Preprosthetic surgery
Contents
Below aspects of soft and hard tissue surgery in preparation for prosthesis, including osseointegrated implants, are described.
Soft tissue surgery
Below some common soft tissue procedures include are outlined:
- frenectomy;
- ridge reduction;
- removal of irritation (‘denture’) hyperplasia;
- vestibuloplasty.
Frenectomy
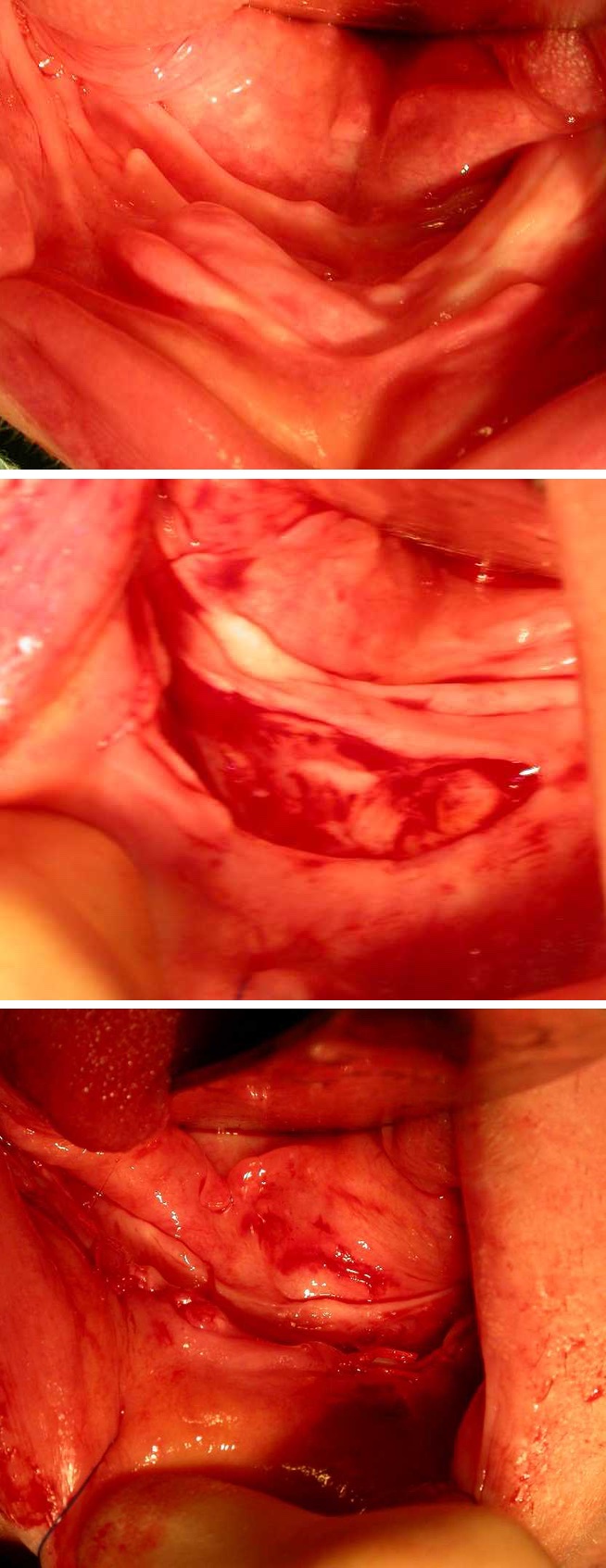
Large frenae (Figure 1) or resorption of the residual ridge can interfere with the peripheral seal of a denture leading to poor retention. The relief for such frenae (that is drilling away some of the acrylic of the denture to accommodate the frenum) may also result in repeat fractures of the prosthesis and discomfort. In these cases, frenectomy is performed either by simple division or by Z-plasty.

‘Flabby’ ridge reduction (‘Schlotterkamm’)
Where tooth loss has been associated with advanced periodontal disease, excess of soft tissue may result in a flabby ridge which in turn causes poor denture stability. This commonly affects the maxillary tuberosity region and labial segments. The localised bone loss can be further accelerated if natural standing teeth oppose a denture. In these cases, soft tissue reduction is carried out by excision of the underlying fibrous tissue whilst preserving, where possible, the attached mucosa. In these cases, it is important to have a replacement baseplate in which a tissue conditioner can be placed to enable close adaptation of the mucosa to the underlying bony ridge.
Irritation (denture) hyperplasia.
Resorption of the residual ridge continues after initial socket healing. The loss of bone height will result in a previously adequately extended denture having a peripheral margin that is overextended, usually into the buccal or labial sulcus. This causes a traumatic ulcer in the sulcus , which, with repeated trauma, produces an overgrowth of fibrous (scar) tissue. Initial management is by the drastic local relief of the flange of the denture and strict instructions to leave the denture out as much as possible (‘social use only’). After a period of a few weeks, inflammation is reduced and the hyperplastic tissue reduces in size. In many cases the reduction in size is such that the hyperplastic tissue will not interfere with new denture construction.
Where the residual hyperplastic tissue will interfere with denture construction, excision is indicated (Figure 2). This may take the form of a simple excision, with elliptical excision of the excess tissue at its base. In large areas of hyperplasia, simple excision may create a shallow V-shaped sulcus. In these cases, a mucosal-preserving approach should be attempted, by dissecting and preserving the buccal / labial mucosa while excising the remainder of the hyperplastic lesion. The preserved mucosa is inlaid as a graft to preserve sulcus depth. In this case, a healing baseplate suitably lined with tissue conditioner is essential to try to maintain sulcus depth.
Vestibuloplasty
In areas where there has been loss of residual ridge height or sulcus depth, commonly due to the loss of attached mucosa, vestibuloplasty may be beneficial. In these cases, a supraperiosteal mucosal flap is reflected and sutured ‘apically’ in the sulcus. Muscle attachments may need to be released in order to achieve the desired increase in sulcus depth. The exposed periosteum may be left to granulate, however this may result in scarring and a narrow V-shaped sulcus, which the prosthetist may have difficulty in utilising. Scar reduction may be achieved by grafting with palatal mucosal free graft or split skin graft. In either case, a healing baseplate lined with gutta percha or a proprietary denture liner should be fixed in place for the initial healing period by means of a heavy non-resorbable suture (or stainless steel wire) passed around the mandible or less often through the maxillary antrum or screws directly into the hard palate.
After initial healing, a temporary denture extended to the full depth of the new sulcus should be provided. Unfortunately, the benefits of vestibuloplasty are lost if subsequent prostheses do not make full use of the new sulcus depth.
Hard tissue surgery
Hard tissue surgery may be required in the form of
- alveoplasty;
- ridge reduction;
- removal of tori and reduction in muscle attachments.
These procedures aim to reduce or remove hard tissue prominences that create excess undercuts, which the prosthetist is unable to use, so creating dead spaces. Complete elimination of undercuts might lead to a worse condition post-operatively with a completely unretentive denture. It is even more important in hard tissue preprosthetic surgery that liaison is maintained between the surgeon and the prosthetist to agree on how much bone should be removed in order to achieve the maximum prosthetic gain.
Where there has been significant bone loss, consideration may be given to
- ridge augmentation (onlay or interpositional grafting);
- distraction osteogenesis.
All of these techniques may be augmented by the use of growth factors derived from platelet-rich plasma.
Alveoplasty
Despite the most careful of extraction techniques circumstances will occur where the residual ridge heals to become irregular or feather edged. Pressure on these bony irregularities under the mucosa by a denture results in pain. Alveoplasty is the smoothing of these bony irregularities. Mucoperiosteal flaps are reflected using a sub-crestal incision to expose the whole of the residual ridge. The irregular areas can be visualised or felt with the gloved finger and smoothed using hand instruments or well-irrigated burrs. Alveolar bone is precious and only the minimum amount of bone should be removed in order to achieve the desired result. In cases where extensive smoothing is required, an intraoperative clear acrylic template may help demonstrate residual areas of irregularity by blanching of the underlying mucosa.
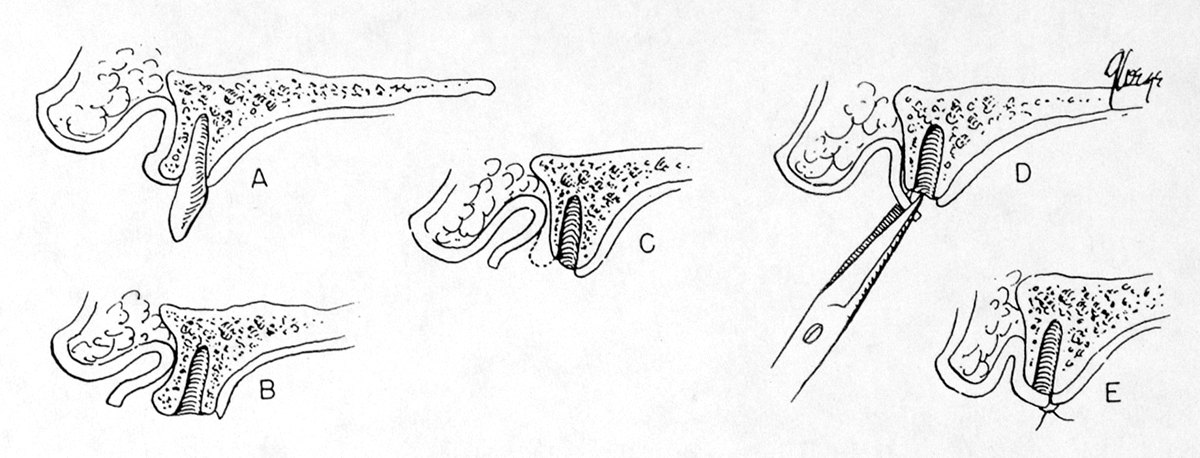
Ridge reduction
Where the residual ridge heals with excessive undercuts, reduction may be of benefit. In consultation with the prosthetist, the undercut is reduced or removed via a mucoperiosteal flap raised from a sub-crestal incision. Pre-surgical planning demonstrating acceptable paths of insertion will dictate how much undercut should be removed to give the maximum denture retention (Figure 3).

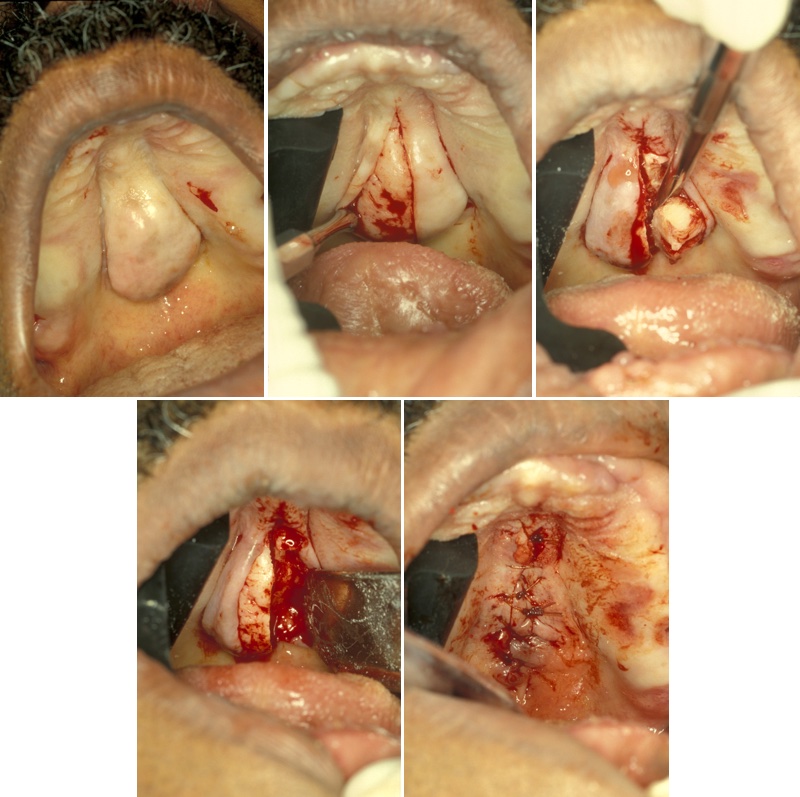
Removal of tori and muscle attachments
Palatal and lingual (mandibular) tori are normal anatomical variants. The lingual tori and prominent genial tubercles are often bony overgrowths at the site of muscle attachments. As the lower full denture is inherently unstable, there may be benefits in retaining the lingual torus unilaterally to facilitate the use of the undercut to improve retention and stability. Prominent genial tubercles commonly occur in the atrophic mandible. They are removed on symptomatic grounds but may result in further loss of stability of the lower prosthesis.
Lingual tori are removed via a lingual mucoperiosteal flap. Care should be taken in reflection of these flaps, as the mucosa is friable. Particular care needs to be taken around the bony prominence due to undercuts. The bony prominence may be removed with burs combined with hand instruments such as an osteotome. A wide flap is raised to protect the lingual nerve adequately because, idiosyncratically, a wide subperiosteal lingual flap is associated with a lower level of lingual nerve neuropraxia than a small flap.
Palatal tori should be removed if they cause denture instability or repeated fracture or where there is soft tissue trauma. The torus is removed via a split palatal mucoperiosteal flap, preserving the incisive neurovascular bundle, in order to fully expose the bony torus. Reflection of the flap over the torus is often difficult due to undercuts. The torus is sectioned with a fissure burr and each segment removed with an osteotome or chisel. Final smoothing is with a large bone-cutting burr. Following closure, a healing baseplate or pack may be placed to reduce the risk of a haematoma forming from the raw bone margins (Figure 4).
Ridge augmentation
The residual ridge may be built up using a variety of materials. These include bone autografts or allografts (or bone substitutes). The risks of viral and prion infections make the use of xenografts or cadaveric materials no longer acceptable. These grafts may be placed as either onlay or interpositional grafts.
The main complication of ridge augmentation is accelerated resorption of the graft. This is thought to be due to lack of an adequate soft tissue envelope resulting in little space for graft placement. The resulting tight tissue envelope is thought to produce loss of the graft. Techniques to improve the soft tissue space, such as periosteal release, can lead to loss of sulcus depth and attached mucosa. This means a later vestibuloplasty (see above) and graft in order to allow full use of the ridge height gained. A brief experiment with intraoral tissue expansion was never followed through, although it provided a theoretical technique to overcome this problem.
Complications of ridge augmentation, in addition to general post-operative complications of bleeding, bruising, swelling, and infection, may include:
- accelerated bone loss as discussed above;
- nerve injuries - surgical approaches close to the infraorbital and mental nerves may give transient or long standing altered sensation. Harvest of a bone graft from the chin may damage the branches of the incisive nerve to give paraesthesia of the gingivae of the lower labial segment. Harvest of bone from the retro-molar region may involve the inferior alveolar neurovascular bundle, with resultant mental paraesthesia;
- fracture - in a severely atrophic mandible, osteotomies for distraction osteogenesis may predispose to a pathological fracture;
- loss of soft tissue support - extensive stripping of the tissues around the chin can lead to loss of the muscle attachments, resulting in the chin no longer being supported and being displaced inferiorly giving an unacceptable profile (‘witch’s chin’).
When choosing the donor site for autografts, consideration should be given to the volume of bone required, the need for particulate or cortico-cancellous block and ease of harvest. There is evidence to suggest that donor bone of the same embryological type gives better results with less resorption. The bone of the residual alveolar ridge is membranous in origin. This supports the use of the retromolar regions or chin as intra-oral sites, which are readily available under local anaesthesia and are membranous in origin. Where large shaped cortico-cancellous blocks are required, anterior or posterior iliac crest proves the most suitable site, even though this is of endochondral origin.
Allographic materials are inorganic bone substitutes. These may be calcium phosphates or hydroxyapatites. There is significant experience using bovine bone, which has been treated to remove all organic material. These materials can be used alone or as a bulking agent for bone autografts.
These graft materials may be augmented by the use of platelet-rich plasma. The principles behind the use of platelet-rich plasma is the concentration of growth factors (endothelial derived growth factor (EDGF), vascular derived growth factor (VDGF), transforming growth factor-β2 group, including bone morphogenic protein (BMP)) in platelets. A sample of the patient’s blood is manipulated in a centrifuge to give 5 to 9 ml of plasma, which contains 2 million platelets. The effect of platelet-rich plasma is to give earlier vascularisation of the bone graft, which allows earlier and better bone consolidation. There are also soft tissue effects with improved healing (Figure 5).

An alternative is to use commercially prepared bone morphogenic protein, although this is expensive and excites a significant inflammatory response.
In Germany the most commonly used bone substitute is derived from bovine material which makes it a xenograft. There is a big lobby by the pharmaceutical companies for allo- and xenografts in Germany. Patients are receptive of the idea of using bone substitute material as it prevents donor site morbidity.
Distraction osteogenesis
The advent of distraction osteogenesis applied to the facial bones using the principles originally developed by Ilizarov is an alternative method of ridge augmentation which may overcome some of the problems associated with onlay or interpositional ridge augmentation. The surgical technique involves an osteotomy of the residual ridge to create a mobile segment. A distraction appliance is fitted and the wound closed. After a latency period the device is activated to increase the alveolar bone height along a predetermined vector. Once the planned amount of bone height increase has been reached, the device is left for a period of up to two months before it is removed. The advantages of this approach are the removal of the need for a second donor site and risks associated with the use of allografts. In addition to distraction osteogenesis, there is also distraction histogenesis increasing the soft tissue envelope, so reducing the risk of increased resorption. The technique does require two surgical procedures and the use of specialist devices with associated costs. Careful patient selection is necessary as sufficient bone must be present to allow the initial osteotomy. The rate of distraction is critical. If the distraction rate is too fast, wasting of the bone occurs. If the distraction rate is too slow, the transport disc fuses prematurely. This can be overcome by placing a platelet-rich plasma / bone graft interposed at the osteotomy site.
Orthognathic surgery in preprosthetic surgery
In cases where there is an existing skeletal anomaly, this can be further exaggerated by bone resorption. In particular resorption of the maxilla is both vertical and horizontal. Ridge augmentation (see above) alone may not be sufficient to allow for the satisfactory construction of conventional dentures. In these situations, consideration may be given to a combined augmentation and maxillary repositioning procedure. This will involve a Le Fort I advancement osteotomy with the insertion of an interpositional horseshoe cortico-cancellous bone graft to down-graft the residual ridge and give ridge augmentation. The planning of this procedure is similar to that for orthognathic surgery in dentate individuals, modified to take account of the proposed positioning of the incisal tips of the prosthesis.
Mandibular prognathism may be corrected by conventional setback osteotomies. There is a change in blood supply to the mandibular bone following the loss of teeth, and the potential effects this may have on healing. The advent of distraction osteogenesis has probably cast procedures such as the visor osteotomy to the history books.
Surgery for osseointegrated implants
Bone grafting is often required to provide sufficient height and / or width of the alveolus to allow implant placement. The commonest grafting procedures are sinus lifting and onlay grafting.
Sinus lifting is necessary where the floor of the maxillary antrum invaginates the residual alveolar ridge in the premolar region, reducing the amount of bone height required for placement of implants in this area. The surgical technique is similar to a Caldwell-Luc approach to the maxillary antrum. In the case of sinus lifting, the bone window is retained attached to the antral lining, which is carefully elevated from the antral floor to create a mucoperiosteal pocket (Figure 6).
Bone is placed into this pocket so raising the antral floor. Indirect closed sinus lifting can also be carried out at the time of implant placement if the amount of additional bone required is small. In this case the bone is prepared for the implant in the normal manner, taking care not to perforate the antral lining. The antral lining is lifted through the hole and bone graft packed into the prepared hole immediately before fixture placement. In the process of placing the fixture, the bone graft is forced under the antral lining giving the necessary support for the newly placed fixture.
Onlay grafting is required to increase residual alveolar ridge width and height. The anterior alveolus in particular resorbs both vertically and distally, giving a narrow palatal or lingually placed residual ridge. Onlay grafting allows for the restoration of normal ridge width and eliminates concavities, which may result in exposed implant threads.
Other techniques to increase residual bone height and width include cortico-cancellous block grafts and segmental distraction osteogenesis. Segmental distraction osteogenesis can be performed either before implant placement or, with special distraction implants, following fixture placement.
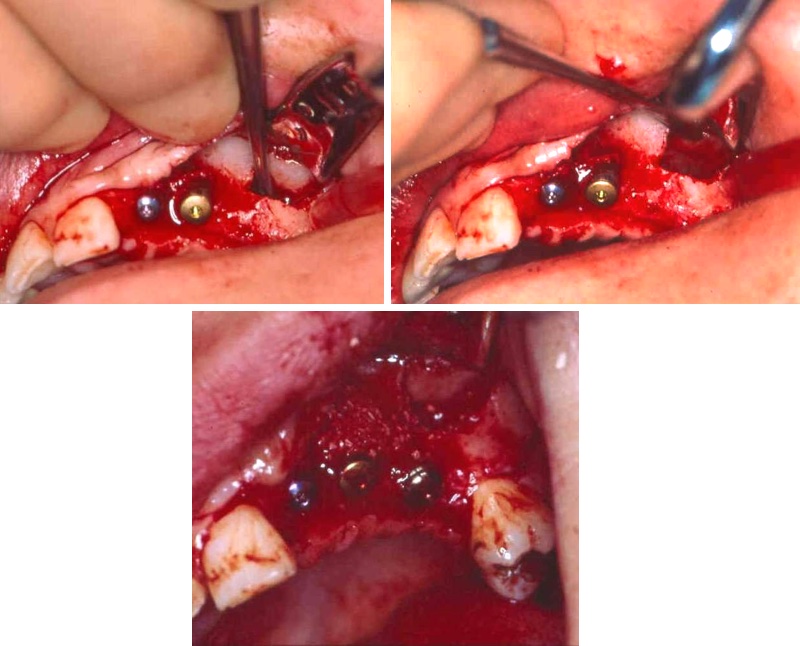
Individual implant placement
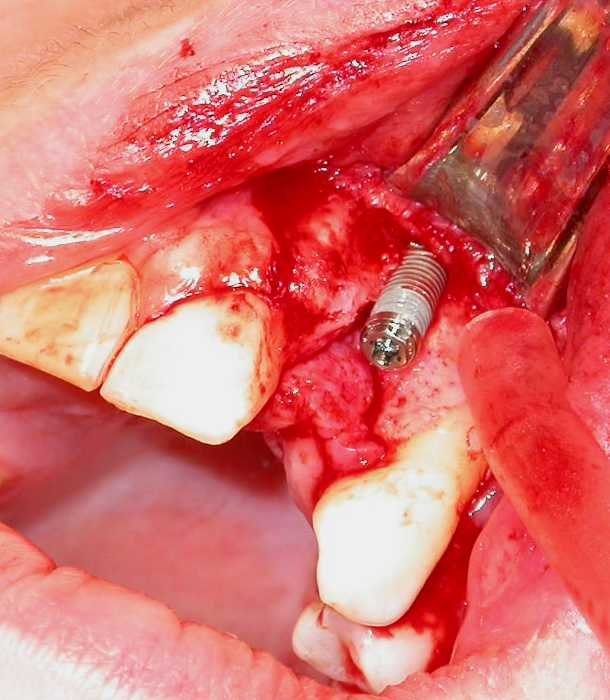
This is usually performed under local anaesthesia [treatment-surgery-anaesthesia-preamble] with or without sedation. The residual alveolar ridge is exposed by a crestal incision and mucoperiosteal flaps are raised medially and laterally. The bone is prepared by drilling at slow speed with meticulous irrigation to avoid osteocyte death caused by bone overheating. The implant site is prepared by sequentially increasing twist drill size to reach one just under the maximum diameter of the implant. Depending on bone density and implant design, the bone is tapped (prepared for a thread) before placing the implant. This is also done under coolant irrigation (Figure 7).
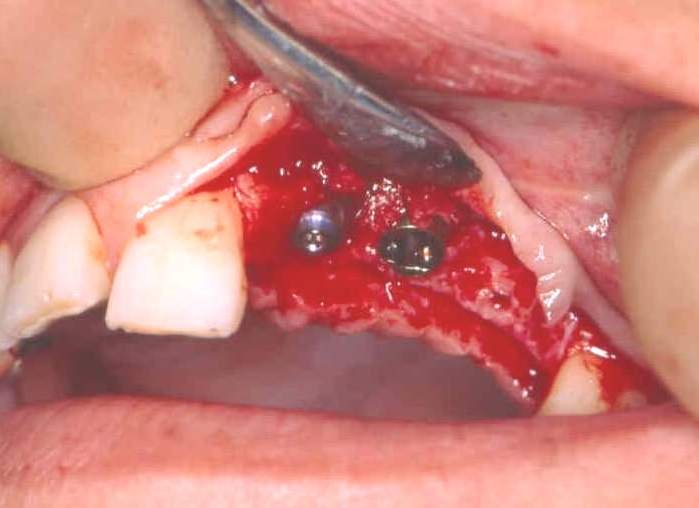
It is essential to avoid contamination of the pure titanium surface of the implant with stainless steel instruments or soft tissue. The implant is screwed into the bone at slow speed until the maximum torque is reached. Over-tightening can strip the implant from the bone. Sometimes exposed threads are seen on the buccal/labial aspect of the implant on final placement. If there is primary stability, the majority of implants will integrate despite exposed threads (Figure 8).
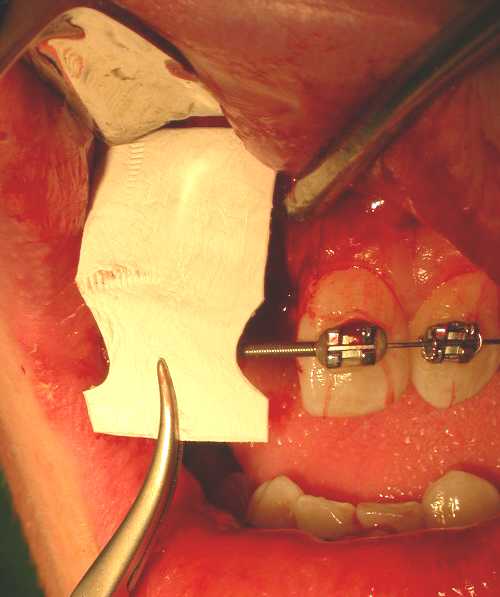
These threads can also be covered by bone harvested by a surgical filter or bone substitute. Semipermeable membrane covering this can promote healing by guided tissue regeneration (Figure 9). A cover screw is fitted over the internal threads of the implant (Figure 10) and the wound closed. The patient is advised not to wear their prosthesis for 7 to 10 days, followed by occasional wear only.
The time taken for integration depends on the quality of bone available at the implant site. It is generally accepted that an implant will integrate in 3 months in the mandible and in 3 to 6 months in the maxilla. Titanium oxide coatings on the threads of implants have reduced the integration time in the maxilla.
At second stage surgery, a small mucosal window is cut over the cover screw and the cover screw removed. Any covering bone is removed. A temporary ‘healing’ abutment is placed of a size which will allow suitable protrusion through the mucoperiosteum. This is left in place for a minimum of two weeks to allow the mucosal cuff to heal around the healing abutment. Once healing has occurred, the final abutment is placed and impressions taken of the fixture head for construction of the definitive prosthesis. The technique for implant placement is essentially the same for single and multiple implant restorations.
Surgery for prosthodontics in patients with head & neck cancer
Surgery for prosthodontics in patients with head and neck cancer should be considered at the time of planning for the ablative surgery. The eventual rehabilitation of the patient has to be considered at the time of initial resection and reconstruction but must not compromise the principles of oncological surgery. With this in mind, planning of flaps to restore tissue volume should bear in mind the eventual prosthetic rehabilitation with regard to appropriate bulk and preservation, where possible, of appropriate bone and soft tissue undercuts.
Complications of osseo-integrated implants
Apart from the traditional peri-operative complications associated with any minor oral surgical procedure (such as bruising, swelling, risk of infection and bleeding), there are few special complications associated with osseointegrated implants. In the placement of implants in the anterior mandible, in particular where using ‘same day teeth’ techniques, the preparation of the bone for the implant often involves perforation of the cortical bone of the lower border of the mandible. This comes with the risk of localised cutaneous bruising. Similarly, in placement of the implants in the anterior maxilla, the cortical bone of the nasal floor is often utilised, with the possibility of bruising around the nose and nasal stuffiness.
In all cases there is the possibility of the implant failing to integrate. This is usually detected at the time of second stage surgery, and where attempts to remove the cover screw lead to unscrewing of the implant. In this situation the bone is allowed to heal and the implant can usually be replaced after allowing three months for bone to regenerate.
It is normally expected that there is a small amount of bone loss around implants in the order of less than 0.1 mm per year. Where there is excessive loading of the implant-retained prosthesis or exceptionally poor oral hygiene, inflammation of the mucosal cuff around the implant abutment may be seen with localised bone loss at the pocket formation. This peri-implantitis is usually reversible with judicious oral hygiene measures and professional scaling, although it may lead to eventual implant loss.