Endodontics
There is more than one reason why root canal treatment may become necessary.
The most common reason is due to death of the pulp of the tooth. The pulp runs through the centre of the roots of a tooth, and contains blood vessels, connective tissue and nerves. Once the nerve of the tooth dies, the pulp starts to break down causing products that discolour the tooth. This can explain why some dead teeth are noticeably darker. When the pulp is broken down, bacteria can move in to this space and eventually reach the tip of the tooth (the apex). The bacteria can cause inflammation at the apex, resulting in pain on biting but as the nerve is dead there is no sensitivity to cold or heat. This is known as apical periodontitis. An abscess may form, where the space at the apex becomes filled with pus (bacteria and white bloods cells trying to fight the infection) which can be extremely painful and severely tender to bite on. Once the nerve of the tooth is dead, the treatment options are to remove the dead tissue and replace it with a dental material (root canal treatment) or remove the tooth.
Antibacterial agents are only indicated if the infection causes systemic illness, if the infection is too large to successfully apply anaesthetics (pus is very acidic which can occasionally reduce the effectiveness of local anaesthetics used), or if there is another reason why treatment is not possible at the time (such as severely reduced mouth opening (trismus), or any other medical contraindications to treatment). Antibacterial agents do not treat dental decay and will not prevent the abscess reforming.
Another reason why root canal treatment may become necessary is following trauma. If a tooth has been knocked out, cracked or severely damaged, sometimes a root canal treatment is needed to help prevent future infection and prolong the life of the tooth. In these circumstances an alive tooth may be root treated. Orthodontic treatment can occasionally have an unwanted result of pulp inflammation and death.
If a tooth is very broken down and if somebody is having a denture made, it may be a good idea to keep the root of the tooth to sit underneath this. This may seem odd but it can retain alveolar bone and add some support for the denture (improving retention). This normally involves root canal treatment for the root and a filling material to seal the top of it, a couple of millimeters above the gum level. The denture then covers this up.
Root canal treatments seem to have a bad reputation. This is probably because it is a treatment option for a very painful, infected tooth. Most patients tolerate root canal treatment very well with no pain at all, once appropriate local anaesthetics are in place. Root canal treatments can require multiple appointments, especially in severe infections.
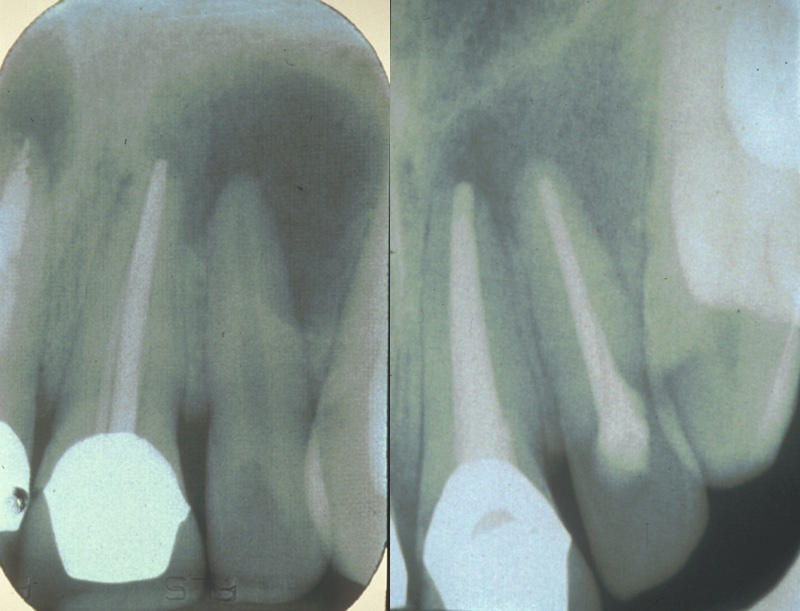
Once the tooth is prepared, a small hole is cut in the top or back of the tooth (unless access can be gained through a cavity once all of the decay is cleared), and the pulp of the tooth is found. A drill is used to do this, in the same way as preparing the tooth for filling material. The pulp is then removed with very thin files (either twisted round by hand or by a rotary machine). Lots of chemicals are used to wash out the inside of the tooth and clean out any bacteria present. X-ray radiographs are needed at several stages throughout root canal treatment to ensure the files and materials are in the correct place.
Once the pulp is removed, the empty space is shaped to make it ideal for filling with whichever material the dentist or endodontist is going to use. Files are used for this as well and sometimes a small electronic device known as an apex locator is used to help the clinician locate the tip of the tooth (as this cannot be seen by looking at the tooth from the outside). Once shaped, the empty and clean canal space can be filled with one of several available materials. An example of this is gutta percha, which is a tough plastic substance from the latex of a specific tree. This can be inserted as small sticks of material or injected inside the tooth in a runny form. The aim is to seal the whole pulp chamber and prevent further bacteria getting inside.
After a root canal treatment, it is essential that the tooth is appropriately restored. Usually, a dental crown is necessary to strengthen the tooth and occasionally filling material is enough to restore the tooth. Root canal treatments are successful in many cases and sometimes re-treatment is possible if a root-treated tooth gets infected. Some dentists do root canal treatments using a microscope to allow them better visualization of the inside of the tooth and there are advanced ways to image the tooth (such as a cone beam CT scan) which are useful in some cases.
Key risks of this treatment are instruments fracturing inside the tooth, re-infection, failure of treatment, multiple appointments are common and there may be obstructions inside the pulp canal which means the filling material cannot be optimally inserted into the space, reducing the chance of success of the treatment.