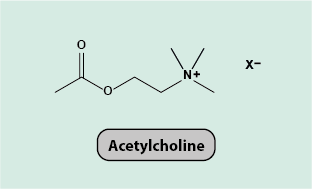
Acetylcholine
Acetylcholine is a small molecule (Figure 1) that has many different functions as a neurotransmitter (a messenger molecule for the functioning of the nervous system and numerous actions of the body triggered by nervous impulses to other cells, including muscle and gland cells, and neurons) in all areas of the body. In the body, acetylcholine is synthesised in certain neurons (so called cholinergic neurons) by the enzyme choline acetyltransferase from choline and acetyl coenzyme A. It is stored in vesicles in cholinergic neurons and released into the synapse by a nerve impulse. Free acetylcholine in the body is rapidly deactivated by the action of the enzyme acetyl cholinesterase.
Acetylcholine itself is not a medication. However, a large number of medications and other drugs interfere in some way with the synthesis, release and/or function of acetylcholine. Given the ubiquitous role of acetylcholine, such agents then carry a potential burden of significant and wide-ranging adverse effects from blocking, mimicking or enhancing the physiological effects of acetylcholine. The only exception where acetylcholine in low dose is actually used as a local medication, is in ophthalmology where in cataract surgery acetylcholine eye drops are used.
One place where acetylcholine acts is at the neuromuscular junctions of the peripheral nervous system. It is released into the synapses between motor neurons and muscle cells. Release of acetylcholine activates muscular contractions in the skeletal muscles and this enables motion. Acetylcholine also acts in the autonomic nervous system, with effects on numerous involuntary and unconscious functions of internal organs. Acetylcholine acts as a neurotransmitter in both branches of the autonomic nervous system, in the sympathetic and the parasympathetic nervous system, with different effects. The sympathetic nervous system uses acetylcholine to cause the release of noradrenaline, which activates adrenergic receptors on target tissues. The parasympathetic nervous system uses acetylcholine to mediate the increasing or slowing of heart rate among other effects.
Acetylcholine is involved in the regulation of the contraction of smooth muscles in the gastrointestinal system (increasing peristalsis) and in the urinary tract, it has effects on the respiratory system, activates the secretions of all glands that are connected with the parasympathetic nervous system, in the central nervous system it aids memory and learning, and has wide-ranging effects on the cardiovascular system where it acts as a vasodilator and down-regulates heart beat rate and contraction of the heart muscle. The acetylcholine receptors in the brain are associated with nicotine addiction: nicotine binds to this type of acetylcholine receptor and acts as an acetylcholine agonist.
Accordingly, any drugs that interfere with this neurotransmitter system can have drastic and dangerous effects, ranging from paralysis to convulsions. Many toxins in nature, produced by plants, animals or microbes, act on the cholinergic system, an example being botulinum toxin causing paralysis. Some medicinal drugs, in particular some antibacterial agents such as clindamycin, some anticonvulsants and some diuretics, reduce the release of acetylcholine.
Some agents act by inhibiting cholinesterase and thus increase the levels of acetylcholine. High doses of cholinesterase inhibitors can cause fatal convulsions. Examples of cholinesterase inhibitors are nerve agents (Sarin) or some pesticides (organophosphates). More benign clinical uses of cholinesterase inhibitors in low doses include the reversal of the action of muscle relaxants, the improvement of muscle activity in some gastrointestinal conditions and the treatment of the autoimmune condition myasthenia gravis (where antibodies inhibit the functioning of acetylcholine at the neuromuscular junctions by destroying the receptors involved). Some symptoms of Alzheimer’s disease may be reduced by cholinesterase inhibitors.