Thyroid hormones
The thyroid gland secretes a number of hormones that all play central roles in the regulation of the body’s general metabolism. One hormone synthesised in, and released from the thyroid gland when Ca2+ ion concentration levels in the plasma are high, is calcitonin. The role of calcitonin is to slow bone resorption in the normal bone remodelling process. The counterplayer to calcitonin is parathyroid hormone, PTH which upregulates bone resorption and the bone remodelling process. Between these two hormones and their actions, a bone remodelling balance is achieved if both hormones are secreted as they should be and if all feedback loops are working well in this regulated system.
Another highly complicated, regulated system is the chain of events that leads to the release of the two thyroid hormones tetraiodothyronine (thyroxine), T4 and triiodothyronine, T3 (Figure 1). These two hormones are at the centre of regulating the general metabolic rates of many body functions, including breathing and heart rates, digestive functions, body temperature, muscle strength and nervous system functions.
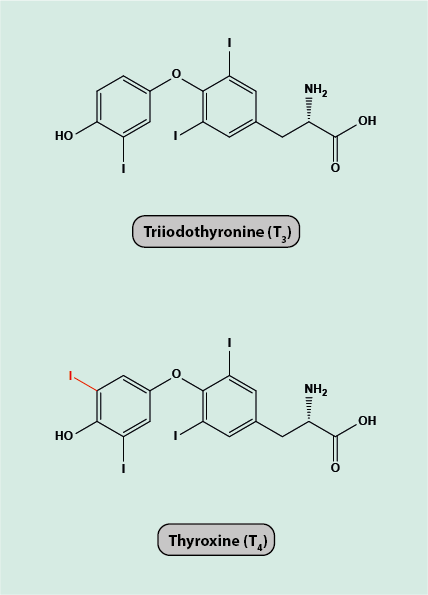
The command centre for the release of thyroid hormone is a small but vitally important region at the base of the brain, the hypothalamus. The hypothalamus releases thyrotropin-releasing hormone, TRH which in turn stimulates the pituitary gland (situated close to the hypothalamus) to secret thyroid-stimulating hormone, TSH. The levels of TSH regulate the synthesis and release of thyroid hormones in the thyroid gland. The amount of thyroid hormones circulating in the blood determines the level of TSH release such that a tight control and feedback loop is maintained to keep the T3/T4 concentrations in a narrow functional window. T4 is essentially the quick-release, circulating storage version of the active form of the hormone, T3. The conversion from T4 to T3 permits rapid response to the body’s situation-dependant metabolic requirements. The chemistry of T4/T3 is unusual for hormones in that both molecules contain three (T3) or four (T4) iodine atoms. To maintain a healthy supply of iodine to enable the synthesis of T3/T4 in the thyroid gland, a sufficient amount of iodine needs to be supplied by the diet. This could be either from natural sources such as seafish, or from supplementation (or use of iodised salt) where the local / personal diet is short of iodine. A sufficient dietary iodine supply helps to prevent the development of goitre, the swelling of the thyroid gland in response to insufficient dietary iodine intake.
Both overactivity (hyperthyroidism) and underactivity (hypothyroidism) of the thyroid gland (or dysfunction elsewhere in the command chain regulating hormone release from the thyroid gland) lead to sometimes severe clinical signs and symptoms that need to be addressed. In a nutshell, underactivity of the thyroid gland or complete lack of thyroid hormones (for example, after removal of the thyroid gland) needs to be managed by replacing the missing hormone levels. Hyperthyroidism may be managed in different ways by a range of different medications to reduce thyroid gland activity levels (for example by carbimazole, a pro-drug that reduces the amount of T3/T4 produced in the thyroid gland), by a targeted form of radiotherapy with radioactive iodine, 131I (which selectively accumulates in the thyroid gland and destroys it), or by surgical removal of some or all of the thyroid gland. Some maxillofacial surgeons carry out tumour-related thyroid (and parathyroid) surgery but always in conjunction with medical endocrinologists.
Diagnostics (mainly clinical examination and a number of specific blood tests) and management of thyroid disorders generally fall into the remit of ear, nose and throat as well as endocrinology specialties rather than maxillofacial surgery. There is, however, one notable exception where maxillofacial surgery in collaboration with ophthalmology is involved in the management of the most common cause for exophthalmus (bulging eyes).
Grave’s disease (also known as Basedow’s disease in Europe) is an autoimmune condition that affects the thyroid gland and leads to overactivity of the gland. One of the signs of the condition is Grave’s ophthalmopathy (bulging eyes) which results from inflammation of the tissues surrounding the eyes in the eye socket. If exophthalmus persists long after otherwise satisfactory management of Grave’s disease, or if the eye condition is such that there is a risk for vision loss from compression of the optic nerve, then maxillofacial surgical intervention is required. The main surgical intervention is orbital decompression surgery, where removing some small bone segments from the eye sockets (orbits) provides decompression such that the protruding eye balls can settle back into a normal position and any pressure on the optic nerve can be relieved. There may also be some corrective surgery to improve function and appearance of the eyelid and / or on the muscles responsible for the synchronised movement of both eyes when diplopia (double vision) is a persistent problem. Double vision may develop as a complication of orbital decompression surgery. Maxillofacial surgical interventions are the same when exophthalmus is caused by other underlying conditions than thyroid diseases.