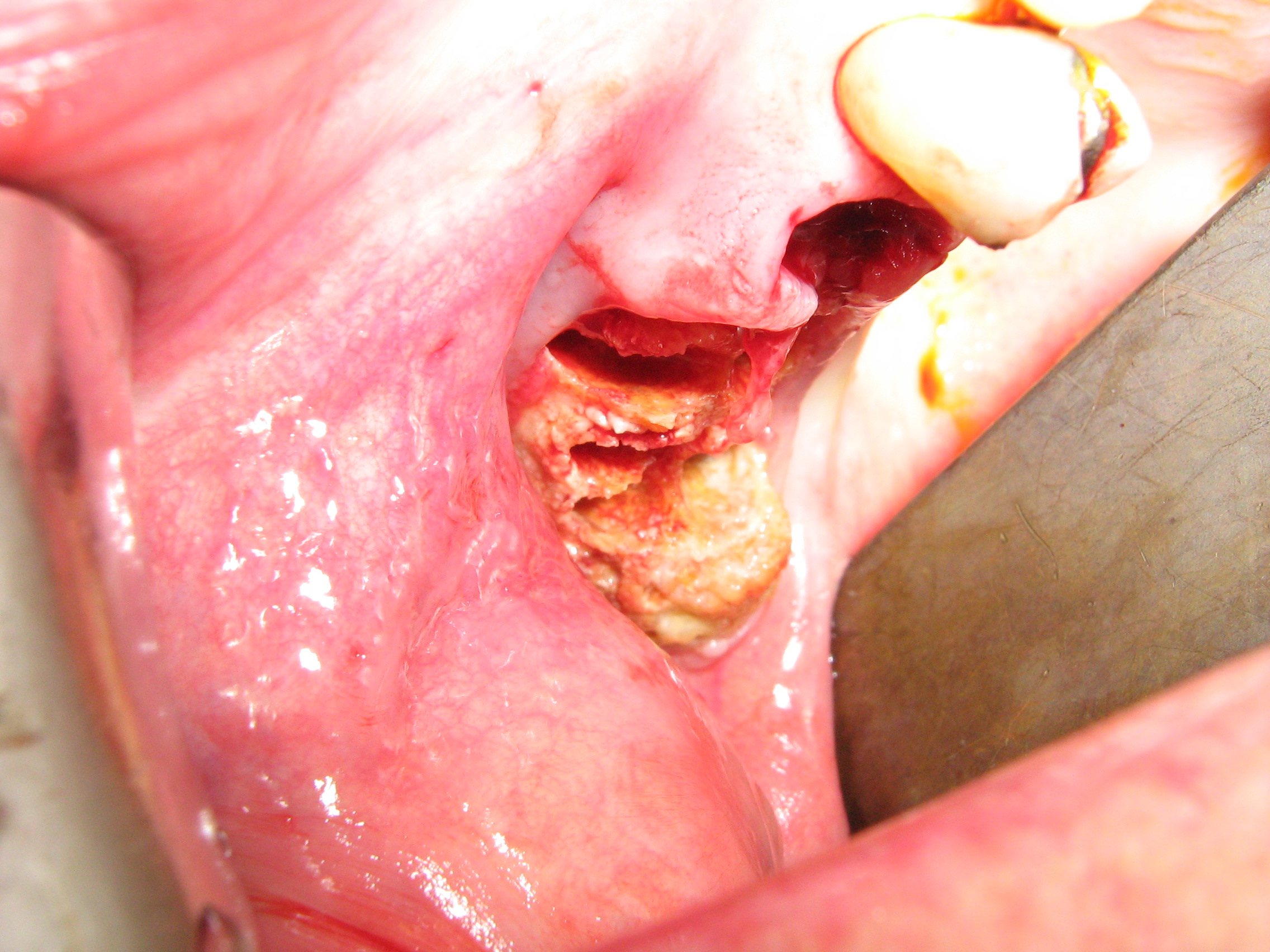
Figure 1, Figure 2 and Figure 3 show examples of different ORN conditions.



Medication Related Osteonecrosis of the Jaws (MRONJ)
A number of drugs can cause medication related osteonecrosis of the jaws (MRONJ). MRONJ is defined by the following criteria:
- presence of exposed bone (or bone that can be probed through an intraoral or extraoral fistula) in the maxillofacial region over a period of 8 weeks;
- current or previous treatment with antiresorptive or antiangiogenic agents;
- no history of radiation therapy to the jaw or obvious metastatic disease to the jaw.
MRONJ is a complication of treatment with antiresorptive agents. These medications are prescribed to treat a number of bone disorders. This type of medication hinders the normal bone remodelling process by interfering in various different ways with the resorption of bone and is thus used for treatments aiming at strengthening bone. There are different types of antiresorptive agents (the group of bisphosphonates, denusomab and an ever increasing number of agents that interfere with the various biochemical signaling pathways involved in bone remodelling) which work by different interactions with the bone remodelling process. MRONJ in the mandible (lower jaw bone) is more common than in the maxilla (upper jaw bone), approximately 2 : 1.
Antiresorptive medications are widely used to treat osteoporosis (brittle bones, in particular in women after menopause); for example, 1.7 million people are on long-term treatment with antiresorptive agents in Germany (2017). The second indication for antiresorptive agents is in the management of bone metastases from a range of malignancies (including breast, kidney, prostate, some brain tumours) or bone deposits from haematological malignancies such as multiple myeloma.
MRONJ has been reported in 1 to 20 % of patients with bone metastases, the rate of MRONJ in osteoporosis treatment with bisphosphonates is much lower, approximately 0.1 to 2 % of patients are affected. However, given the large number of people on long-term treatment with antiresorptive agents, even a small percentage of MRONJ complications equates to a significant number of people suffering from MRONJ. The risk for MRONJ is higher when antiresorptive agents are administered intravenously than for oral delivery. The risk for MRONJ increases with dose and duration of treatment. In particular for treatment with bisphosphonates, MRONJ is a long term risk as these agents become firmly embedded in the bone matrix where they remain for many years (more than 15 years has been reported).
Antiangiogenic drugs are another potential cause of MRONJ. Antiangiogenics are specialized cancer treatment drugs that target the growth of blood vessels feeding a tumour, essentially aiming to starve the tumour. Their mode of action can impact on the vascularization of the jaws and thus lead to MRONJ via an impaired blood supply to the bone.
Chronic exposure to steroids causes osteoporosis but it is difficult to extract evidence for the direct involvement of steroids in causing MRONJ. However, combined with bisphosphonate treatment of osteoporosis, steroids seem to make MRONJ more likely and/or worse.
Similar to the classification of osteoradionecrosis (ORN; see above) there is a clinical staging scheme of MRONJ:
- at risk category: no apparent exposed/necrotic bone in patients who have been treated with either oral or intravenous bisphosphonates;
- stage 1: exposed/necrotic bone in patients who are asymptomatic and have no evidence of infection;
- stage 2: exposed/necrotic bone associated with infection as evidenced by pain and erythema (redness of skin) in the region of the exposed bone, with or without purulent drainage (pus);
- stage 3: exposed/necrotic bone in patients with pain, infection and one or more of the following: pathological fracture, extra-oral fistula, or osteolysis extending to the inferior border of the mandible.
Figure 4 and Figure 5 show examples of MRONJ of the maxilla and mandible, respectively.

Other causes of osteonecrosis of the jaws
Osteonecrosis of the jaws from the two major causes (see above), radiotherapy applied to the head and neck region and systemic treatment with antiresorptive medications is on the rise. It may sound slightly bizarre but the reasons for this significant increase in the number of ONJ resulting from these two causes are actually positive: more people with head and neck cancers live longer, and most people live to older age in general – which increases the probability of having treatment with some antiresorptive agents at some point and live long enough afterwards to be confronted with the unwanted treatment effects. Clearly, better strategies and methods to prevent ONJ would be highly desirable.
ONJ resulting from other causes includes a fair number of different potential causes but altogether they make up a small minority of ONJ cases.
Of these other possible causes underlying osteonecrosis of the jaws, the most prominent ones are a range of infections. These include:
- bacterial infections, including actinomycosis, syphilis, tuberculosis, noma;
- viral infections, including HIV, herpes zoster (shingles);
- fungal infections, including aspergillosis, mucormycosis.
Local or regional invasive growth of malignancies can include the jaws and lead to ONJ. Trauma, be it related to accidents or surgery (for example, following osteotomies (cutting of bone) in orthognathic surgery (corrective surgery for jaw disproportions) or other maxillofacial surgery), can be a cause for ONJ. A range of long term conditions such as diabetes or arteriosclerosis and some haematological disorders carry an increased risk of ONJ development, most likely related to impaired vascular and blood supply to the jaw bones. Chemical irritants can trigger ONJ; examples being the tissue damage caused by long term cocaine snorting, or by sodium hypochlorite, NaOCl, used in dental practice in root canal treatment, when extruded through the apex of the tooth root into the adjacent bone; some materials used as ‘fillers’ in root canal treatment can cause similar problems.
However varied the collection of ‘other causes for ONJ’, there is one unifying aspect. In all these cases treatment / cure of the underlying condition / problem is also curative for the ONJ. This is distinctly different from ONJ caused by radiotherapy or antiresorptive medications. These differences obviously have a profound impact on the treatment and management of the different varieties of osteonecrosis of the jaws.