Bone lesion
We keep the following subdivision of bone lesions and their treatments:
- inflammatory (including bone infections) and other non-neoplastic bone lesions;
- benign neoplastic bone lesions (benign bone tumours);
- malignant neoplastic bone lesions (bone cancers)
and look next into treatment options for individual conditions within each of the three categories of bone lesions.
Infections, inflammatory and other non-neoplastic bone lesions
Dry socket (alveolar osteitis)
The treatment of localised dry socket (alveolar osteitis) consists mainly of local treatments. If the application of local anaesthetics can be tolerated, then cleaning out of the socket and dressing it with a resorbable commercial antiseptic or analgesic pack will often be all that is needed. If these packs do not work, then an alternative pack made up of cotton wool, a small amount of zinc oxide (an effective topical anti-inflammatory agent) and eugenol (the main component of clove oil) will provide pain relief. This pack will have to be removed and sometimes has to be replaced, but it is almost unique in providing complete pain relief from intractable dry socket pain.
If the application of local anaesthetics cannot be tolerated, then provision of systemic antibacterial medication such as metronidazole (effective in treating infections by a range of anaerobic bacteria) and systemic analgesics (mainly nonsteroidal anti-inflammatory drugs, (NSAIDs), such as ibuprofen, with or without codeine/paracetamol) is just about all that can be achieved.
It is worth noting that some people seem to be much more prone to this condition than others.
Osteomyelitis
The term osteomyelitis covers a fair range of inflammatory bone conditions, typically evolving from some initial bacterial infection of dental origin but may also lack any frank (or obscure) infectious origin. Osteomyelitis may be suppurative or non-suppurative (producing pus, or not). In addition, there are different forms of acute and chronic osteomyelitis. The corresponding treatment options reflect this diversity.
The general management of acute osteomyelitis includes the correction of any underlying systemic factors and potential causes; this is vital. Routine investigations should include:
- full blood count
- routine biochemistry tests, including blood glucose
- C-reactive protein (CRP) +/- ESR
- blood cultures.
If somebody is systemically unwell, then intravenous application of antibacterial agents should be started. Penicillin and flucloxacillin are a good best guess; clindamycin is used when somebody is allergic to, or intolerant of, penicillin and penicillin derivatives. If necessary, the antibacterial agent(s) can be changed when bacterial culture results are available and suggest a different agent.
Surgical treatment includes the drainage of pus and the removal of any focus of infection (such as tooth, foreign body). In established cases, saucerization (excavation of tissue) and decortication (removal of surface layer of bone (the hard, cortical bone layer)) may be necessary to allow coverage of the medullary space (the inner channel of bone) by well vascularised (supplied with blood vessels) soft tissue. Measurement of the CRP count helps to monitor the response to treatment.
Resection of any bone sequestrum (piece of dead bone) or clinically ischaemic (lacking blood supply) bone is particularly important in the type of osteomyelitis caused by radiation or medicinal drugs. This may be helped by packing of the resulting defect with a collagen ‘fleece’ impregnated with gentamycin (an antibacterial agent). The remaining bone must be covered with sealed healthy vascularised tissue whenever possible.
In pathological fractures associated with osteomyelitis, rigid fixation is shown to improve healing. In those cases involving bone damage by radiation or medicinal drugs, fresh vascularised bone and soft tissue to create watertight seals around healing bone are generally advocated.
Chronic osteomyelitis
Treatments are the same as for acute osteomyelitis (see above). All correctable host factors for infection should be addressed. Hyperbaric oxygen therapy, HBO may be of value in refractory cases, particularly those associated with previous radiotherapy. However, there is no conclusive evidence about the efficacy of HBO for this condition.
Garré’s’ sclerosing osteomyelitis
Any source of infection should be removed, sometimes this has to be surprisingly radical. Antibacterial agents are not helpful. Remodelling of the bone is the rule, but surgical re-contouring may be needed.
Chronic sclerosing osteomyelitis
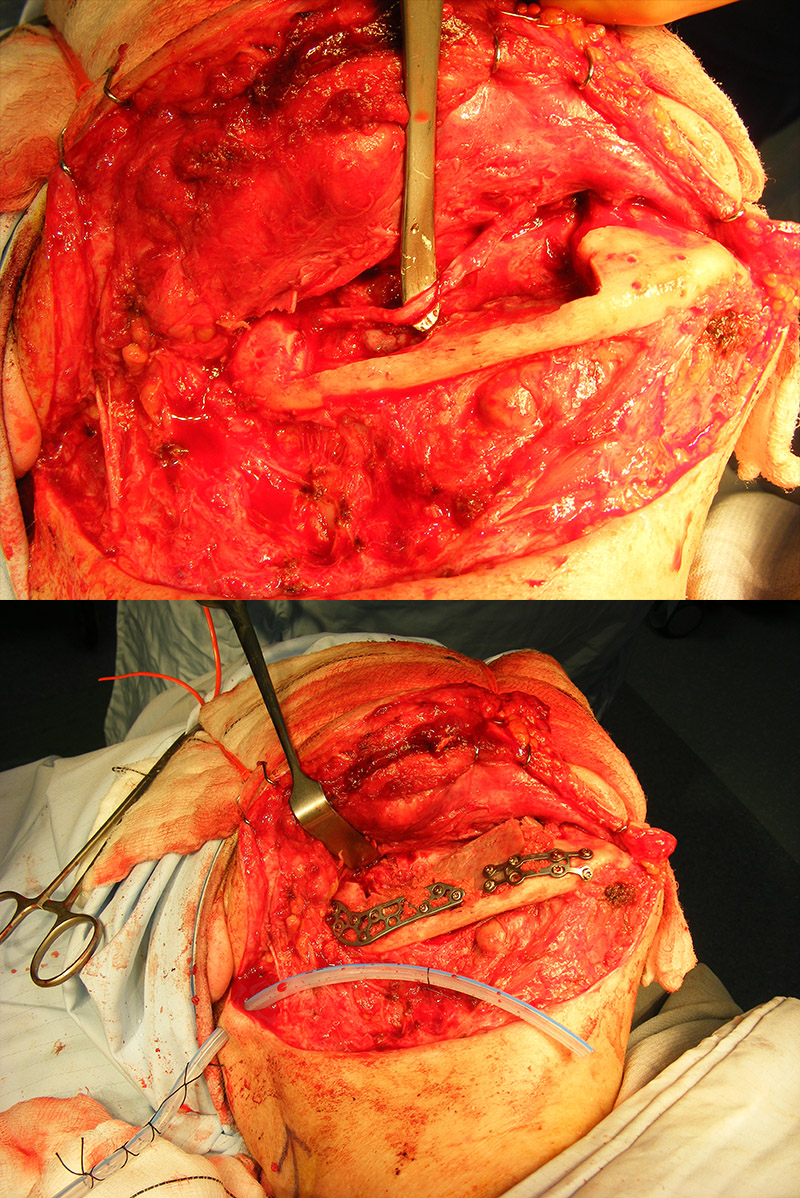
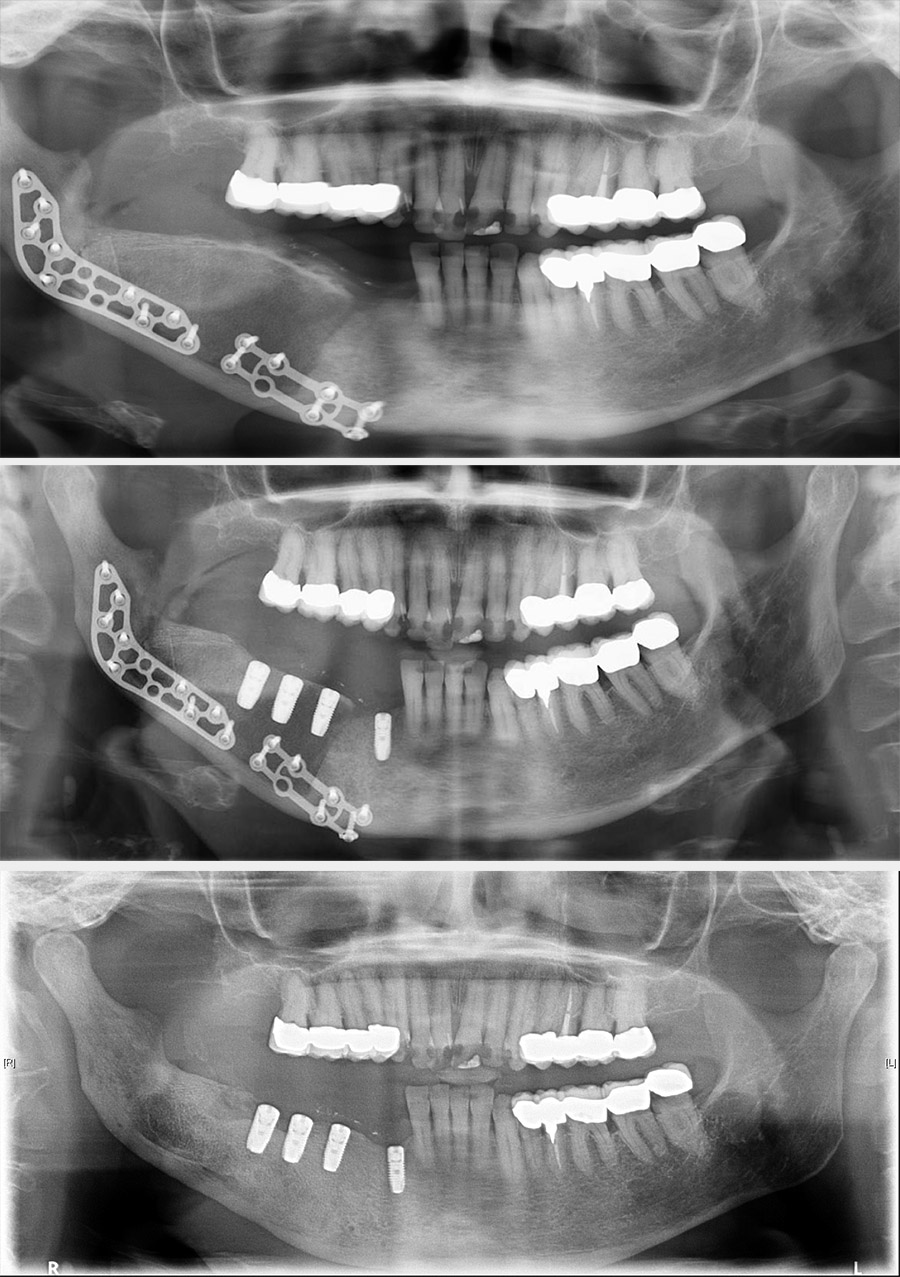
Treatment can be problematic. Long-term antibacterial therapy has been reported as being of benefit if given early in the course of the disease, but there are also reports that high-dose long-term antibacterial therapy has no beneficial effects. In more refractory cases, a course of corticosteroids and decortication may be of benefit. Hyperbaric oxygen therapy can be used to supplement the surgery although the evidence base is conflicting. Bisphosphonates have been advocated for chronic pain but have obvious conflicting risks regarding development of osteonecrosis. In some cases, more radical surgical intervention is required, such as resection of the affected region of the mandible (Figure 1 and Figure 2; note that the surgical techniques are essentially the same for some benign and malignant (see below) conditions).
The real problems are the management of pain, which may be due to some form of autonomic dysfunction (a degree of malfunction of involuntary nerve actions).
Cysts
Fibrous dysplasia and ossifying fibroma
Treatment should wait until completion of growth because this is a hamartomatous problem (a benign malformation that evolves at the same rate as normal body growth in infants). Resculpting of the malformation is best achieved after growth is completed.
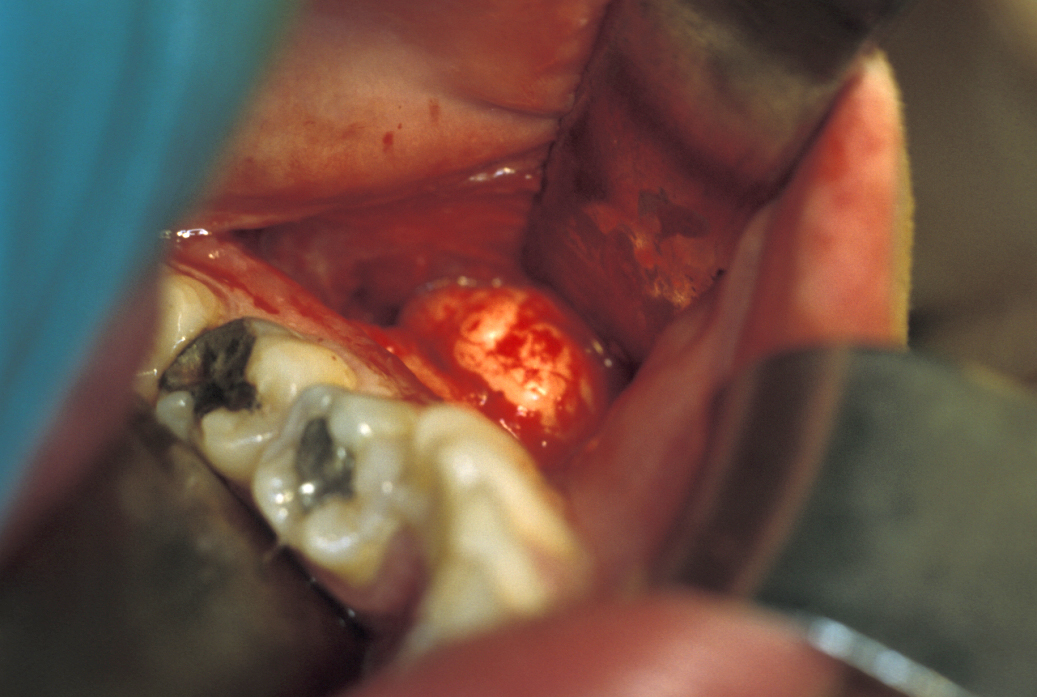
Ossifying fibroma is thought to be a localised, benign tumour, variant of fibrous dysplasia. The lesion can usually be safely enucleated (removed) within its fibrous envelope (see Figure 3 for an example). Significant bone resection is not necessary.

Osteopetrosis
There is no cure for this rare inherited condition. The milder form of the condition in adults is often without symptoms but may require surgical intervention if over time facial disfigurement or dysfunction develops. The severe form of the condition in infants typically is fatal within approximately 10 years.
Paget’s disease of bone
Treatment is complex and in the absence of symptoms there may be no need for treatment. If, however, there is need to treat the condition, the management is by medication. The medications most commonly used are bisphosponates (otherwise a common type of medication to treat osteoporosis). The risk of bisphosphonate-related osteonecrosis of the jaw associated with this treatment of Paget’s disease of bone is of obvious relevance. An alternative medication may be calcitonin. Calcitonin is a hormone that is involved in the regulation of the calcium metabolism as well as the general regeneration metabolism of bones.
Very rarely, surgical intervention may be required to correct bone deformation(s), for example to reduce pressure on nerves.
Benign neoplastic bone lesions (benign bone tumours)
Ameloblastoma (unicystic, follicular/plexiform, and peripheral)
Ameloblastoma has a range of pathological behaviours, based on local destructiveness and propensity for recurrence. These tumours do not metastasise but do need wide local excision and sometimes reconstructive surgery.
Treatment of unicystic ameloblastoma consists of ‘radical’ enucleation, in which a margin of the surrounding bone is resected or otherwise treated (cryosurgery, Carnoy’s solution (‘chemical curettage’). This is similar to the treatment of recurrent keratocystic odontogenic tumours.
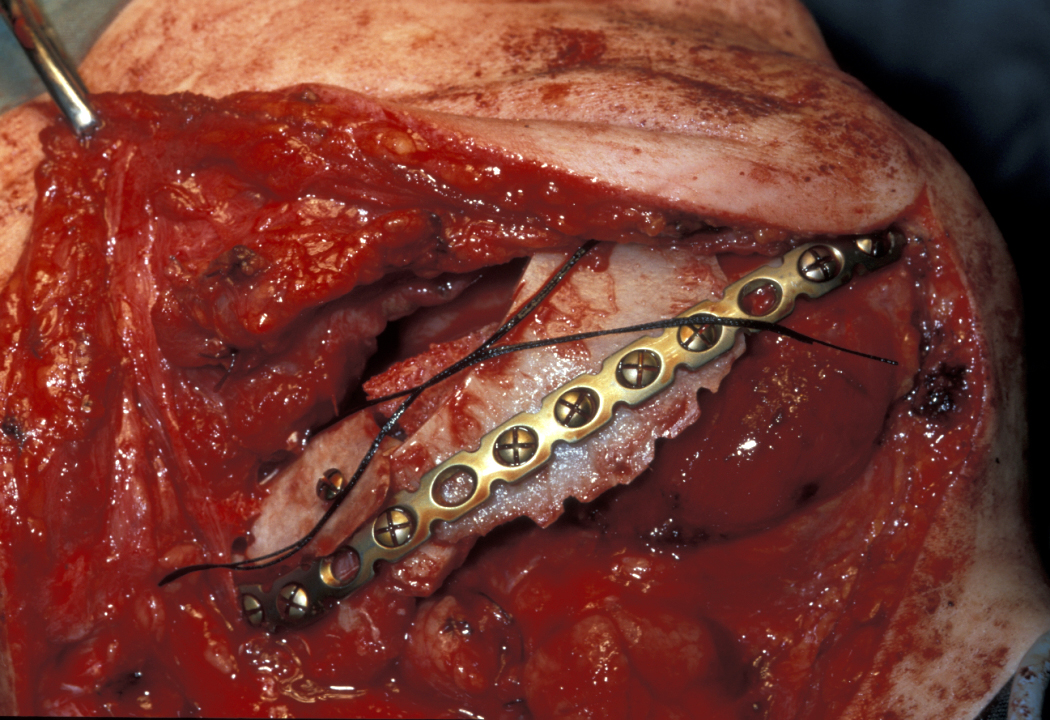
For the treatment of follicular/plexiform ameloblastoma, conventional bone resection is performed with a small margin (0.5 cm), preserving vital structures when possible. Segmental resection may be necessary, and bone and nerve grafting may be necessary to repair the mandibular discontinuity after segmental mandibular resection (see Figure 4).
The (rare) extraosseous soft-tissue version of ameloblastoma, peripheral ameloblastoma, is treated by subperiosteal (beneath the dense connective tissue enveloping bone) soft tissue excision with a 0.5 cm margin of normal tissue.
Other odontogenic benign tumours (such as adenoameloblastoma, myxoma, or ameloblastic fibroma) are all extremely rare. They are all managed by conservative excision.
Bizarre parosteal osteochondromatous proliferation (Nora’s lesion)
Resection with a very limited margin is usually used but there is no real certainty about the best form of treatment.
Giant cell granuloma of bone
Treatment of this intrabony swelling is the same as for its soft-tissue counterpart, by excision. In the United States there are some clinicians who manage these lesions by intralesional application of corticosteroids, calcitonin or interferon; these medical management approaches are not in use in the UK or Europe.
Osteoma / Gardner’s syndrome
Treatment of this benign tumour of bone consists of local excision, Figure 5 depicts an example of resection of a mandibular osteoma.
Torus
These entirely benign bony exostoses (outgrowth of cartilaginous tissue on a bone) require removal only if somebody is very concerned about them, or in preparation for prosthesis. Significant exostoses may require excision both for diagnostic purposes and/or for reasons of symptom relief.
Malignant neoplastic bone lesions (bone cancers)
Treatment for all of the rare primary bone malignancies (including osteosarcoma, osteogenic sarcoma in cystic cavities, Ewing sarcoma, chondrosarcoma, ameloblastic carcinoma) in the head and neck region is essentially the same. The first line treatment is radical resection. In most cases there will be substantial defects that will require reconstruction in order to restore functionality. Where the mandible is involved, in some cases it is possible to preserve continuity of the mandible (a so-called rim resection; see Figure 1 above), otherwise a segmental resection (see Figure 4 above) causes discontinuity of the mandible. The former is desirable in terms of superior functional results but must only be used if the required degree of radical resection is not compromised.
Neck dissection is standard practice in node positive patients (with malignant deposits in the lymph nodes), or when access to neck vessels (even if nodes are negative on imaging) is required for reconstruction. Postoperative radiotherapy is used if margins are close (less than 5 mm, or multiple positive lymph nodes found on histopathological examination after neck dissection, or extracapsular spread is found in common with other head and neck malignancy).