Dry mouth
Xerostomia
Dry-mouth treatment by medication
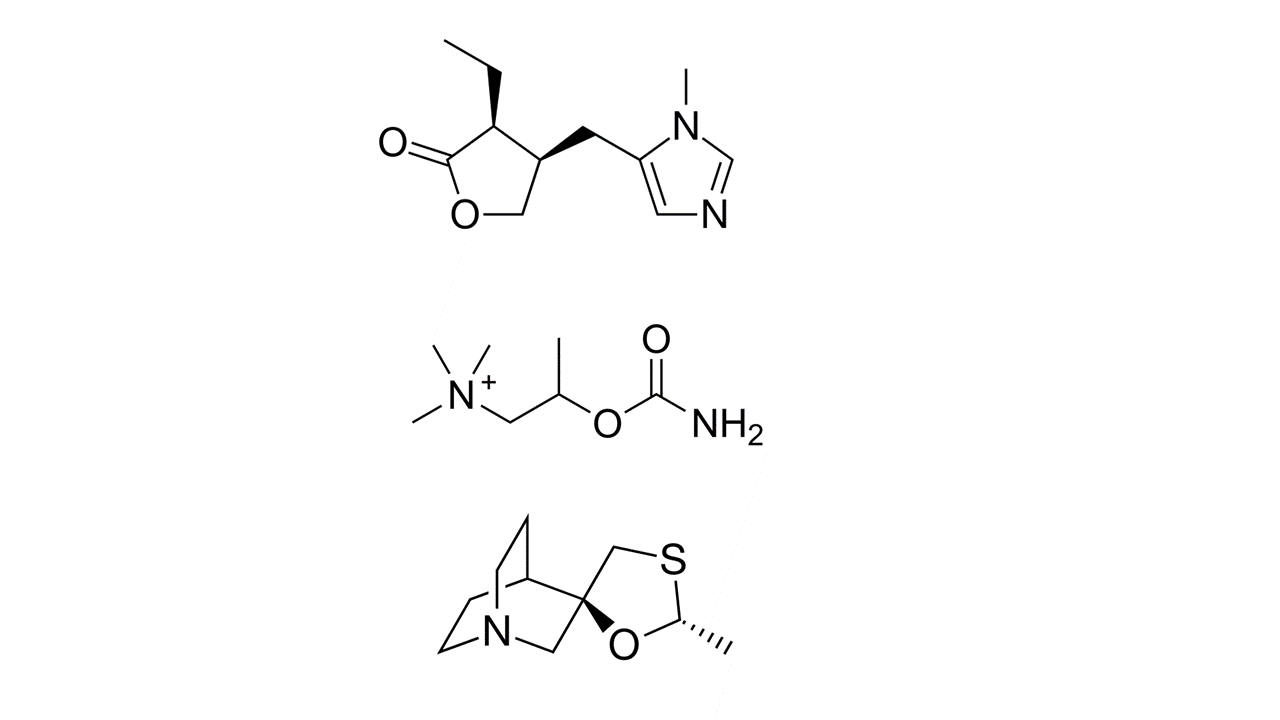
Dry mouth is usually a chronic complaint which is often not helped by medications or treatments. Pharmaceuticals are usually mimics of the parasympathetic transmitter acetylcholine and so while they will cause an increase in salivation they can also cause other effects such as sweating, nausea and increased urinary flow. Pilocarpine, bethanechol and cevimeline are three of the more commonly used such medications (see Figure 1).
These medications (sialogogues) have common and serious unwanted effects because the receptors they act on to achieve the wanted effect (increased salivation) are not specific to the salivary glands. In fact, pilocarpine is a drug that has been known for over 100 years and is also used (in the form of topical preparations) to treat eye conditions (glaucoma), where excessive production of saliva and sweat have to be considered as unwanted effects. The number of remaining functional acinar (secreting) cells in damaged salivary glands determines how well these drugs can stimulate salivation rates.
Treatments in the form of artificial salivas are readily available from pharmacists but are often too transient to be of great benefit. It is important to look for preparations which contain fluoride ions and are not acidic (some artifical salivas are acidic).
Anything which stimulates the sense of taste will cause an increase in salivary flow but care is needed to avoid cariogenic foods (sugar in particular; also beware of hidden sugar in low fat and other highly processed foods, they all contain added sugar, sometimes in substantial quantities). So sugar-free mints / sweets can be useful. Maintaining hydration by drinking water would appear to be essential although conversely drinking water can exacerbate dry mouth symptoms (because drinking lots of water or continually sipping water, washes away any precious remaining saliva production). Chewing sugar-free gum can also increase salivary flow and relieve dry mouth to a certain extent. Other ideas and alternatives to keep the mouth moist and stay hydrated can be found in our detailed section about practical tips around oral food intake.
If the occurrence of a dry mouth has coincided with the starting of a new medication, that medication is likely to be the cause. A discussion with the prescribing clinician may allow an alternative drug treatment that doesn’t cause xerostomia.
Attempts to avoid xerostomia as a long-term effect of radiotherapy
With a view to reducing the long-term adverse effects of high-energy radiation delivered to healthy tissues of the head & neck region (such as xerostomia, but also including dysphagia, trismus and osteoradionecrosis), much effort has been devoted to develop more selective irradiation schemes. Intensity-modulated radiotherapy (IMRT) irradiation schemes have the potential to spare crucial structures (for example, salivary glands) from exposure to high radiation doses while being able to better shape the high-level irradiation to the target volume. These modulated irradiation schemes have become standard radiotherapy treatment approaches over the past 10 to 15 years. IMRT schemes have been shown to reduce long-term problems with xerostomia. However, wider structures that would not have been exposed to high-energy radiation in conventional irradiation schemes (for example, front of mouth and tip of tongue) in IMRT schemes are exposed to lower-level irradiation (‘dose bath’).
In some selected circumstances it may make sense to temporarily surgically relocate the submandibular salivary gland to the submental space (under the chin), outside the planned irradiation field. It has been shown that this method prevents radiation-induced xerostomia and preserves the function of the gland in the majority of people treated in this way. However, this method is only feasible for a small subsection of head & neck cancer cases and thus is rarely used, having only a practical role in laryngeal cancer.
Some customised mouth-opening devices (intraoral stents) have been shown to reduce radiation damage to healthy tissue simply by, for example, increasing the distance between upper (maxilla) and lower jaw (mandible), as well as immobilising the mandible for the duration of an irradiation session. The exact degree of benefit from such otherwise easy to manufacture devices remains to be evaluated.
Many substances have been, and continue to be, researched as candidates to act as ‘protectants’, that is as chemical or biochemical agents that help to prevent or reduce radiation damage to healthy cells and tissues in general, including the reduction of severity and duration of xerostomia resulting from head & neck radiotherapy schemes. Of the many such agents investigated, so far only amistofine (see Figure 2) has some track-record as a promising protectant. It has been shown that amistofine does reduce severity of xerostomia during radiotherapy treatment periods; the long-term protective effects are less clear. The fact that amistofine is a prodrug which relies on a specific hydrolysis mechanism for activation not likely to be active in malignant cell lines, makes this chemical the currently most promising candidate as a protective agent. Trials have shown that amistofine does not compromise local tumour control by radiotherapy. However, amistofine causes severe other unwanted effects and its use requires careful clinical monitoring.
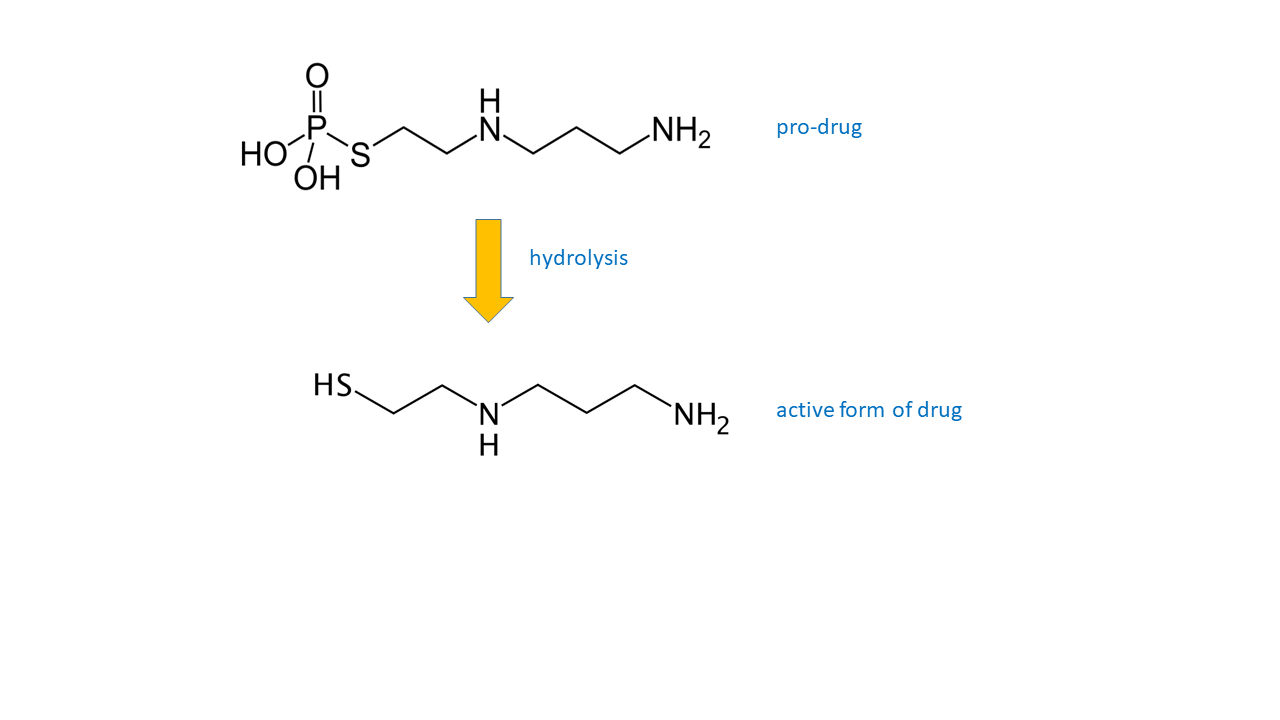
Other biochemical agents are being investigated for similar radiation-protection purposes (for example, keratinocyte growth factor (palifermin)) in the hope to find drug candidates with fewer or less severe unwanted effects while maintaining a high level of cell-protection in healthy tissues. These searches and suggestions include some not entirely convincing examples, with little or no supporting evidence. The major hurdle and caveat in these investigations is to ensure that the agent i) does protect healthy cell lines, and ii) that it solely protects healthy cell lines from radiation damage but not malignant cell lines. For the time being, amistofine is the only agent for which some conclusive evidence exists.
On the pre-clinical research front, autologous stem cell transplantation has been proposed as a prevention of long-term xerostomia caused by radiation damage to salivary glands. In animal models, stem cells from submandibular and parotid glands were collected prior to irradiation. When transplanted back into salivary glands after the radiotherapy cycle, these stem cells differentiated into functional salivary gland cells and regenerated salivary-gland function. If these pre-clinical studies can be translated to clinical practice, this approach would hold promise and would not be marred by the many and serious unwanted effects of the other, current prevention strategies.
Management of (and self-help for) dry mouth
Whatever the cause of dry mouth, rigorous oral health regimes are necessary to prevent the rapid progression of caries. Saliva is the natural protector of teeth from decay. A pro-active dental-care regimen, especially involving dental hygienists, brushing morning and night with a fluoride containing toothpaste (see our video demonstrations), avoiding sugary foods, always having a glass of water with any meals and snacks (more for rinsing the mouth to remove some minor food debris, than for helping with swallowing) are sensible precautions.
As well as dental caries, dental erosion is increased in dry mouth. Erosion of dental enamel is normally prevented by the presence of Ca2+ ions in saliva, in the absence of the sticky protecting type of saliva, teeth are more vulnerable to the loss of calcium ions, leading to erosion. So acidic foods are best avoided or should at least be consumed with water. Changes in taste and palatability of foods may occur with dry mouth to such an extent that malnutrition or dehydration may occur. These consequences of dry-mouth problems are usually exacerbated by difficulties with swallowing due to lack of the lubricating properties of saliva.