Hyaluronic acid and hyaluronidase
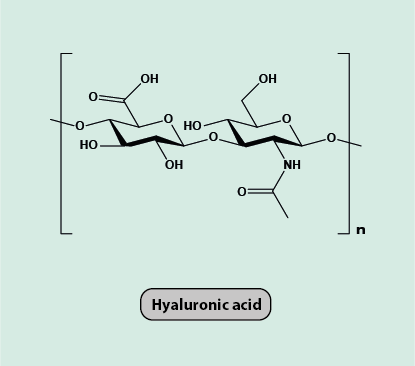
Hyaluronic acid is a component of skin, connective and nerve tissues where it is found in the extracellular matrix (the material surrounding cells) and where it has a number of structural and functional roles, plays a part in wound repair and local immune response and inflammation, and in cell migration (including potential involvement in the metastasis of malignancies). Hyaluronic acid (Figure 1) occurs in the body in the form of highly polymerised, very high molecular weight molecules (the number of repeat units, n (see Figure 1) is such that typical molecular units, depending on the tissue in which the hyaluronic acid is located, will have a molecular mass of several thousand kg/mol). Hyaluronic acid belongs to the chemical class of sugars (carbohydrates; see below), specifically it is a glycosaminoglycan. Hyaluronidase refers to a family of enzymes (catalysts) that are responsible for breaking down polymeric hyaluronic acid molecules during the normal ongoing process of renewal of body components. Hyaluronic acid synthases are a group of enzymes that facilitate the biosynthesis of new polymeric hyaluronic acid in this renewal process.
Properties and function of hyaluronic acid in the body
Similar to other highly polymerised carbohydrates, hyaluronic acid easily accommodates water molecules and swells in the process. Other such examples of swelling by water uptake are the insoluble fibres in foods (related to cellulose) such as wholegrain bread or pulses, helping the digestive process in this way; gelatin derived from animal collagen, turns liquid foods into jellies and acts as a food lubricant. Similar mechanisms underpin the two main effects of hyaluronic acid in the body, to act as a filler and as a lubricant.
The most prominent role of hyaluronic acid in the layers of skin is to act as a ‘filler’ to maintain the extracellular space as a well-hydrated structure. It is thought that the presence of hyaluronic acid in these structures may help to increase the presence of retinoic acid (vitamin A) which, in turn, is thought to protect skin against damage by UV radiation and aging. Excessive exposure to UV radiation (sunburn) further reduces the concentration of hyaluronic acid in skin layers.
Hyaluronic acid has an important function as a lubricant in joints and in muscular connective tissues (the fascia layers). One of the main components of synovial fluids (the fluids inside joint capsules) is hyaluronic acid. There it helps to adjust the viscosity of the synovial fluids such that the cartilage and the joint itself are optimally protected against wear and tear, for example caused by compression.
Closely related to this function as a local lubricant, hyaluronic acid also plays a more general role in enabling and regulating the movement and proliferation of cells. This is important in skin wound healing where initial inflammation, followed by angiogenesis (formation of new blood vessels), granulation (formation of new tissue) and eventually fibrosis (formation of mature scar tissue) are facilitated by the presence of increased levels of hyaluronic acid in wounds. This facilitates the timely transport of the appropriate ‘repair materials’ to actual sites of need in repairing defects in all stages of wound healing, mainly by facilitating the detachment of cells. It is thought that hyaluronic acid supports the healing process by activating and moderating the initial inflammatory response to injury, by facilitating cell migration and proliferation into the wound matrix and by improving the structure of granulation tissue. It has been observed experimentally that hyaluronic acid levels remain high long after the healing of foetal wounds and it has been hypothesised that this may be (one of) the reason(s) why foetal wounds heal without scar formation.
There are some hypotheses about potential involvement of hyaluronic acid in the spread of malignant cells to distant body sites. The argument here is that the mechanisms supported by hyaluronic acid in wound healing may be exploited in the formation of metastases by malignant cells becoming more easily detached from the original tumour site, as well as being helped to establish themselves in a distant site. It has also been noted that concentration of hyaluronic acid is correlated with disease progression in some prostate and breast cancers and its concentration is used as a biomarker in such cases to monitor disease progression. The general / potential role of hyaluronic acid and hyaluronidase in tumour metastasis is a theme that is currently much debated and controversially interpreted, with lots of ongoing research. Another avenue of research in this context is based on the observation that the most common target receptor for hyaluronic acid to bind to the cell surface (a receptor called CD44) tends to be overexpressed in some malignant cell lines. Following these observations, it has been argued that in the future some hyaluronic acid preparations may be used as vehicles (‘nanomedicine’) that transport drugs more selectively to tumour target sites in order to reduce systemic adverse effects while improving drug uptake in malignant tissues.
Medical uses of hyaluronic acid and hyaluronidase
Medical uses of hyaluronidase preparations include its use to reverse the effects of failed or otherwise ‘unloved’ dermal filler / hyaluronic acid injections. Another use is in ophthalmic (eye) surgery in combination with local analgesics to improve pain control.
Medical and cosmetic uses of hyaluronic acid preparations include its common use in skin care products and (in gel form) as an injectable dermal filler to smooth out temporarily facial wrinkles (the effect lasts for a few months). Hyaluronic acid is a component in preparations for the treatment of dry eye syndromes (‘artificial tears’) and for the treatment of dermatitis / dry skin. Injection of hyaluronic acid into joints is a treatment option for osteoarthritis. In maxillofacial surgery this approach is sometimes used to treat osteoarthritis of the temporomandibular (jaw) joint. The evidence base for these intra-joint injections is controversial and there is a risk of severe adverse effects. Other than for its natural role in the processes of wound healing, there is no convincing evidence that applications of hyaluronic acid preparations augment and improve the healing of diabetic ulcers, burn wounds or surgical wounds.