Speech
Similar to swallowing, speech is a complicated process that requires many different structures to function in a coordinated manner. In the same way as swallowing problems (dysphagia), speech impairments can have many different causes, only some of which are within the remit of oral & maxillofacial surgery.
Speech problems can be classified roughly in three types of impairments:
- articulation problems
- fluency problems
- voice problems.
These categories, in turn roughly correlate with the many different underlying causes of speech impairments. Articulation problems are mainly the consequence of mechanical failures of the oral structures required for speech, mainly the tongue. Fluency problems (such as a stutter, or impaired speech (aphasia) following a stroke) typically have neurological causes, sometimes behavioural / mental health or cognitive origins. Voice disorders (such as polyps of the vocal cords, or poor voice quality (functional dysphonia) without any obvious cause) mainly originate from disorders of the larynx and belong to the domain of ENT (ear, nose, throat) specialists. Our website does not discuss fluency and voice problems, but concentrates on articulation disorders encountered in oral & maxillofacial conditions.
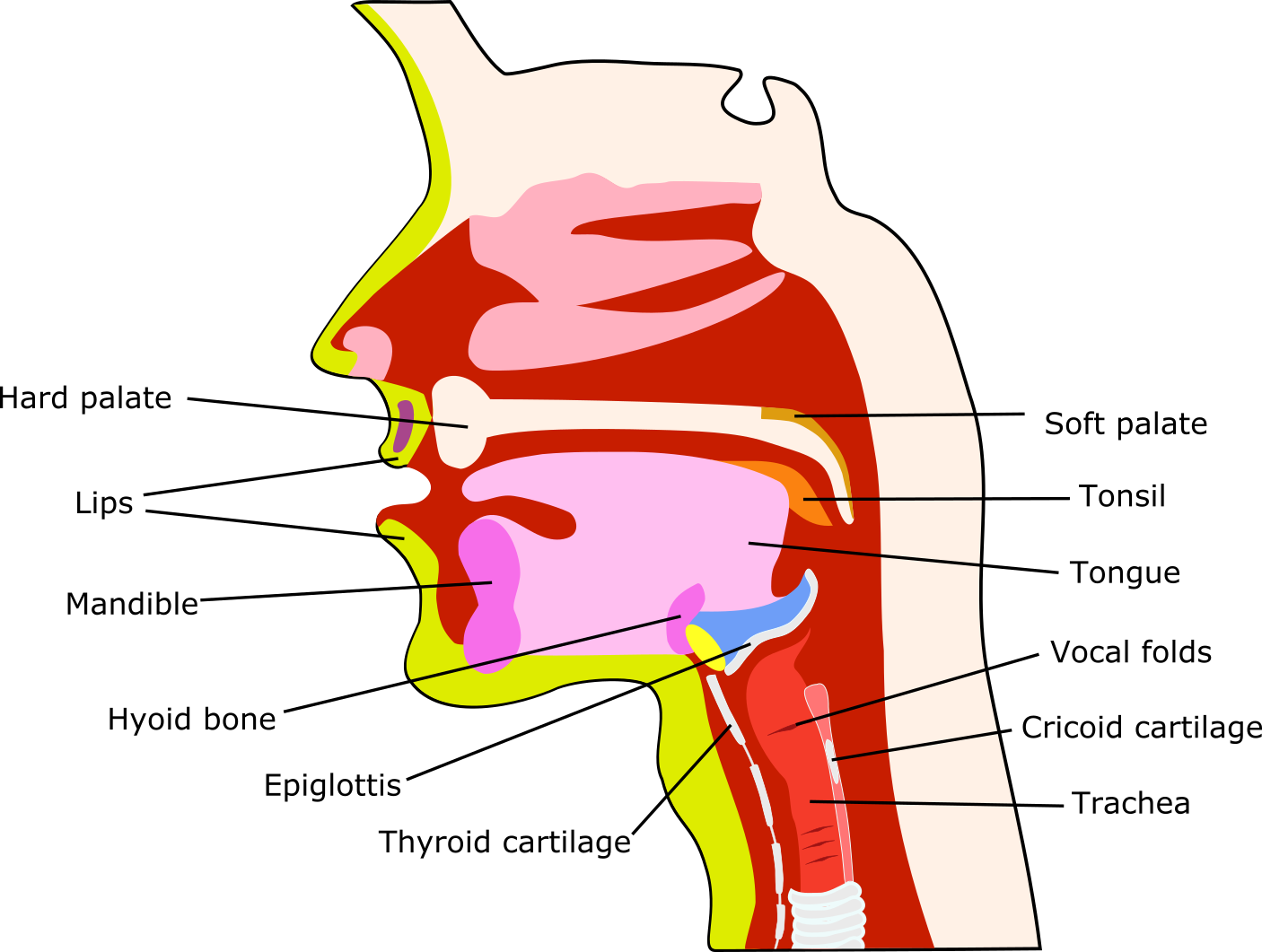
In an oral & maxillofacial surgery context, nearly all speech problems are articulation problems. The short real-time MRI video clip (Figure 2), demonstrating pronunciation of the vowels, together with a schematic overview of the anatomical structures involved (Figure 1) illustrates the many structures involved in articulation.
Speech problems encountered in oral & maxillofacial surgery are a diverse group of symptoms, arising from disease and/or its treatment(s). Speech problems occur across all ages, can be temporary or permanent, and cover the entire range from minor inconvenience without need for interventions, to severe and debilitating, lasting speech dysfunction.
The most common causes of speech impairments related to maxillofacial conditions include
- head & neck malignancies, especially affecting the tongue and/or lips, at all stages of disease and treatment, including reconstructive surgery and long-term effects of radiotherapy applied to the head & neck region;
- major trauma;
- cleft lip and palate and craniofacial syndromes;
- some benign conditions such as torus palatinus, or a tongue tie which limits tongue tip movement, or jaw disproportions such as an open bite;
- xerostomia (dry mouth) or, at the other extreme of salivary conditions, severe sialorrhea (drooling);
- facial palsy from any cause, particularly affecting the branches of the facial nerve which innervates the lips and cheeks;
- minor but troublesome impediments may arise from wearing prosthesis such as false teeth/tooth or removable orthodontic appliances, although these are usually quickly adapted to.
Irrespective of the exact nature of the condition leading to speech impairment, the role of speech and language therapists broadly covers two aspects:
- assessment, and
- training/rehabilitation and coping strategies.
Management of speech problems typically is a long-term collaboration between speech and language therapist and patient, including a major element of self-help and practising. For many speech problems from maxillofacial conditions, restorative dentistry plays an important role. Most management is non-surgical; only rarely will speech impairments benefit from surgical interventions such as lingual fraenotomy or orthognathic surgery. It is common for maxillofacial patients that speech impairments occur alongside swallowing problems.
Assessment of speech disorders typically includes a conversation about, and a record of the subjective perception of the problem(s), type and severity. This narrative should include the consideration of any emotional impact which can be considerable. Objective assessment typically includes the recording of some standardised speech patterns (where the standard phonemes (sound bites) are characteristics of different languages) for a given language (see Figure 3 for illustration), followed by analysis of speech intelligibility by some computer software package.
Advice and training / rehabilitation, as well as the extent to which speech can be restored, strongly depend on the underlying cause(s) of the speech impairment. For example, there will be strategies to prevent a child from developing ‘wrong’ speech habits because of a cleft lip & palate, where pretty much universal standard of care is for early palate closure before serious language learning takes place. This is very different from the most helpful approaches for an adult after major maxillofacial ablative & reconstructive surgery when, for example, the tip of the tongue can no longer support articulation. Resilience and perseverance are important ingredients in any attempts to regain as much intelligible speech as is individually possible in such circumstances.