Damage
Contents
This page gives a more detailed description of some of the materials and methods used in the surgical treatment and repair of soft tissue damage.
The basics: asepsis and antisepsis
Let us just get started with the terminology:
Sterilisation – refers to a process which results in the complete absence of microorganisms, including bacteria and bacterial spores, viruses and fungi.
Asepsis – refers to a process which is close to sterile (‘surgical asepsis’) and ‘as good as can be’ in a living organism without causing tissue damage.
Antisepsis – refers to a process which results in the absence of most pathogenic microorganisms. However, some bacteria, viruses and spores may still be present.
Clean – refers to a reduction in the total bacterial count.
Sepsis was an almost universal complication of surgery and carried a high mortality until Joseph Lister, in 1867, in Scotland, proposed his ‘germ theory’ and put forward the idea of antisepsis to reduce infections in surgical patients. This was one of the major fundamental advances in surgery. Lister used so called carbolic acid (phenol in modern chemical terms) as an antiseptic for skin before surgery and used carbolic-acid drenched dressings afterwards.
Lister’s contributions to make surgery safer are also a wonderful illustration of early interdisciplinary collaboration and international cooperation (it seems that good things happen when Scottish surgeons and European scientists collaborate…). A few years before Lister’s ‘germ theory’ (and practice), Louis Pasteur as the Dean of Sciences at the University of Lille discovered the causative relationship between the presence of bacteria and infection in 1857 to 1863 from his work on fermentation. Lister scrutinised and advocated Pasteur’s work, while Pasteur publicised Lister’s medical applications and his ideas about antiseptic approaches to surgery in France.
The 19th century was an exceptional period in the history of surgery, a century full of improvements and discoveries, many with repercussions today. Amongst the numerous contributors to these innovative approaches was another Scottish surgeon, Lawson Tait. A little later in the 19th century than Lister, he also strongly advocated what he called ‘asepsis’ in surgery, avoiding Lister’s carbolic acid, with similarly improved results over traditional approaches. Ignaz Semmelweiss in Vienna in the early 19th century had demonstrated impressively the beneficial effects of washing hands with antiseptics before treating patients (in particular saving countless lives of women in childbirth). Ernst von Bergmann, a German surgeon in Würzburg and Berlin, is another 19th century pioneer and driver of innovation in surgery: he introduced methods to sterilise surgical instruments in an autoclave. Finally, toward the end of the 19th century, the American surgeon William S. Halstead pioneered the use of sterile latex gloves and the then modern approaches to anaesthesia in surgery. Stop for a second and consider; surgery as we know it has only been possible for just over a century.
Materials for wound cleansing
There are a variety of cleansing solutions available, including:
- Normal saline (9 g of NaCl per 1000 ml H2O)
- Chlorhexidine 0.5 % (aqueous)
- Chlorhexidine 0.5 % (alcohol based)
- Iodine (povidone iodine) 1% (aqueous)
- Iodine (povidone iodine) 1% (alcohol based)
Normal saline (sometimes called ‘isotonic saline, because the Na+ ion concentration is similar to that in blood plasma) has little antiseptic effect but is the least irritant to the tissues. It makes an excellent solution for irrigation (‘lavage’) of wounds during exploration and cleansing. Sterile saline solution in abundance is quite adequate (‘the solution to pollution is dilution’).
Iodine is an effective antiseptic and is widely used for skin disinfection in the form of povidone-iodine (a readily water-soluble mixture of a polymer, hydrogen iodide and elemental iodine). Povidone-iodine has been shown to be effective against MRSA and to date no bacterial resistance to it has been reported. It is also effective against other bacteria, spores, viruses and fungi. Because of this, iodine has replaced most topical antibiotics. The main disadvantage is that some people may develop sensitivity to iodine; it should thus be used only in the short term. It should also not be used on large wounds because here significant absorption of iodine may occur, and the iodine is also destructive to human cells (although less than to pathogens). The alcoholic solution is an irritant to wounds and dangerous on the face near the eyes; it is also a fire hazard. Aqueous solutions are the only preparations used for facial wound disinfection.
Chlorhexidine is an effective antiseptic which is less of an irritant to the tissues than iodine. It is an alternative when allergy to iodine is a problem (and is commonly used for ‘scrubbing up’ of the surgeon). Chlorhexidine is unusual in that when it is used in the mouth, it binds to both tooth enamel and epithelial cells and leaches out over time, thus providing a long-acting effect. This may account for the evidence that suggests that chlorhexidine-containing mouthwashes are more effective than others in controlling oral bacterial infections.
Direct irrigation of deep and obviously infected puncture wounds with a 20 % solution of hydrogen peroxide (H2O2 in water) followed by saline irrigation is a useful occasional technique and an effective haemostatic manoeuvre.
Unfortunately, but unsurprisingly, it has been shown that all these antiseptics inhibit fibroblastic activity and therefore interfere with wound healing. Their use in cleaning infected wounds is not essential because the more important factor is the volume of solution used. Sterile saline solution in abundance is quite adequate, although a diluted povidone-iodine solution used both to scrub mechanically and irrigate ‘dirty’ wounds is commonplace.
Hair-covered epidermis may pose a problem when exploring and closing wounds, particularly when a wound is complex. For simpler wounds, provided that that access is good and cleansing and débridement is easily achievable, it may be acceptable to leave hair in cosmetic areas alone or to trim it. However, where the presence of hair is likely to make cleansing, débridement or closure difficult or when hair is likely to become trapped in a wound, the hair around the wound should be shaved prior to cleansing. There is, however, evidence to suggest that wound infection rates increase significantly if the wound area is shaved in elective surgery. A pragmatic compromise is needed here.
Commonly used wound dressings
Traditional (for example, gauze and Gamgee (made from layers of absorbent cotton wool placed between two layers of gauze (after the inventor, surgeon J.S. Gamgee, Birmingham, 1880)) – these are useful as a secondary dressing to help to control exudate.
Low adherent – these are useful on wounds that have a low exudate, in securing skin grafts or on burns or abrasions. Some are silicone polymers which may improve scar quality.
Alginate dressings – these are dry absorbent dressings made from seaweed. The dressing absorbs exudate from the wound and becomes a gel. Alginates are also useful as haemostats. They should not be used on dry wounds.
Charcoal dressings – these contain activated charcoal which is effective in absorbing chemicals released from fungating, smelly and necrotic wounds. Some charcoal dressings also contain silver which helps to reduce bacterial growth.
Foams – these are synthetic dressings made of hydrophilic polyurethane which absorb wound exudate and maintain a moist wound healing environment. Foams can be used on moderate to heavily exudating wounds which are healthy and granulating.
Hydrocolloids – these consist of a hydrocolloid base made from gelatine, cellulose or pectin. They are completely occlusive and provide a moist wound healing environment. Fluid from the wound is absorbed into the dressing and forms a gel. They are useful on necrotic, sloughy and granulating wounds.
Enzyme preparations – these contain two enzymes: streptokinase and streptodornase and are used to débride wounds, especially wounds with a necrotic eschar.
Hydrogels – these dressings are made up of a copolymer starch and have high water content. They can be used to débride necrotic tissue or sloughy, granulating and epithelializing wounds.
Impregnated dressings – some of these are made from woven cotton which is impregnated with paraffin. These are commonly used on minor burns, abrasions, split skin grafts and donor sites. Other impregnated dressings are made of rayon mesh, impregnated with 10 % povidone – iodine solution (see above). The iodine is released directly onto the wound.
Vapour-permeable films – these are semi-permeable, adhesive film dressings which prevent evaporation of water from the wound. They should only be used on superficial low exudate wounds. These dressings can be useful in the prevention of pressure sore formation over bony prominences by reducing friction.
Antibacterial creams – these contain silver sulphadiazine 1 % (a topical broad spectrum antibacterial agent which inhibits the growth of nearly all pathogenic bacteria and fungi in vitro. This is particularly effective against pseudomonas and staphylococcus aureus and is widely used in the treatment of burns.
Haemostatic agents – these are forms of oxidised cellulose that promote clotting, fibrin foams are effective on bleeding bone ends.
Glues – these fibrin-based tissue glues can be used on skin wounds and (as a spray or drops) to stick grafts or flaps to concave wounds.
Vac-pacs – these are basically adherent dressings which allow the generation of a modest vacuum (reduced pressure) within the sealed area. They promote healing to a sometimes remarkable extent.
Materials for wound closure with sutures
Many different sutures are now available and are generally classified as absorbable or non-absorbable.
Absorbable sutures include those made of
- polyglactin 910 (copolymer of a lactic acid diester and glycoside) – braided resorbables which are absorbed by hydrolysis;
- polyglycolic acid
- copolymer of glycolide and epsilon-caprolactone – a monofilament that is less irritant for subcuticular use;
- catgut (from sheep) has been discontinued for clinical use in the UK but is available in the US.
Non-absorbable sutures include those made of
- nylon, polypropylene, polybutester (a benzoic acid derivative)
Nylon has less memory than polypropylene and ‘polybutester’ but is marginally more irritant. These are the usual sutures for closing skin wounds.
- silk – is essentially and temporary suture material nowadays.
Sutures may also be classified according to their structure
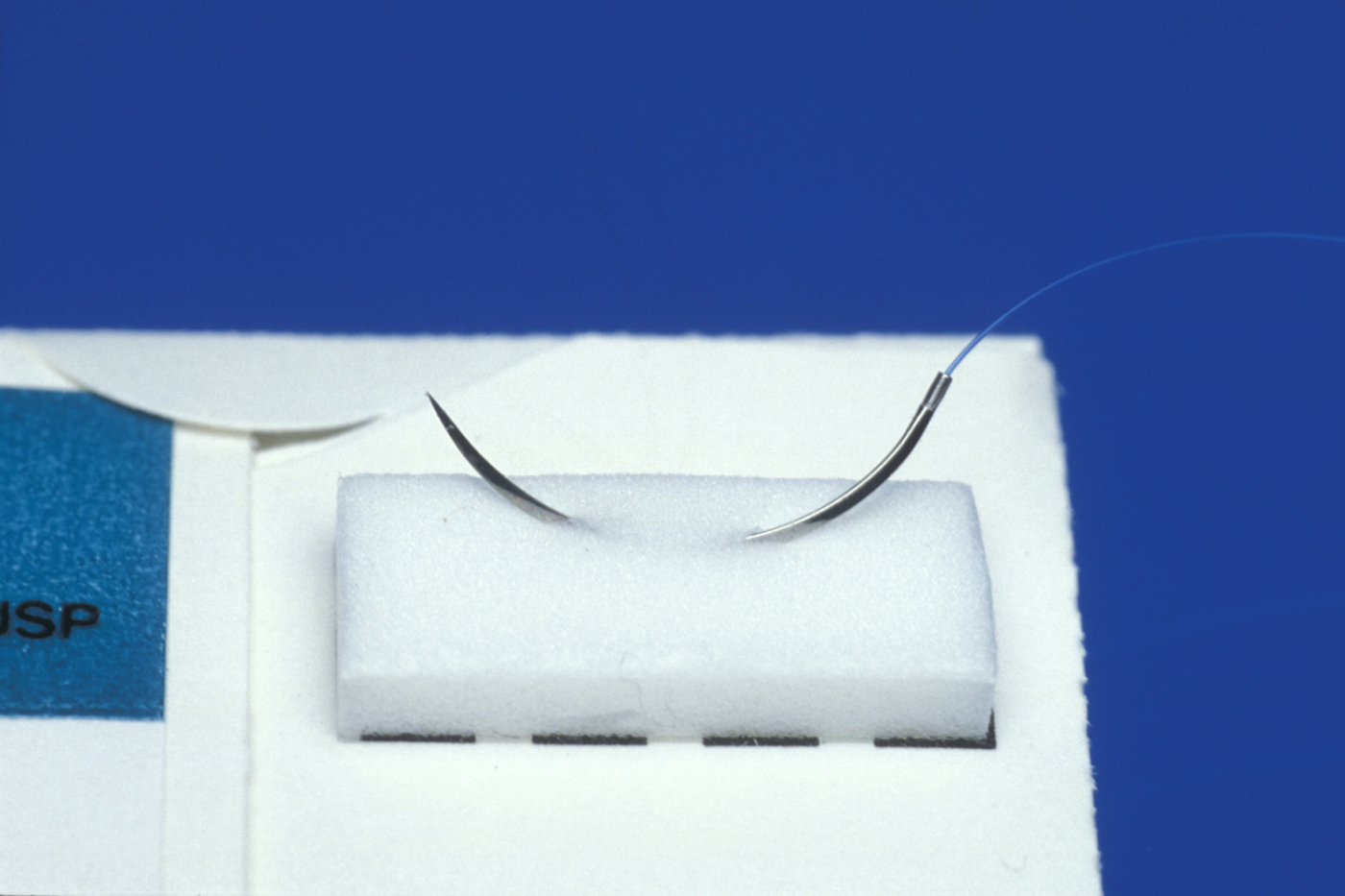
- monofilament (see Figure 1) – these minimise infection, produce less tissue reaction and are the suture of choice for skin;
- twisted or braided - these have plaited strands, which provide secure knots but may act like a wick causing a focus for infection.
Traditionally, silk has been used in the mouth as it is easy to handle, strong, and the ends are comfortable for the patient. Its major disadvantage is that it must be removed. Polyglactin sutures are also popular, since they resorb, and hence do not need to be removed.
Suture techniques
Not only is there a large selection of suture materials, the range of suture techniques is enormous and will accommodate the requirements of a wide range of wounds. These techniques include interrupted and continuous sutures, which may be locking or non-locking and resemble stitching techniques used in embroidery. Methods for layered wound closure, such as vertical and horizontal mattress sutures, confer strength to a wound without suture scars. Subcuticular sutures run in a winding snake like fashion just under the surface of the skin and may be pulled out or left in depending on whether or not the material dissolves. Metal staples of various types are a very rapid method of closing skin which won’t scar if taken out within 10 days. Paper strips can hold the skin surface together if the wound has deep sutures which remove tension. Various tissue glues can be used in a similar fashion.
Interrupted sutures
Interrupted sutures, where individual stitches are not connected, are the most common technique for wound closure.
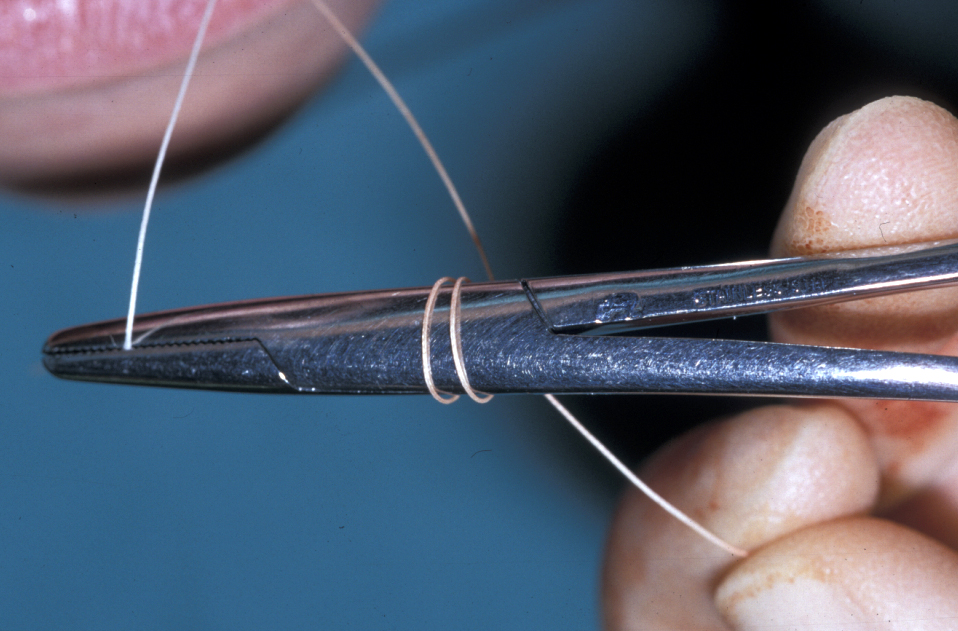
Following cleansing and débridement, the appropriate suture material for the tissue is selected. The wound margins are accurately opposed such that when closed they will align in the correct position. If there are no clues, such as skin creases or angles in the wound, straight wounds may be brought together by means of skin hooks at either end of the wound, creating apposition under gentle tension. The suture needle is held with the needle holder positioned at least one third away from the end of the suture attachment. This reduces the chance of bending or breakage of the needle in the wound. A ‘bite’ of skin is taken at a landmarked site, the size of the bite depending on the depth of the wound (the deeper the wound, the further the bite from the wound edge). The suture needle is advanced to the depth of the wound margin and then out through the wound opening. The needle is next inserted via the depth of the wound and rotated up through the opposite skin margin and the landmarked site for apposition of the wound. The breadth of bite of skin by the suture on either side of the wound should be the same. If the bites are inconsistent, ‘stepping’ of the skin will occur when the suture is knotted, and ultimately scarring.
If the suture is correctly placed and approximates the wound margins accurately, the knot should be tied in the suture (the first knot of the suture is a double-loop which creates a knot with some resistance to loosening; see Figure 2) to bring the margins together, such that the skin edge is slightly everted. Inverted skin margins will heal with a poor aesthetic result. Once the correct suture position is achieved, the suture should be ‘locked’ with a further knot or series of knots.
Aftercare of closed wounds on the face, neck and scalp benefits from application of a thin layer of sterile petroleum jelly (conveniently found in antibiotic (chloramphenicol) eye ointment) which keeps the wound moisturised and clean and minimises crusting, thus making suture removal easier. In wounds under high tension or muscular activity, intramuscular botulinum-alpha toxin injected on either side of the wound can be helpful: it temporarily removes activities creating stretching forces on the scar.
Reasons for failure of sutures:
- breakage – the tensile strength of the suture material is too low or the suture is too small;
- cutting out – too fine a suture material is used or the suture is placed in friable tissue;
- knot slippage – inadequate tying (Every material other than silk benefits from an extra throw on the conventional surgeons knot);
- extruded suture – occurs in combination with infection;
- resorption is too rapidly – nonabsorbable or more slowly absorbable suture material should have been used;
- removal too early – suture is removed before sufficient healing.
Wound healing
Following tissue trauma, there is an initial acute inflammatory response. Protein-rich exudate is released into the wound. Coagulation of blood occurs as fibrinogen is converted to fibrin. White blood cells, lymphocytes and phagocytes, migrate to the wound. Capillaries and lymphatic vessels infiltrate the wound to form granulation tissue, epithelial cells multiply from the margins of intact skin and begin to grow across the surface of the wound. Fibroblasts and collagen fibres begin to appear within the wound as the tissue becomes organised. Contracture of the wound occurs as healing continues and the blood vessels become less obvious. The fibrous tissue in the wound eventually matures to form a ‘scar’.
Wound infections
Wounds may become infected at any stage
Wounds which are frankly infected pre-operatively or have failed to heal with post-operative infection should not normally be closed until the infection has been eradicated. Once the infection has been treated and resolved, it may be appropriate to debride and close it or to allow the wound to heal by granulation. Primary closure is usually delayed in contaminated wounds where there has been a delay in treatment. The wound is usually dressed and remains open for up to five days to ensure infection has not taken hold before further debridement and closure.
The infecting organisms may come from a variety of sources – either endogenous or exogenous. Most wounds encountered, other than clean surgical wounds, must be considered contaminated and therefore require antibiotic treatment. Whilst an ‘informed guess’ may often be made as to the most likely causative organism and antimicrobial therapy commenced on that basis, it is important to take swabs of the wound and send them for culture and sensitivity analysis to ensure the appropriate drug regimen is in place.
Common wound infecting organisms
Staphylococcus aureus is the most frequent cause of wound infection. It is commonly found in the commensal skin flora of around 30 % of the population. There are a variety of strains of s. aureus, which vary in their virulence, whilst multiple antibiotic resistance is on the increase (MRSA, see below); the more common strains of s. aureus still tend to be sensitive to flucloxacillin and similar antibiotics from the penicillin class.
Streptococcus pyogenes, whilst far less common than s. aureus is still found in many wound infections. It is usually sensitive to penicillin.
The above organisms will be the most likely cause of infection in most facial wounds where other sources of contamination have been ruled out. Therefore, initial treatment of such wound infections with flucloxacillin, co-fluampicil (mixture of flucloxacillin and ampicillin) or co-amoxyclav (mixture of ampicillin and clavulanic acid) is effective in most cases. Clarithromycin (a macrolide antibiotic), clindamycin (similar to macrolide antibiotics) or doxycycline (a tetracycline derivative) are the alternatives of choice in such infections when somebody is allergic to the penicillin. The cross reactivity between penicillins and cephalosporins (a beta-lactam derivative) has probably been overstated in the past.
Other organisms
Depending on the source of contamination, wounds may be infected with enterococci, other streptococci or staphylococci, clostridium species or there may be mixed infections.
Most aerobes will be sensitive to penicillin, flucloxacillin, a cephalosporin, or erythromycin and for anaerobes, metronidazole is the drug of choice.
MRSA is a methicillin (multiply) resistant strain of staphylococcus aureus. MRSA is difficult to treat as it is resistant to most antibiotics, intravenous vancomycin being one of the few treatments to be effective in most cases. In a hospital setting, cross-infection control must be put in place to prevent this organism from being spread between patients.
Clostridium species include clostridium tetani. The importance of checking the tetanus immunisation status cannot be over-emphasised. Clostridium species are also responsible for ‘gas gangrene’ whereby the infection causes rapid tissue necrosis via bacterial toxins, and gases are produced. ‘Synergistic gangrene’ may be caused by a mixed infection of aerobes and anaerobes and also results in tissue necrosis. Both forms of gangrene can be rapidly fatal and require urgent treatment with broad-spectrum antibiotics, wide margin excision of the wound, and lavage with hydrogen peroxide (see above).
Streptococcus milleri is the organism most frequently found in serious necrosis-producing head and neck infections. Radical débridement with the appropriate antibiotics as early as possible is the appropriate tactic.