Neuropathies
Nerve damage
Surgical intervention for nerve damage is essentially to release compressing or constricting pressure.
This can be by removing bone compressing a swollen nerve (this is often better achieved medically by short term steroids or a steroid injection) or by removing expanded bone such as in fibrous dysplasia or Paget’s disease.
Perhaps more often it is by removing scar tissue around a nerve that has been caught up in fibrous tissue during healing after trauma or surgery. This is known as neurolysis and is essentially the removal of dense scar tissue while keeping the residual nerve intact and by making incisions along the direction of the nerve in any scar tissue which can not be safely removed from around the nerve.
The key to understanding what can be achieved in terms of nerve damage beyond compression lies in what has gone wrong and what it is surgically feasible to correct or improve. Figure 1 gives a schematic overview of the classification of nerve damage and the corresponding anatomical pathophysiology.
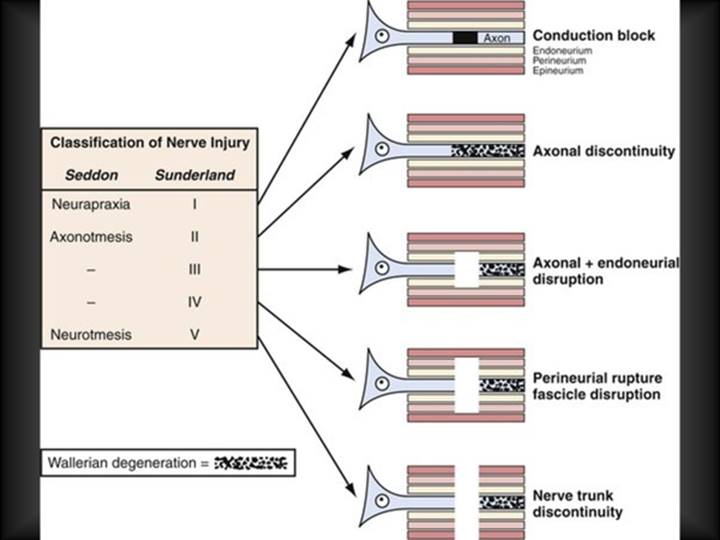
The overview in Figure 1 highlights simultaneously the sheet / layer structure of nerves (endoneurium, perineurium, epineurium) as the basis of classification of damage as well as the resulting functional disruption to nerve conduction capacity as a function of damage to these structures. This is in addition to the physiological response and degenerative process (Wallerian degeneration) that follows damage to peripheral nerves and further hinders nerve conduction outward from the injury), similar to some of the effects occurring in some neurodegenerative diseases.
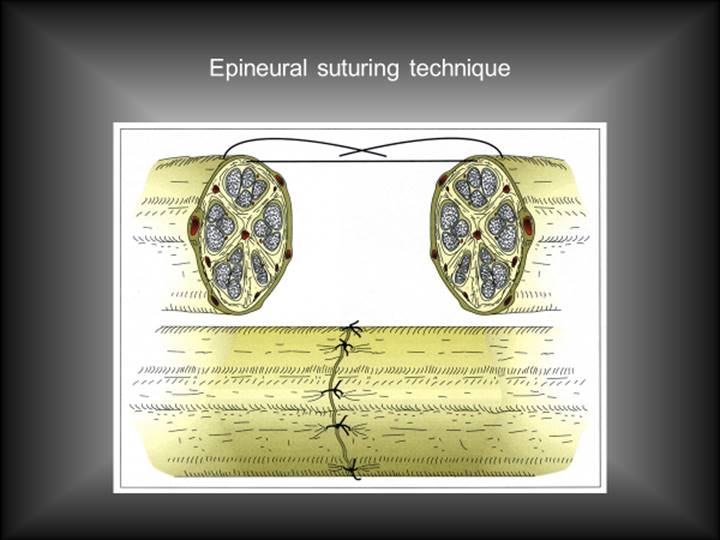
For the most part all that can be realistically achieved under a microscope is to align without tension the macroscopic nerve by suturing the surrounding soft tissue, the epineurium (Figure 2).
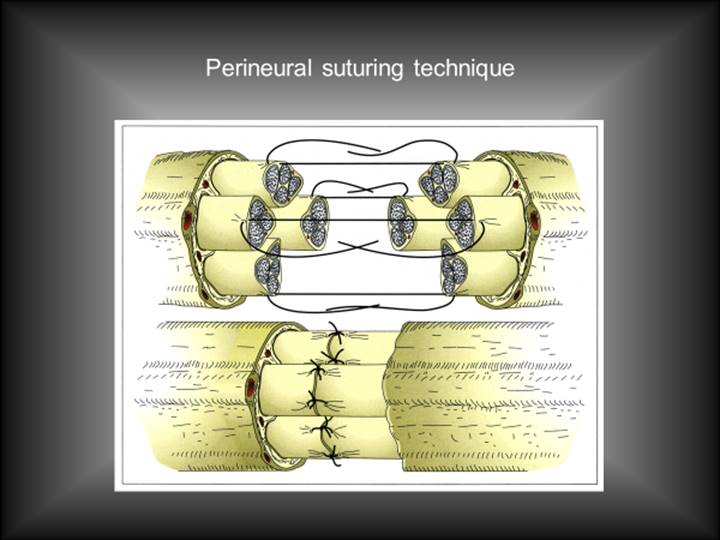
In very large nerves it may be possible to align the nerve fascicles to such an extent that perineurium suturing is possible (Figure 3).
If it is not possible to reconnect severed nerve endings without tension, it may be necessary to bridge a gap by using a nerve graft. An example is shown in Figure 4 where surgical damage to the facial nerve from removal of a schwannoma is repaired by a nerve graft, in this case from the nearby greater auricular nerve. This trades a permanently numb earlobe and side of neck for a possibility (perhaps a 30 % chance) of some recovery of useful function in the branches of the facial nerve.
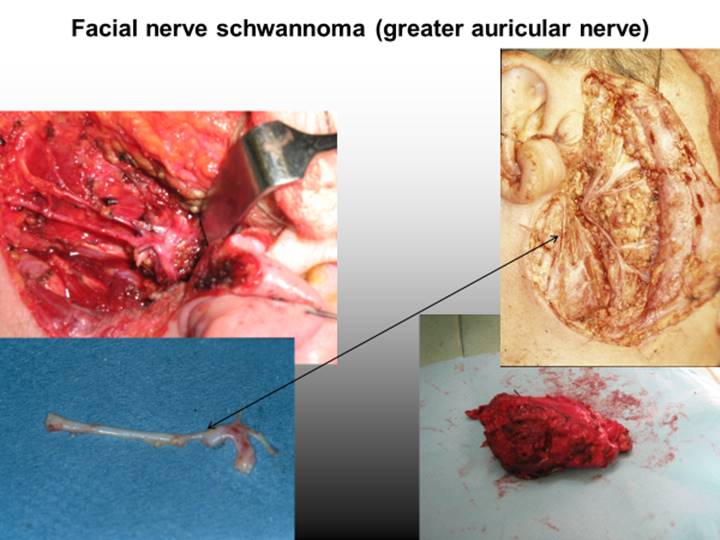
Nerve grafting is typically a choice of the lesser evil as it creates a donor-site defect for sometimes not so great benefit, but on the other hand sometimes there is huge benefit. Typical donor sites for nerve grafts in maxillofacial surgery are the greater auricular nerve and the sural nerve (in the lower leg). As with many aspects of highly specialised surgery there are centres which gain a large volume of experience, create specialist teams with rare resource and by virtue of that, maximise experience. These centres have published results which are substantially better than the experience of surgeons who do not routinely perform nerve grafting.
In all cases beyond simple neuropraxia (temporary loss of nerve conduction, Sunderland Class 1; see Figure 1) where the axon is intact but ‘stunned’ there is axonal degeneration (Wallerian degeneration) back to its origin in the brain or spinal cord. It then has to grow back out to the most distant site it previously reached for sensation or motor activity to return to the pre-injured state. The greater the damage to the ‘tunnel’ it has to grow along, the less likely that process will be fully and easily accomplished.
One way of looking at this is the axon as a rail track and the remaining nerve structures (myelin and myelin secreting cells, connective tissue, endoneurium) as a tunnel. A main nerve is a group of tunnels stuck together by perineurium and a major nerve consists of several groups of tunnels wrapped in epineurium. The best microsurgery may align at a perineural level, so the chances of some of the train tracks (the axons) ending up in a different place from before is quite high.
Microneurosurgical anastomosis of even quite large peripheral nerves appears technically easier than microvascular surgical anastomosis but the functional results are rarely as good.