Antiepileptic medications
Anticonvulsants, also known as antiepileptics, are drugs that are commonly used in the treatment of epileptic seizures. They have a second / additional life as medicinal drugs in both the stabilisation of mood and in the treatment of pain. Whilst they are not designed as analgesics (painkillers), they can be effective in the treatment of some forms of chronic pain, in particular the acute pain of trigeminal neuralgia and other facial pain syndromes (including pain caused by herpes) and a range of neuropathies. The effect can differ from person to person, and from condition to condition, sometimes these medications may have no beneficial effect at all – but it is worth to explore as a potential treatment option for some of these difficult-to-treat chronic pain conditions.
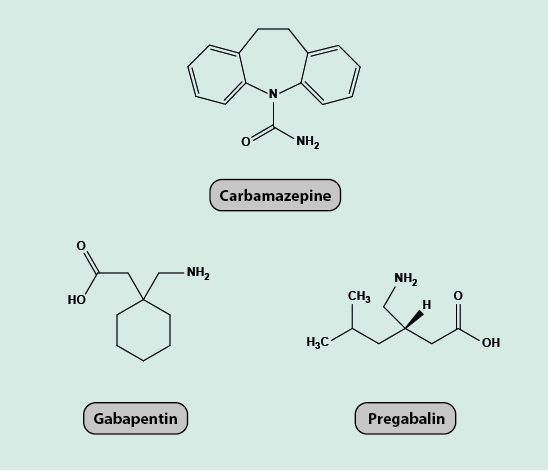
If they are effective, only a low dosage is needed in their role as analgesics for the treatment of neuropathic pain. Drugs that are used for such purposes are carbamazepine, gabapentin and pregabalin (Figure 1).
Carbamazepine was first synthesised in 1953 and was first marketed as a drug to treat trigeminal neuralgia in 1962, including its use as a prophylactic treatment. Carbamazepine is still the drug of choice for treatment of trigeminal neuralgia and can be used in the diagnosis of the condition.
The mechanism of action of carbamazepine is thought to be by blocking voltage-gated sodium channels, binding to inactivated sodium channels and stopping them from becoming active again. This stops the action potential moving along neurons. Carbamazepine also has some action against voltage-gated calcium channels, stopping calcium influx causing the release of neurotransmitters, while also increasing the amount of the inhibitory neurotransmitter GABA (a ubiquitous messenger molecule) and decreasing the amount of the excitatory neurotransmitter glutamate.
Gabapentin is an analogue of GABA. Gabapentin was synthesised in 1977 for the treatment of spasticity and epilepsy. Pregabalin is another analogue of GABA that was developed a decade after gabapentin and has a very similar mechanism of action and effect on the body. Whilst both are GABA analogues, they have no activity against GABA receptors, channels or transporters.
The mechanism of action of gabapentin and pregabalin is not fully understood but the analgesic action is thought to be due to action on voltage-gated calcium channels, stopping release of neurotransmitters.
Pregabalin is six times more potent than gabapentin and has a greater bioavailability , so is more likely than gabapentin to have dose levels that are both effective and tolerable.