Blood malignancy
The first part of this section outlines maxillofacial signs and symptoms of haematological malignancies. The second part briefly discusses oral and maxillofacial conditions arising during the treatment of haematological malignancies.
We keep this section brief because the exact diagnosis and treatment of haematological malignancies are taken care of by haematological oncology; oral and maxillofacial surgery has a support role in providing diagnosis (and management/treatment) of oral manifestations of these malignancies. More detailed information about all aspects of haematological malignancies can be found in the ample literature about the topic.
Oral and maxillofacial signs & symptoms of haematological malignancies
The oral and maxillofacial signs and symptoms associated with haematological malignancies are incredibly common signs and symptoms for many non-malignant conditions. Thus, only rarely will these be presenting signs of a haematological malignancy. However, along with all their other signs and symptoms, people with haematological malignancies typically have oral signs.
Myeloma affects a type of white blood cells, the plasma cells. Plasma cells are an integral part of the body’s adaptive immune system and are normally involved in the production of antibodies to fight infections.
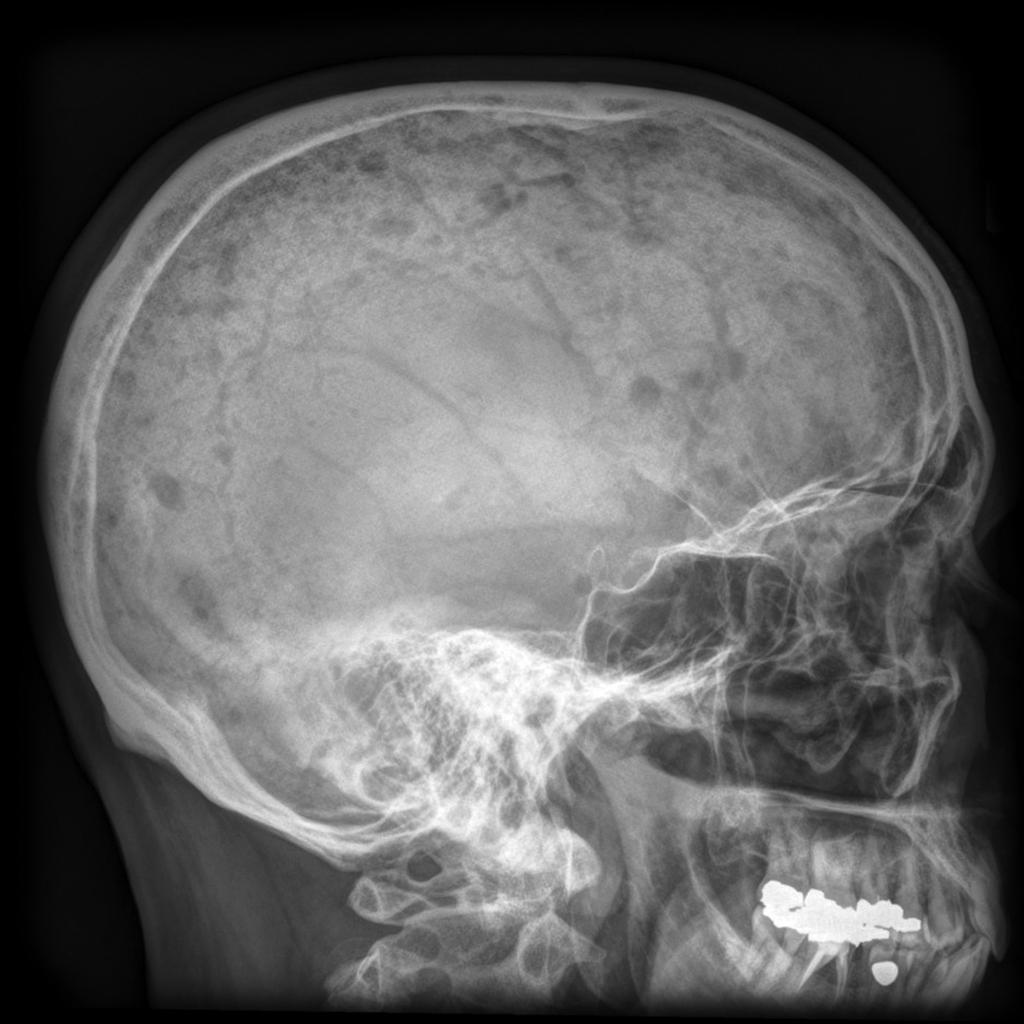
Myeloma causes bone destruction (osteolytic lesions, painful ‘holes’ in the bone). The growth of myeloma cells hinders the normal function of bone-building cells (osteoblasts). In addition, the activity of cells that normally remove worn bone tissue (osteoclasts) is increased. This imbalance of making new and removing old bone tissue caused by myeloma leads to bone destruction. There may be a single lesion or, more commonly, multiple locations (multiple myeloma). In the maxillofacial region the bone lesions predominantly affect the skull and less often the jaws (see Figure 1).
Lymphomas are malignancies of the lymphocytes, a sub-set of the white blood cells. There are many different types and variations of lymphomas (Hodgkin lymphoma is characterised by the presence of a particular type of cell, non-Hodgkin lymphoma are all others), with widely varied clinical behaviour, most of them manifest in the lymphatic system in the lymph nodes. Some lymphomas follow an orderly pattern of spread, and some lymphomas manifest in other tissues and organs (extranodal) as the malignant lymphocytes can infiltrate other tissues.
Oral manifestations of lymphoma can be difficult to distinguish from other conditions such as periodontal disease, osteomyelitis and other malignancies. Commonly mentioned signs and symptoms of oral manifestations of lymphoma are lumps and swellings (including the neck), pain, ulcerated lesions, disturbed sensation and trismus.
The most common location of lymphomas in the maxillofacial region are the salivary glands, in particular the lymph nodes in the parotid gland. This can be as salivary associated lymphoma or a late complication of Sjögren’s syndrome.
Other common locations of lymphoma infiltration are the tonsils, the nasal cavity, and the cervical (neck) lymph nodes. The most common location of lymphoma in hard tissue in the maxillofacial region is the maxilla (upper jaw). There are differences in locations between Hodgkin and non-Hodgkin lymphoma.
The term leukaemia covers a range of different malignancies of the blood system that affect different strands of white blood cells. These are T and B type lymphocytes (acute lymphoblastic leukaemia (ALL) and chronic lymphocytic leukaemia (CLL)) or some white blood cells originating from the myeolid line (acute myelogenous leukaemia (AML) and chronic myelogenous leukaemia (CML); the terms myeloid and myelogenous have the same meaning and are both in use).
Similar to lymphoma cells, also leukaemic cells can infiltrate different tissues and lead to a variety of soft tissue deposits. Oral manifestations are common, in particular localised skin and mucosa infiltrations, including gingival hyperplasia (swellings of the gums), bleeding (petechiae) and haematoma in the oral cavity, oral ulcers, sometimes necrotic lesions, and inflammation of tonsils and throat. Approximately a quarter of patients with acute leukaemia report oral conditions as the first symptoms and nearly three quarters of leukaemia patients at some stage report oral symptoms.
Oral and maxillofacial conditions arising from the treatment of haematological malignancies
The main treatment modalities for haematological malignancies are chemotherapy and radiotherapy or combinations of both. Both treatment modalities typically have unwanted effects with oral manifestations which may have to be treated during treatment for haematological malignancy. The working principles of both chemotherapy and radiotherapy exploit the differences between rapidly and slowly replicating cell lines and cause significantly more harm to rapidly replicating cell lines (such as malignancies) but also the lining cells of the mouth or throat.
Healthy mucosa is a tissue with a high replication rate and thus is susceptible to the cytotoxic effects of chemo- and radiotherapies. Typically, there will be painful severe inflammation and ulceration (mucositis) of the oral mucosa. The risk of infection of these oral lesions is high, with an added risk of tissue necrosis and an increased risk of developing sepsis. This is highly relevant in the treatment of haematological malignancies as most infections under these circumstances are oral infections. Aggressive treatment strategies (for example, chemotherapy approaches in the treatment of childhood leukaemias) are more likely to lead to serious damage to oral (and other) mucosal tissue which may become severe enough to become treatment-limiting.
In addition, a bone marrow transplant from a genetically non-identical donor (allotransplant) for the treatment of leukaemia carries a risk for a serious complication called graft versus host disease. Essentially, the donated graft rejects the host: the immune cells in the graft recognise the recipient’s body cells as foreign and consequently attack them (this is not the same as the host’s immune system recognising the transplanted graft cells as foreign). The complication can take the form of an acute crisis or a chronic form. Graft versus host disease causes oral ulcers which are at high risk of infection because of immunosuppression; chronic graft versus host disease can cause a particular type of white mucosal patches with an enhanced risk for malignant transformation.