Non-oral food intake
Having to temporarily, short- or medium term, rely on bypassing the oral cavity and/or throat for feeding (enteral tube feeding) is a fairly common circumstance in major maxillofacial surgery. For example, approximately 70 % of people treated for head & neck malignancies at some stage will need some tube-feeding support. For the majority of people this is a temporary, often short-term condition.
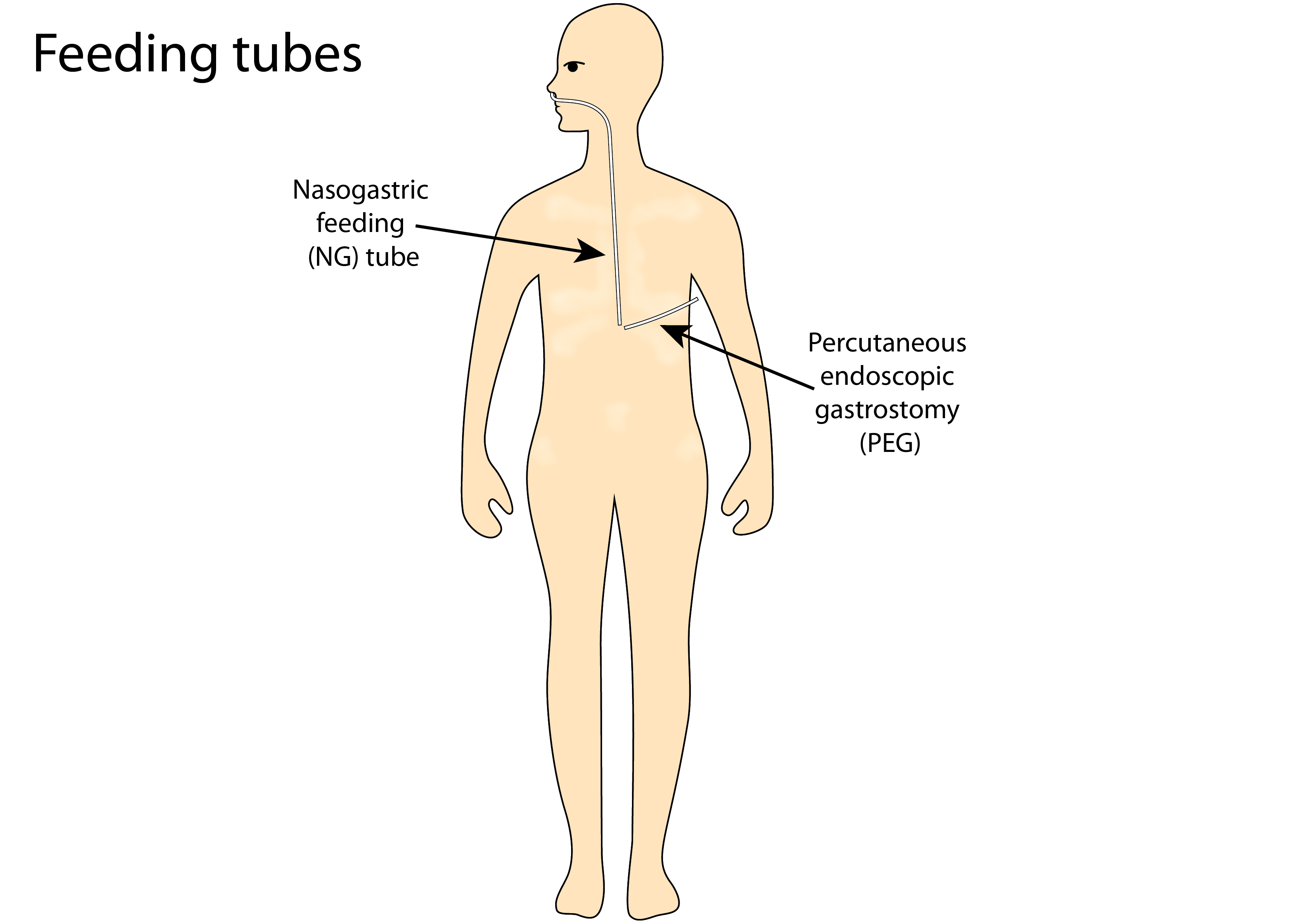
In maxillofacial surgery the need usually is just to bypass the oral cavity and/or throat, and digestion in the stomach and beyond is not impaired. This is the background for the two most common forms of tube feeding in these circumstances: a nasogastric (NG) tube placed through the nose and inserted down the oesophagus into the stomach, or a gastrostomy; either percutaneous endoscopic gastrostomy (PEG) where the tube is inserted directly into the stomach through the wall of the abdomen, radiologically inserted gastrostomy (RIG) or very rarely open gastrostomy. Broadly speaking, NG tubes are mostly used for short- or medium-term needs, usually for periods shorter than three months. A gastrostomy is typically considered for medium- to long-term needs (Figure 1). Long-term needs may be a complete reliance on a gastrostomy for all food and drink, or to use a gastrostomy as a means to supplement oral food intake.
There are numerous aspects to consider, apart from the obvious purpose of tube feeding – providing nutrition when oral food intake is difficult or impossible. It is fair to say that opinions are split for almost all these aspects, and for some of these debates there is not much of a robust body of evidence / information to firmly support one or the other approach. The general consensus probably does not reach much further than the broad agreement that excessive weight loss and malnutrition should be prevented in the first place, but certainly warrant counteracting once developing or established. The literature repeatedly reports a strong correlation between malnutrition and poor outcomes. There also seems to be general acknowledgment of a strong correlation between malnutrition / eating difficulties and depression. Below we sketch a summary of various questions, considerations and arguments related to tube feeding.
When should a (short-term support) NG tube be placed? There are undoubtedly circumstances after major oral and maxillofacial surgery where a NG feeding tube is necessary to protect a surgical wound, to maintain nutrition and/or sometimes to prevent oral infections. Similarly, there are postoperative circumstances where there is really no need to place a temporary NG. To a large extent all situations between these two extremes are a matter of opinion and often follow local/regional established pathways and procedures rather than robust evidence. For example, the short-term postoperative use of NG tubes after relatively minor surgical interventions is far more common in Germany than in the UK. The argument for generous use of postoperative NG tubes in Germany often is the prevention of oral infections. However, the oral cavity is never a sterile or even ‘clean’ environment and one can argue that meticulous oral hygiene and guidance & support postoperatively goes a long way in preventing infections and the need for NG tubes. In fact, meticulous oral hygiene is even more important when using a NG tube – in preventing infections!
There is a longstanding debate about the prophylactic placement of a NG tube (or PEG/RIG; see below) at the beginning of radiotherapy treatment to the maxillofacial region. Opinions diverge here strongly. Some argue that the adverse effects of radiotherapy (painful mucositis in particular) are so common that the majority of people undergoing high-energy irradiation regimens will eventually need support by a feeding tube anyway, so why not place a tube ready to be used at the beginning of the radiotherapy scheme. Others argue that feeding tubes should only be considered when there is really no alternative, that clever management of difficulties, attention to detail, appropriate support and suitable forms of oral food may help many more people through such periods without having to rely on tube feeding. The argument about maintaining some swallowing as much as possible at all times weighs even more heavily where it comes to dealing with the management of the adverse effects of radiotherapy. There are pronounced and lasting effects of radiotherapy on the soft (and hard) tissues of the head and neck region. Supporting some swallowing activity, even under temporarily difficult circumstances, may be considered as some special form of physiotherapy exercise, aiming at maximally preserving and restoring swallowing functionality. There does not seem to be any conclusive evidence as to the short- and long-term benefits (or lack thereof) of prophylactic placement of feeding tubes at the beginning of head & neck radiotherapy treatment as opposed to placing a feeding tube only when definitely needed. There is, however, consensus that return to near pre-treatment swallowing is quicker when tube feeding is not used. This seems to be due to a combination of psychological and physiological reasons. The difference is even more marked between nasogastric feeding and gastrostomy feeding. The main difference in opinion amongst professionals seems to be the threshold for when enteral feeding cannot be avoided.
When should a (short-term support) NG tube be removed? The answer to this question is simple: as soon as is safe/ reasonable / possible. A return to some degree of oral food intake, be it texture-modified or otherwise adapted foods (temporarily or permanently) or a ‘normal’ diet, is a major contributing factor to recovery and wellbeing. The removal of a NG tube after a probably difficult and unpleasant period is a real milestone for most people. Apart from these holistic considerations, one can also make more technical arguments to support an approach aiming for the shortest possible duration of NG tube feeding. It has been shown that for some people over time some form of tube dependency can develop along some fear of returning to oral food (with mostly children and elderly people affected). This effect can be reduced by keeping the NG tube feeding episode as short as possible. Another argument that has been made repeatedly is the lack of training effect on the muscles that support the swallowing act if tube feeding is used for longer periods, following the general idea of ‘use it or loose it’. If more swallowing competence and ability is lost over extended periods of tube feeding, it only makes the return to oral food harder and more ‘relearning’ is needed. Finally, in principle a healthy and balanced diet is easier to provide with oral food intake, even when having to rely on texture-modified food, than when relying on feeding-tube formula (see below).
Which type of feeding tube, NG, PEG or RIG, should be chosen? Generally speaking, NG tubes cater for short-term needs, gastrostomy is more suitable for longer-term needs. The advantage of a NG tube is that its placement is a less invasive intervention than the placement of a PEG or RIG. Both types of tubes are similarly quick and easy to remove – they just need to be pulled. The insertion of a PEG is usually a minimally invasive, endoscopically guided procedure, a RIG is done with an NG tube in place under ultrasound guidance; an open surgical approach is rarely used. Different feeding strategies, either mimicking several meals per day or some more continual, slow drip-feed approach, are possible with both types of tubes. A gastrostomy is a more lasting ‘installation’ but needs regular replacement. With a view to long-term feeding needs, a gastrostomy is more stable, allowing for more flexibility and mobility, and is more discrete as it is not visible under normal clothes. A gastrostomy tube typically lasts for half a year before it needs replacing with a new tube.
There is a consensus on NG tubes being disliked intensely whereas gastrostomy, once in place, seems to be better tolerated. Certainly from the maxillofacial surgery perspective, once people have got used to a gastrostomy it is difficult to wean them off it, whereas people can’t wait to get rid of NG tubes.
What are commercial feeding formulae made of? There are numerous different brands and liquid preparations for tube feeding. These formulae follow general composition guidelines according to normal requirements of macro- and micronutrients, carbohydrates, proteins, fat and fibres, plus trace elements and vitamins, respectively.
These formulae satisfy recommendations as to the amounts of calories and composition. Unfortunately, they do so by mixing ingredients that nobody would normally consider as components of a healthy diet. Much of the calories is made up by sugar (corn syrup a common component, glucose and fructose), protein is usually provided by soy bean products or milk proteins of all kinds, many use fats derived from palm oil, mostly triglycerides and fibre components vary widely with some preparations short on fibres. Micronutrients are added to the preparations to cover trace element and vitamin supplies.
It is evident that these preparations are not the equivalent of a healthy balanced diet. These formulae provide the basic needs in terms of quantities but one may be tempted to view them as a diet consisting of liquefied doughnuts enhanced by vitamin tablets. Many people relying on these formulae have problems with indigestion, constipation, vomiting, diarrhoea, nausea and other forms of food intolerance. This is a serious concern especially for long-term feeding. Some of the intolerance problems can be minimised by using different formulae and different feeding regimens (‘long and thin’ as opposed to bolus feeding) but usually intolerance problems cannot be completely resolved in these ways. The high sugar content is less than ideal for all but is highly problematic for anybody suffering from diabetes.
If long-term tube feeding cannot be avoided, it may take some effort to find a workable regimen. An alternative to commercial formulae are blended liquid diets, prepared from ‘normal’ foods at home. Until the introduction of commercial formulae for tube feeding, this used to be the only way to eat with a feeding tube. There are many patient reports that blended liquid diets can work better than commercial formulae. It is a viable and good alternative for some, but may not work for all.
What are the most common difficulties encountered with tube feeding? Feeding tubes as such normally do not cause discomfort. However, there is one very common difficulty with short- and long-term use of tube feeding: intolerance to the various commercial formulae (see above). Feeding tubes have fairly small diameters in order to minimise discomfort (similar to the diameter of a small drinking straw). This explains another common problem, a blockage of the tube. Most commonly, such blockages are caused by medications applied through the tube, or by not sufficiently flushing the tube with water before and after eating. In most blockage cases, a little perseverance, patience and gentle nudging with the help of warm water or a fizzy liquid will resolve the issue.