Craniofacial implants
Prostheses are adapted to craniofacial implants with either magnets or retentive buttons, or in some instances custom fitted bars to provide retention and anchorage points for the ear, eye or nasal prosthesis being used.
Perhaps the easiest way to describe the process of placing craniofacial implants and the more time consuming and complex process of creating the prosthesis is by illustration. Here are some examples. We briefly describe rehabilitation by a prosthetic nose, by a more complicated prosthesis after extensive loss of mixed tissues, by repair of an orbital fracture, and by prosthetic replacement of a large skull bone defect.
A prosthetic nose
If part of the face has to be removed, for example the nose (Figure 1), in treatment with curative intent of skin cancer, such as an extended squamous cell carcinoma of the nose, the first stage, after wound healing, is to make an impression of the part of the body where the resection took place.


Then craniofacial implants (shorter length than dental implants) are inserted in suitable bone matrix (Figure 3).

Next, a specialist maxillofacial technician creates the nose on a plaster model (Figure 4) and finally colours the prosthesis. In this case, magnets are used to retain the new nose to the implants (Figure 5; the magnets used for such purposes are tiny, yet powerful, permanent magnets).


Prosthetic rehabilitation after major maxillary resection
Maxillectomy (removal of parts of the upper jaw) with orbital exenteration (removal of the eye ball and other soft tissues in the eye socket) in tumour surgery can create a complex combination defect which requires a combination of reconstructive flap techniques and rehabilitation with craniofacial implants and prosthesis (Figure 6).

Again, the prosthesis is held by craniofacial implants with magnetic attachments. Depending on the type and size of the defect, finding suitable anchor points for prosthesis can be a challenge. In this case, the upper implants are inserted into the intact supraorbital (upper) ridge and the lower implants are inserted into a microvascular bony flap (Figure 7).

Following the creation of models and fitting and colouring the prosthesis, the final result (Figure 8) has high aesthetic standards because these body replacement parts can be fabricated to extremely high standards in the laboratory.

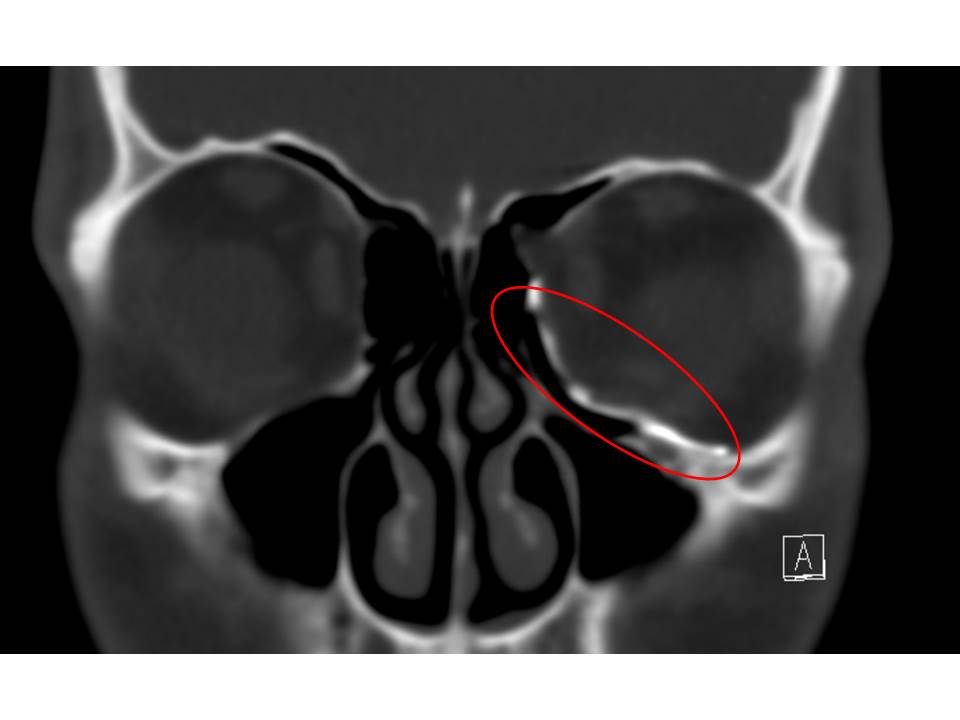
Rehabilitation / repair after orbital (eye socket) fracture
Some consider titanium implants used in the repair of orbital fractures a form of craniofacial implants.
After a CT scan the healthy orbit is mirrored to the fractured one. The mirrored orbital floor is used as guide for a custom made craniofacial implant. The implant is designed on the computer and then 3D printed in titanium. The implant is inserted to the orbital floor and fixed with screws to the lower orbital rim (Figure 9).

The aim is to nearly normalise the orbital volume and remove adhesions to the fracture which can cause double vision by impacting the optic nerve. Clinical evaluation of eye movement and vision is used to assess the outcome and a CT scan is performed to assess the fit of the implant (Figure 10).
Prosthetic rehabilitation of a large skull defect
A further variant of craniofacial implants are implants to reconstruct the skull. Cranioplasty with both acrylic and titanium implants are very common after neurosurgical procedures where the skull has been lost, such as after severe trauma.
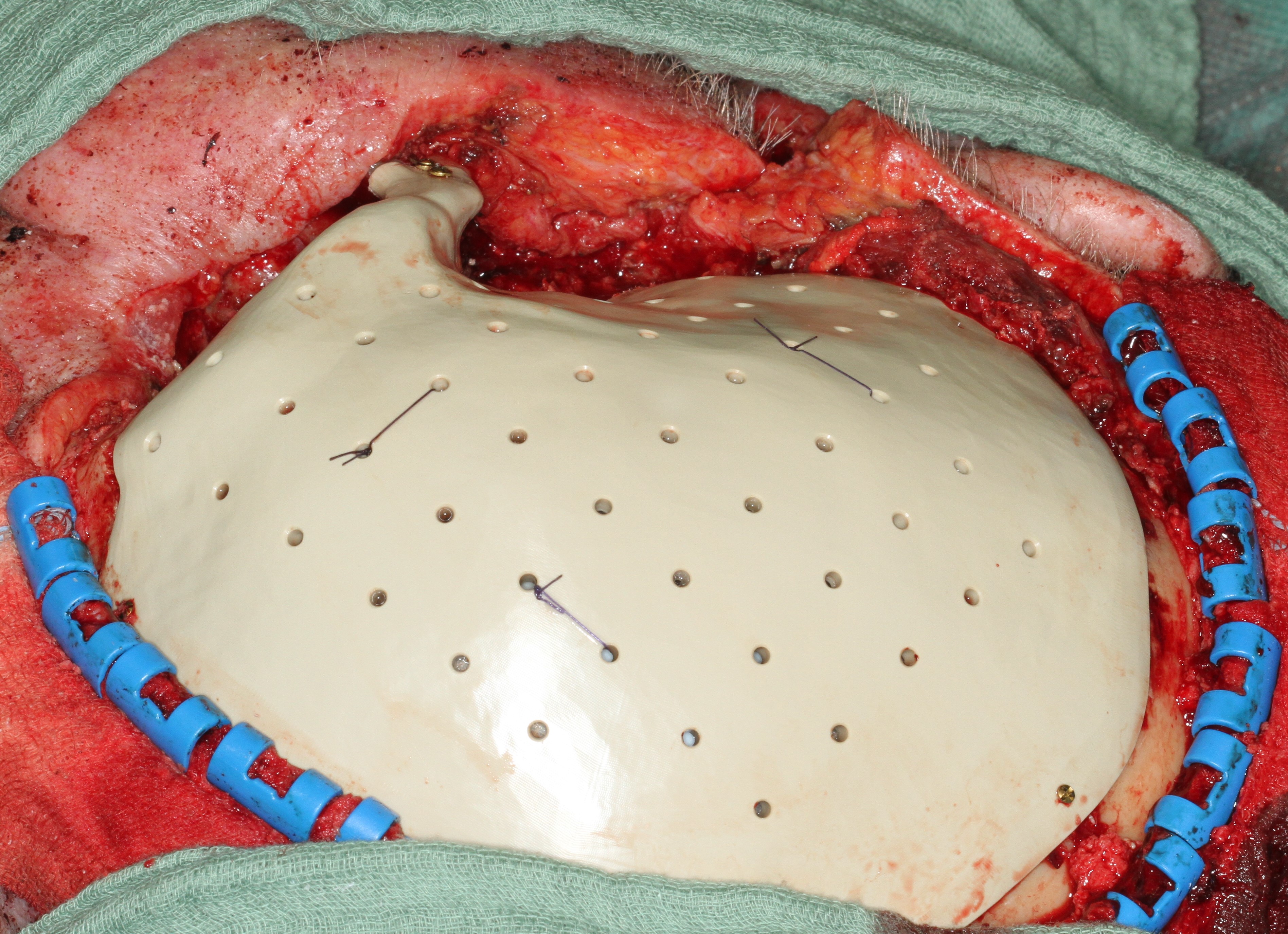
In cases of elective resection of the skull, for example in tumour surgery, a combination of resection guides and customised cranial implants can be helpful (Figure 11).
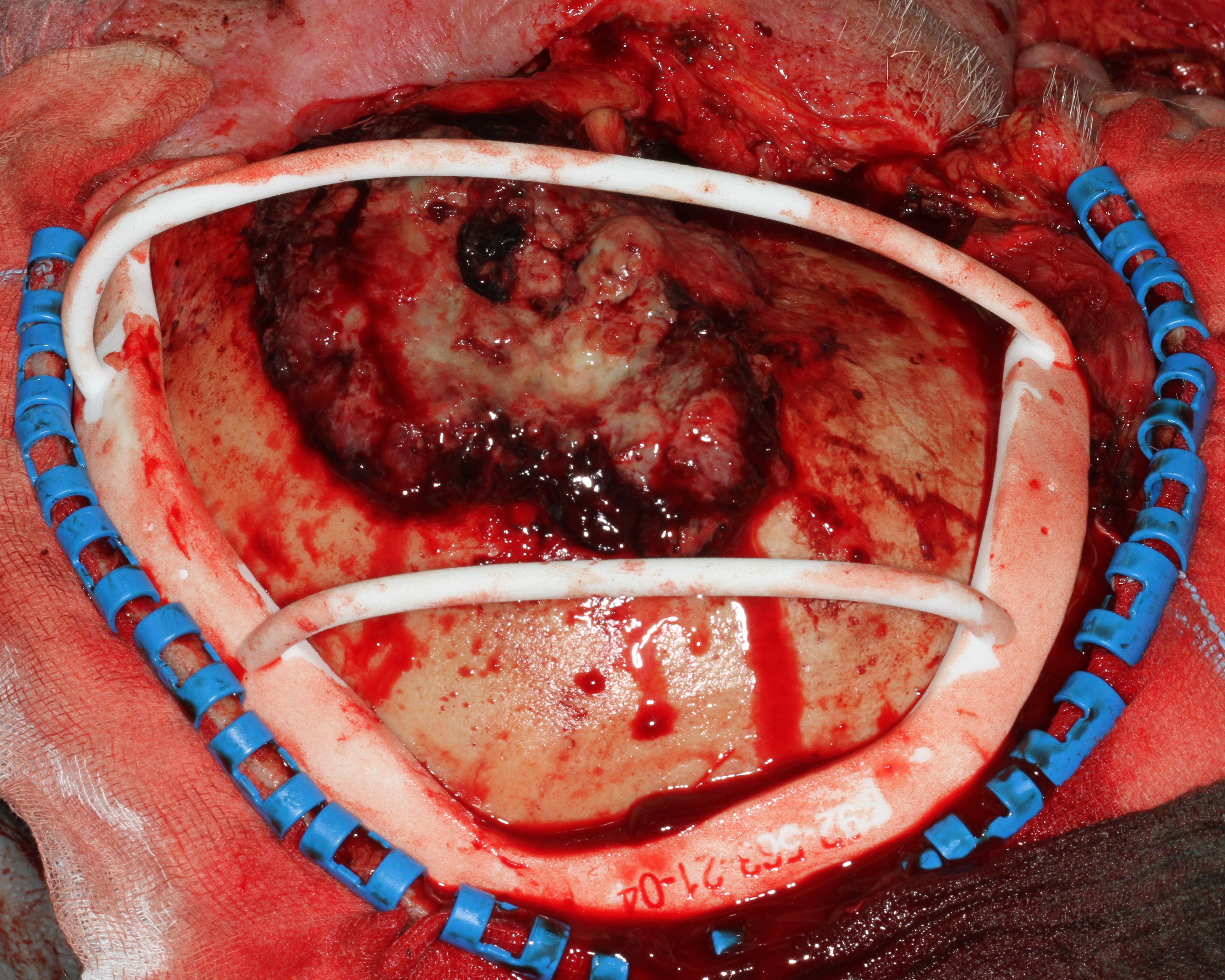
The removal of the affected part of the skull is planned based on a CT scan. To aid precise excision while minimising unnecessary bone loss, a resection guide is 3D printed from the high-resolution CT data. After resection along the resection guide, an implant exactly fitting into the defect is placed to protect the brain (Figure 12).
At the end of surgery, the skull implant has to be covered by a soft tissue flap to protect the implant from infection. Here the soft tissue coverage is provided by an anterolateral thigh free flap (Figure13).
