Ectopic (displaced) teeth
Contents
Impacted and ectopic teeth
Third molar teeth (wisdom teeth)
Surgical removal of a third molar or ‘wisdom’ tooth is one of the most common procedures undertaken in oral and maxillofacial practice. It is also a common cause for litigation. In the UK, even the indications for removal of third molar teeth excited controversy, although this has now been addressed by guidelines developed both by the British Association of Oral and Maxillofacial Surgeons and the National Institute for Clinical Excellence. The UK guidelines were reviewed in 2014. The German Society of Oral and Maxillofacial Surgeons guidelines (2013) are fairly similar. Many other countries have devised their own guidelines and there is a lack of international consensus on when and when not to remove third molar teeth. The American Association of Oral and Maxillofacial Surgeons views are quite different from the European views. The safest way to remove wisdom teeth is a source of continual controversy, in particular how the lingual nerve is best protected.
If surgical removal of a third molar tooth is necessary, the surgeon needs to decide:
- the path of withdrawal;
- obstructions to this path – do they need to be removed or left;
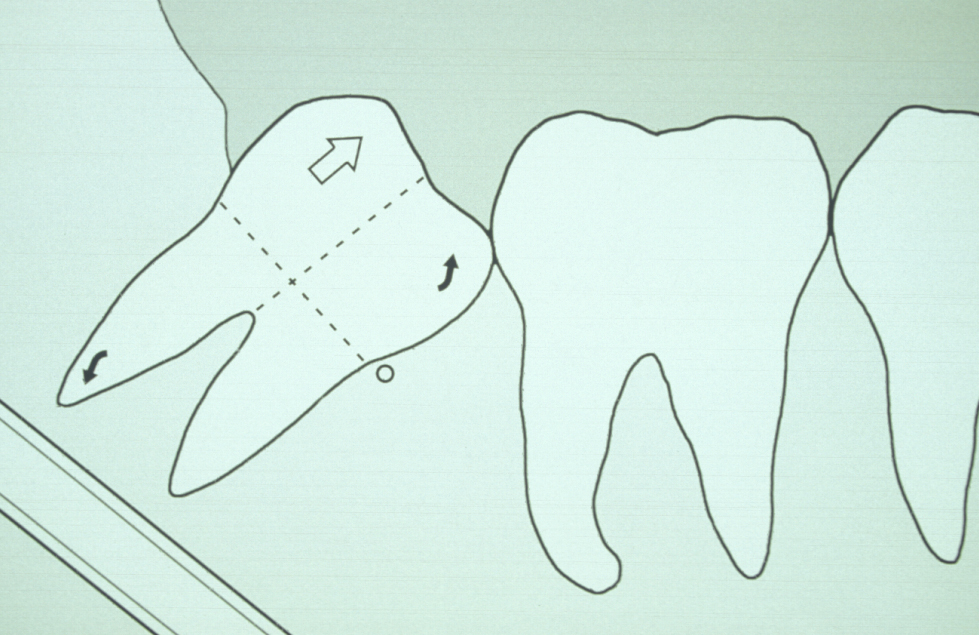
- the amount of bone which needs to be removed to allow application of an elevator (Figure 1);
- the direction of withdrawal (distoangular teeth are renowned for looking easy radiographically, but being much harder to remove);
- is the tooth best divided and removed in pieces.
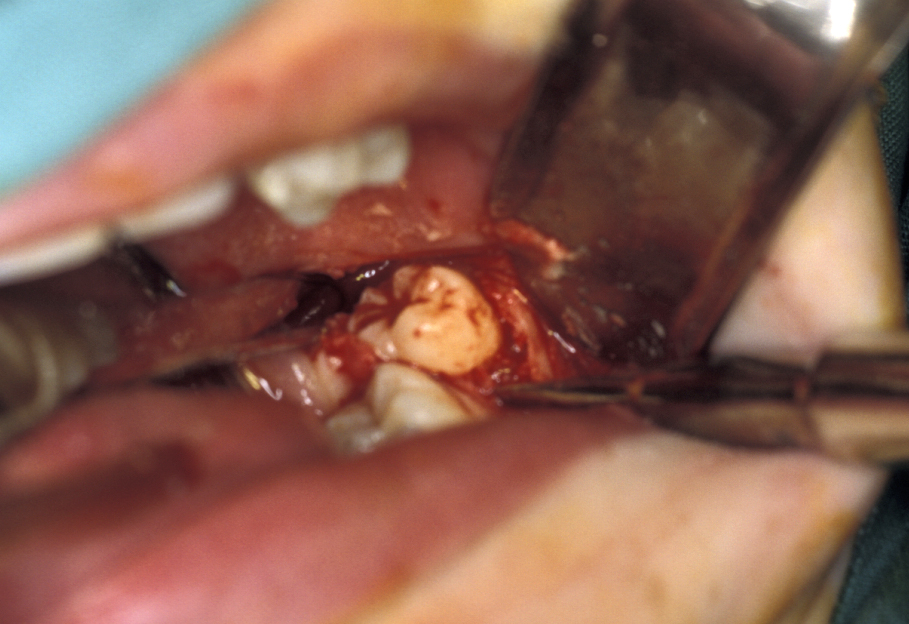
With experience, many of these points are determined intuitively by careful examination of the radiograph. Removing the third molar tooth is really removing the impediments and applying correctly orientated force (Figure 2).
Surgical technique for the removal of lower third molars carries some controversial aspects. Should a lingual flap be raised, should burrs or chisels be used, should systemic antibacterial agents be prescribed (if so, when for how long), should steroids be prescribed? Given this is such a common operation it is astonishing that there have not been adequately powered randomised controlled trials and a huge dataset for meta-analyses. For these, and many other points, there are no hard and fast rules. What seems to be emerging from the literature is that some techniques work well for some individuals and should therefore be encouraged. Only by supervised training and carefully conducted audit can these issues be answered and safe techniques developed for each surgeon.
The various stages in the technique are:
- Anaesthesia – local anaesthesia helps haemostasis and postoperative pain relief, even if the surgery is carried out under a general anaesthetic. This involves local infiltration where the flap is to be raised; some surgeons will augment this with a nerve block even if the procedure is carried out under is a general anaesthetic.
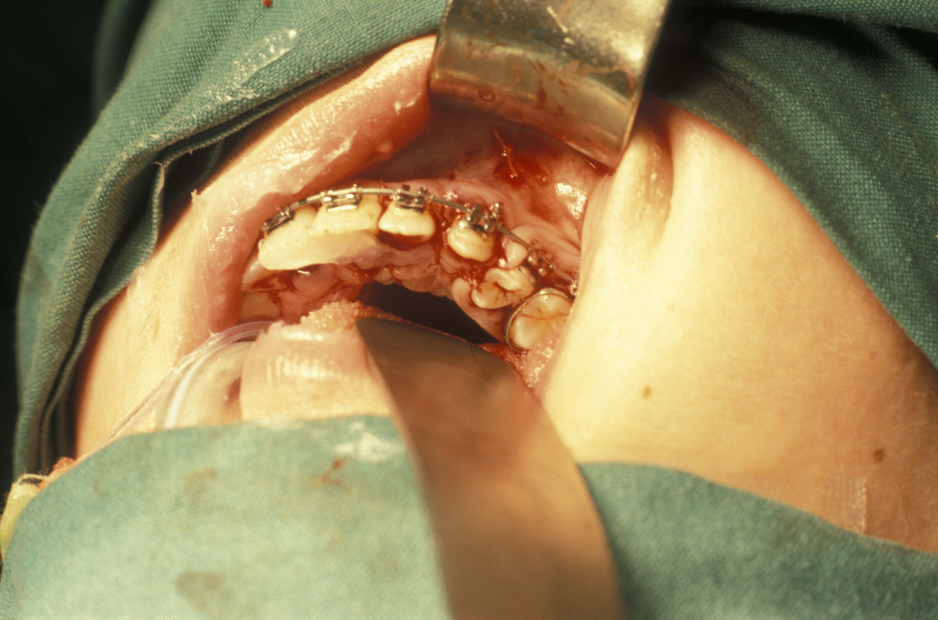
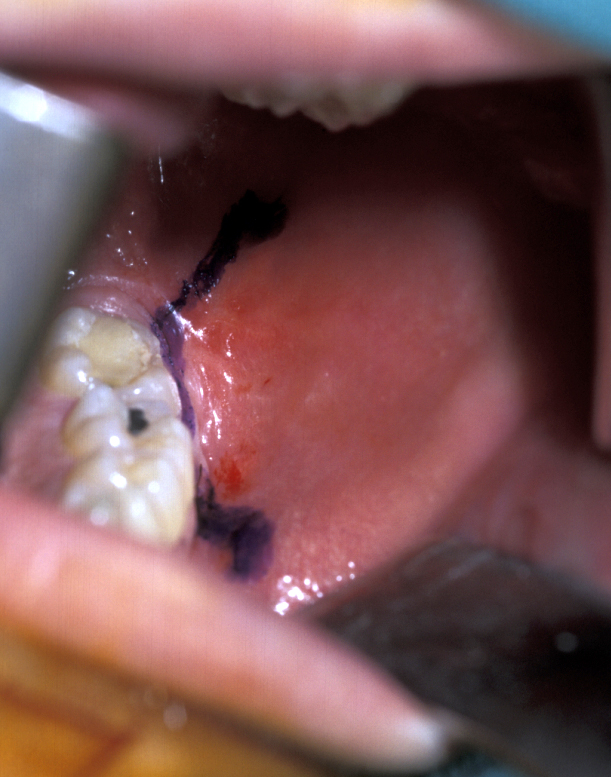
- Buccal Flap – a full thickness mucoperiosteal flap is raised from the buccal surface of the wisdom tooth area. The choice of incision varies, but commonly involves an incision along the external oblique ridge passing forward either around the second molar tooth or out into the buccal sulcus (Figure 3). If little or no bone is to be removed, a simple relieving incision may be all that is necessary. The important point is that dissection proceeds in a subperiosteal plane as this minimises postoperative swelling and trismus (Figure 4).

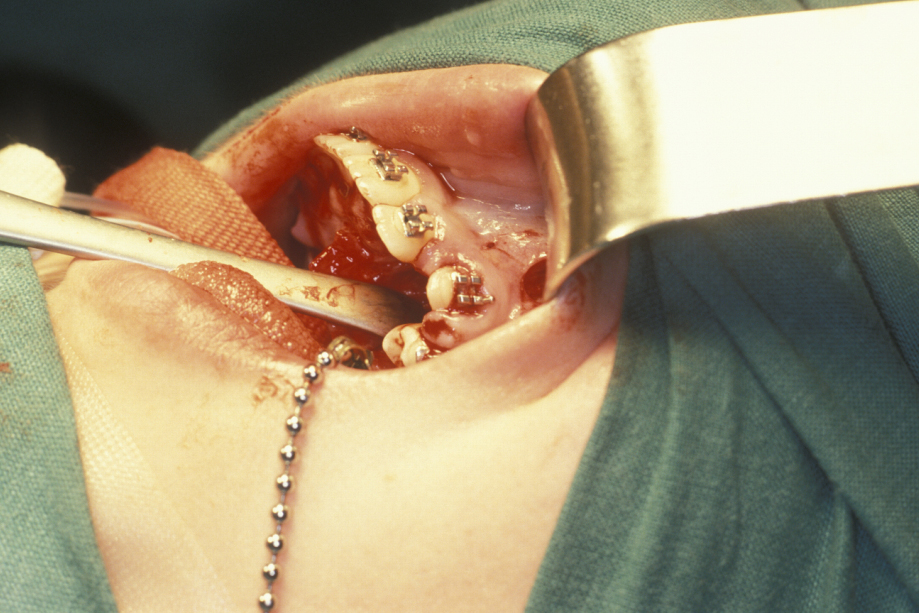
- Lingual Flap – some authorities do not raise a lingual flap at all. The popularity of this approach was from the days when accurate very high-speed surgical drills were not available and the ‘lingual split bone’ technique was popular in the UK and areas influenced by UK training. Their argument is that it is the process of actually raising the flap that causes injury to the lingual nerve. On the other hand, it is argued that the nerve is at risk from direct trauma from the burr/chisel if it is not retracted. Again, if used, the flap is raised by subperiosteal dissection. Here it is important not to ‘bow-string’ the nerve over the retractor (usually a Howarth’s elevator; Figure 1), but to widely undermine the lingual periosteum to allow the tissues to lie passively and use a wide subperiosteally placed retractor. The elevation of a small cuff of distal attached mucosa is designed for visibility, not for ‘lingual nerve protection’ and is not associated with an increase in morbidity (Figure 5).

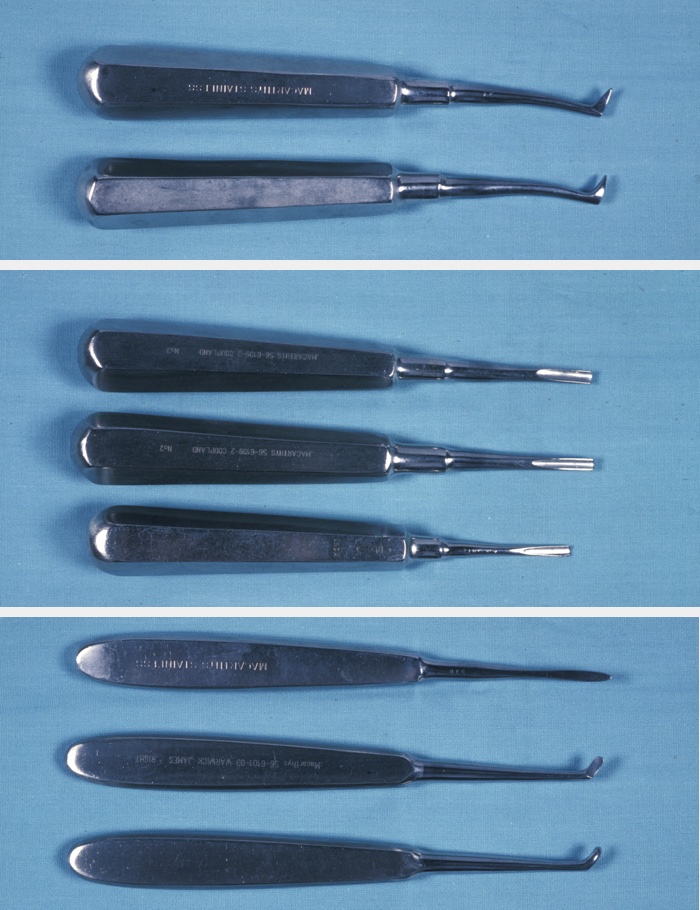
- Bone removal – this is usually done with either a burr (Figure 6) or (rarely now) chisels. A piezoelectric saw has been used but much less commonly. How much bone needs to be removed depends on the position of the tooth. Care is required to ensure that enough bone remains to support the second molar tooth. If chisels are used, mesial and distal stop cuts need to be placed to prevent fracture propagation (Figure 7).


- Tooth removal – in less impacted cases a point of application may be drilled into the tooth, which is then elevated out of the socket (Figure 8). It is important not to lever the tooth out as any resistance may change the fulcrum of elevation and result in the inferior dental nerve being crushed. If the tooth does not elevate it may be better to divide it and remove it in pieces. This is where the unprotected lingual nerve may be damaged if the burr is passed too deeply.
- Coronectomy - there has been a reinvention of the concept of decoronation for third molars which are coronally symptomatic (causing pericoronitis (inflammation and/or infection) or caries) but have significant risk of neurological damage associated with the operation to remove the tooth conventionally. In these cases, some surgeons simply remove the crown through the amelodentinal junction (boundary between enamel and underlying dentin), reduce the root surface to allow 2 mm of alveolar bone above the resection line and either close the wound or place an antiseptic pack. This was a popular preprosthetic technique many years ago, the retained roots preserving alveolar bone. The obvious risk is infection of the retained root at some time in the future. Clinical trials have suggested that coronectomy carries a lower risk of damage to the inferior alveolar nerve, with no increase in symptoms related to the retained root, which sometimes migrates coronally at least in short term follow up. Whether or not coronectomy becomes as common as conventional third molar removal remains to be seen.
Residual follicle is removed by curettage working on the bone of the socket, taking care if the inferior alveolar nerve is exposed in the base of the socket. Bone spicules are smoothed and bone dust is washed from under the periosteal flap. Irrigation of the socket may be counterproductive if a healthy clot is forming. All last remnants must be irrigated out from under the periosteum (Figure 9).

- Closure - free mucosa is sutured to fixed mucosa with one or two resorbable sutures only. A pressure pack is applied to create a clot. This is not first-intention healing in most cases; the flap protects the clot and allows the socket to granulate (Figure 10).

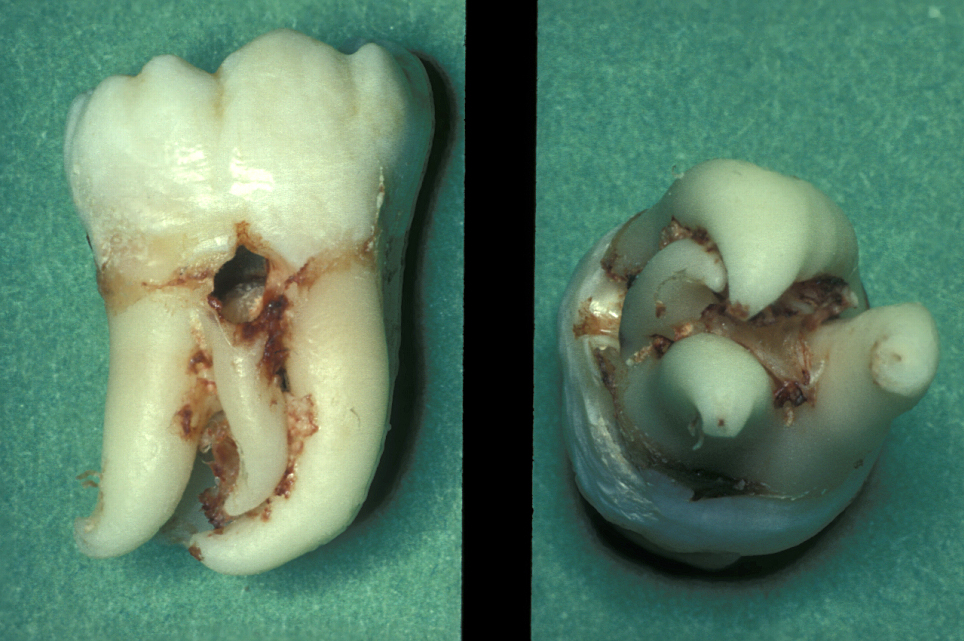
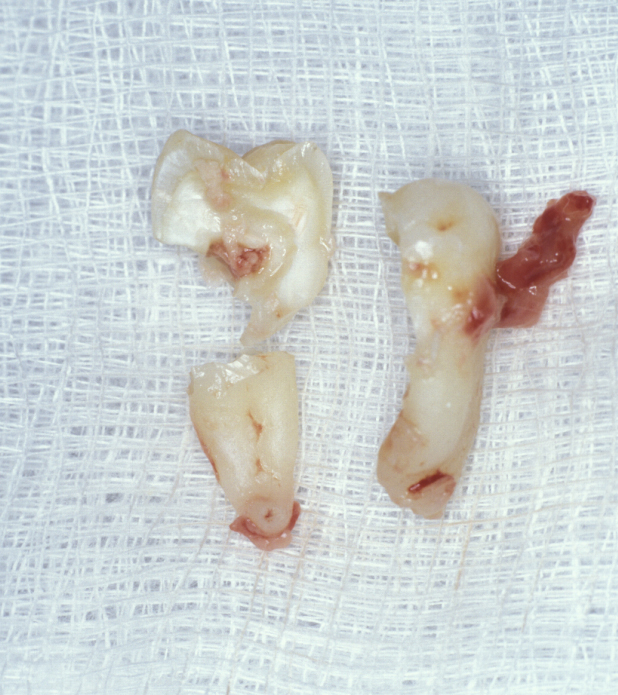
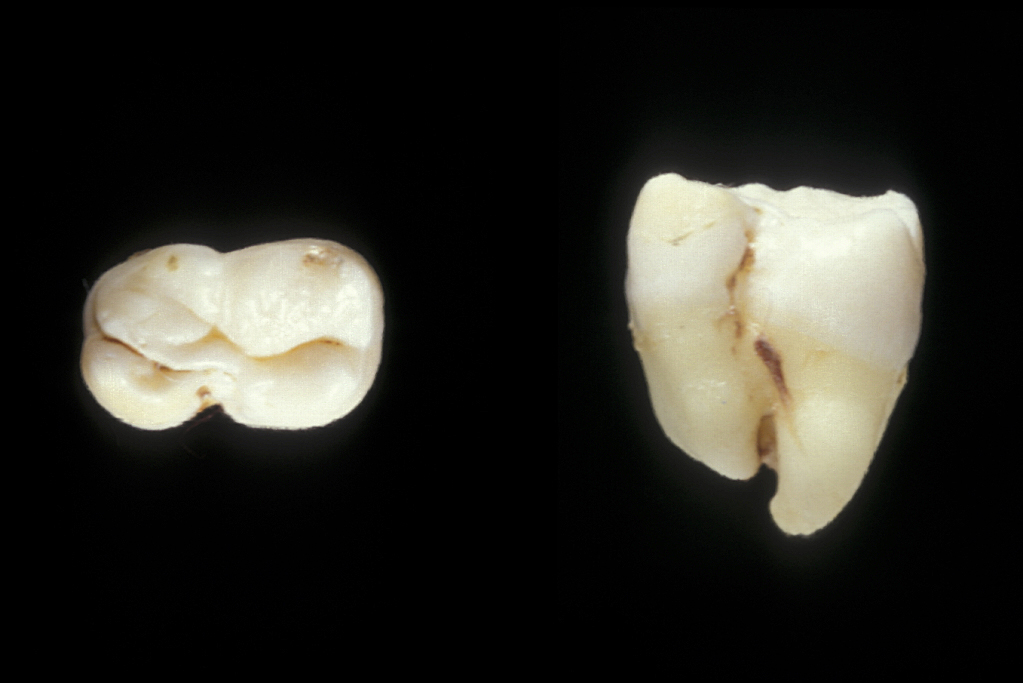
The root pattern (Figure 11) and relationship to the inferior alveolar nerve bundle, to the adjacent second molar, and to bone of the ascending ramus of the mandible can all create problems with simple elevation of third molars. Sectioning the tooth is the safest technique to overcome this. The tooth is decoronated by cutting through the amelo-cemental junction (about 80% through), then the crown is fractured off with an elevator. If the tooth is still resistant to elevation, the roots are separated by cutting through the bifurcation and elevating them individually (Figure 12).
Surgical technique for removal of upper third molars involves a buccal flap. The flap is raised with an incision either around the second molar or a ‘slash’ passing from the distobuccal cusp into the buccal sulcus (Figure 13). Bone can often be removed buccally with a Coupland’s elevator (Figure 1) and the tooth then elevated with a Warwick-James or Cryer’s elevator. Deeply placed teeth rarely cause symptoms and are probably best left alone. Beware the fused, ankylosed or multirooted upper third molar (Figure 14).

Complications in third molar surgery include:
- pain – if anticipated this can be minimised by the regular use of analgesics for the first 3 to 4 days. This is a painful procedure, common humanity dictates to prescribe adequate rather than over the counter analgesia. Pain is harder to control once it is established;
- swelling – steroids are often given when surgery is carried out under general anaesthetic, but this is unusual when the operation is carried out under local anaesthesia:
- trismus – some muscle spasm may occur during the first few days. Gentle exercises are required to prevent contracture. If there is still limitation in mouth opening at three weeks, some authorities elect to manipulate the mandible under a general anaesthetic;
- bleeding ;
- fractured mandible (rare), fractured maxillary tuberosity (part of the posterior surface of the body of the upper jaw, where the superior alveolar nerve enters the maxilla; uncommon complication) (Figure 15);
- displacement of the upper third molar into the maxillary antrum (one of the paranasal sinuses) or infratemporal fossa (cavity below the cheekbone), fortunately very rare (and scary!) (Figure 16);
- nerve injury – see below;
- dry socket – see below;
- infected haematoma – see below.


Nerve injury is an important complication of mandibular third molar removal, in particular injury to the lingual nerve – this is a common cause of medico-legal claims. The lingual nerve carries sensory fibres to the tongue, taste buds and secretomotor fibres to the submandibular and sublingual salivary glands. Injury can therefore result in loss or distortion of sensation (including taste) on the affected side of the tongue and disturbed salivation. Most patients describe abnormal sensations, such as pins and needles, tingling, or itching although some experience painful sensations (dysaesthesia).
The reported incidences of lingual nerve injury in the UK vary considerably from 0 to 15 %. Of these, most will make a full recovery within a few weeks, but recovery can take up to 12 months. However, a smaller group (approximately 0.5 %) are left with permanent sensory disturbance. Temporary disturbance of the lingual nerve is often due to retracting the mucoperiosteal flap during surgery. Permanent injuries often result from nerve division during burring.
In selected cases, exploration of the nerve may be undertaken. Scar tissue is released (neurolysis) and if the nerve is found to be injured, the segment may be excised and the cut ends sutured together or grafted. Results vary considerably but improvements have been noted in up to 75 % of cases. Timing is crucial. It has been suggested that in the absence of any sensory recovery by three to four months following injury, exploration is indicated.
Injury to the inferior alveolar nerve is less common but harder to manage. The nerve may be directly injured by the needle during the injection of local anaesthetic or may be crushed by the tooth root during elevation. Rarely the roots of the tooth may surround and encase the nerve so that elevation is unavoidable. Clues to this injury can be seen on the radiograph and when the tooth will not elevate easily (it actually feels as if it is attached by a rubber band).
Increasing availability of cone beam computed tomography scans (CBCT) can be useful in assessing lower third molars whose roots are in close proximity to the inferior alveolar nerve and helping to determine the risk of neurosensory disturbance. If such cases are identified, a decision may be made to remove the crown of the tooth only (coronectomy; see above).
Dry socket is a localised inflammation (alveolar osteitis) of a socket following extraction, most commonly the lower wisdom teeth. Typically, there is severe dull throbbing paid around 4 to 5 days after extraction and sometimes a bad taste in mouth. Pain is often exquisite, with inflammation, exposed bone and halitosis. Treatment of dry socket includes a range of local and/or systemic interventions.
An infected haematoma is a more significant problem than dry socket, mainly because the mass of a haematoma can rapidly liquefy and become pus, which will create a large abscess. Careful haemostasis prior to closing the wound can largely prevent this complication. If bleeding continues, the bleeding point needs to be identified and controlled before wound closure. If a large tense swelling develops after surgery, systemic antibacterials should be started immediately (commonly amoxicillin or ampicillin and metronidazole; either clarithromycin or clindamycin for people who are allergic to penicillin).
Canines
If problems with impacted or ectopic canines are identified and addressed early, chances of success are high with relatively minor interventions. If, however, the problem is not identified until later in life then other treatment options are required, frequently involving both orthodontic treatment and surgery. Treatment planning needs to take account of general factors, including issues such as patient desire, expectation and co-operation (Figure 17).
Management options are protean and should be fully discussed with the patient and parents/carers prior to any definitive treatment planning decisions. Informed consent should be sought as what could be a routine, though complex treatment for a patient during their adolescence, if delayed may become extremely difficult later in life.
Management options include:
- observation;
- surgical removal;
- surgical exposure and alignment;
- surgical repositioning.
Observation can be performed clinically, including vitality testing of adjacent teeth, and radiographically using a number of techniques. There are, however a number of potential problems that need to be considered before it is decided to leave the canine under observation. An ectopic canine can occasionally cause severe root resorption of adjacent teeth and this is often apparent only on radiographic investigation whilst being unsuspected clinically.
When the deciduous (primary) canine is retained, its long term prognosis is uncertain. If it is lost either there will be an unaesthetic gap or complex dental restoration will be required and that will, in all probability, have to be replaced at regular intervals. The deciduous upper canine may also suffer significant attrition by the lower permanent canine if retained for an extended period. This is concomitant with overeruption of the lower canine, potentially complicating any future dental restorative care due to the lack of vertical space in which to place a restoration.
In view of the potential long-term problems that can arise if no active treatment is undertaken, all options need to be discussed carefully. Patients with ectopic canines often have acceptable aesthetics and function, unlike patients with other types of malocclusion. The benefits of treatment are consequently less obvious and only later in life will a problem present, such as when the deciduous canine is lost.
Surgical removal of an ectopic canine should only be carried out if it is resorbing adjacent teeth, its follicle has undergone cystic change, or if retention will prevent adoption of a comprehensive orthodontic approach. The decision to electively remove a permanent canine rather than any other tooth as part of comprehensive treatment is somewhat controversial. Aligning the canine is potentially advantageous for many reasons, including the fact that some clinicians believe that it is functionally important to establish canine guidance. In addition, because canine teeth have excellent longevity, it may be useful for future restorative dental care if required or preferred over the first premolar on aesthetic grounds. This view, that the canines should always be retained, is based on a somewhat historical perspective and does not take into account changes in the pattern of dental disease. It is now accepted that as long as there is a mutually protected occlusion, canine guidance as such is not required. Prolonged treatment to align a canine is difficult to justify for aesthetic reasons or for future restorative considerations, especially as one can now expect the vast majority of adults to retain the majority of their teeth in the long term.
There are risks associated with upper permanent canine removal, including not only those associated with a general anaesthetic (which is normally required), but also iatrogenic damage to adjacent teeth and supporting structures. These risks often outweigh the benefits of removal in the vast majority of cases.
The principles of surgical removal are no different from those described for removal of retained roots. Accurate localization is essential as this affects the approach to the tooth, especially for upper canines. The vast majority are palatally positioned and therefore require a palatal flap for access. After the flap is raised, bone may have to be removed, either with chisels or a burr, and the tooth localised. It can be removed either en bloc or divided and removed in pieces. Extreme care needs to be taken not to damage adjacent roots. Occasionally the ‘broken instrument technique’ can be applied, passing the elevator through the buccal cortex or the nasal floor.
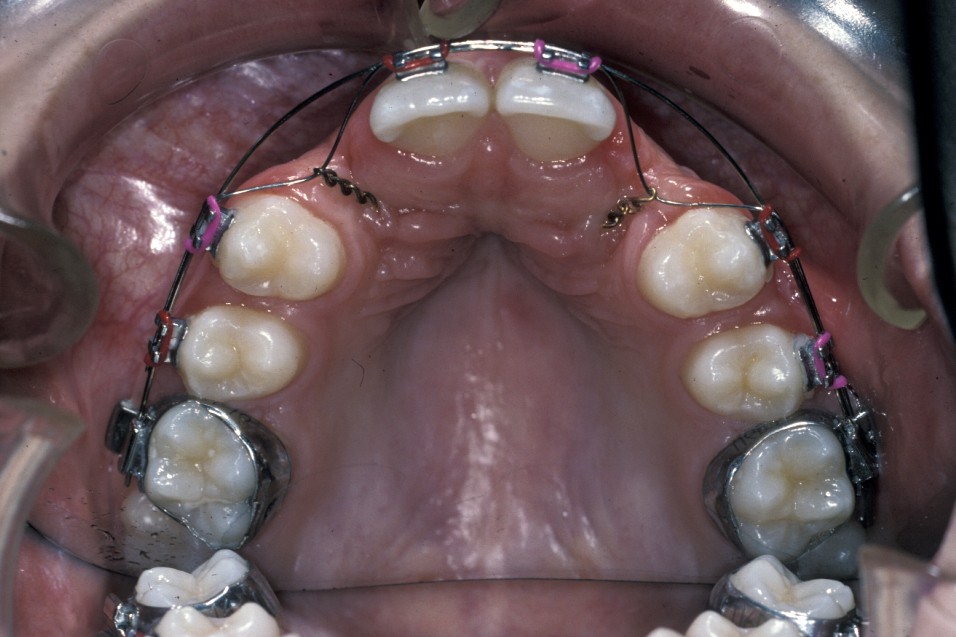
For satisfactory results to be achieved by surgical exposure and alignment of ectopic canines, complex fixed-appliances treatment for sometimes in excess of two years is required. Such appliances may include the need for dual-arch fixed appliances to allow for the use of interarch elastics and to allow arch co-ordination.
Before surgery is undertaken a decision has to be made between open or closed eruption. The aim of any exposure is to uncover enough of the crown either to place an attachment or prevent recovering of the crown during the healing phase. The most important principle of surgery is to ensure the tooth will erupt through keratinized mucosa. If this does not happen, which can occur with buccally placed canines, then the post-treatment periodontal condition will be compromised. This can obviously affect gingival aesthetics and health.
Closed eruption uses an attachment secured to the tooth to apply orthodontic traction and is useful in the treatment of markedly ectopic teeth where it would be difficult to undertake an adequate open exposure. It is often used when the canine is palatally positioned. It can be used for the treatment of buccal canines but the results can be disappointing if the attachment herniates through the thin buccal gingivae. To avoid this, the attachment should be placed either on the tip of the tooth or palatally. This is sometimes not possible because the crown position increases the risk of either excessive bone removal or iatrogenic damage to adjacent structures. It is, however, useful in the treatment of buccal canines if the crown overlies an adjacent tooth and it would be difficult to undertake an apically repositioned flap.
Surgery involves the same access as for the removal of the tooth, except that great care must be taken not to damage the cementum of the root surface as this can lead to ankylosis of the tooth and subsequent failure of eruption. An adequate amount of the crown should be exposed to allow attachment of the bracket and chain. Prior to bonding the bracket to the tooth, the area should be as uncontaminated as possible. Bleeding should be arrested as much as practicable with the use of local application of vasoconstrictors (as is added to some local anaesthetics) or the use of diathermy. Once the area is prepared, the tooth surface should be washed with saline or water and then prepared for bonding either with acid etch or with self-etch priming agents. The latter offer the advantage that they do not need to be rinsed off, need less time to prepare the tooth and are to some extent hydrophilic.
Once the tooth surface has been prepared the bracket can be secured either with chemical- or light-cured composite. The bracket should be tested to ensure that it is securely in place prior to wound closure. The chain or ligature can either exit through the wound margin on the alveolar ridge or through a stab incision elsewhere if it is felt that this would give a better vector of traction to align the tooth. With teeth that are significantly ectopic or are close to the roots of adjacent teeth, it is sometimes useful for the orthodontist to be present at the time of surgery. This allows an assessment of the relationship of the canine to adjacent structures and to plan the vector of traction that will be most appropriate.
Open eruption is often the treatment of choice for both buccally and palatally ectopic teeth.
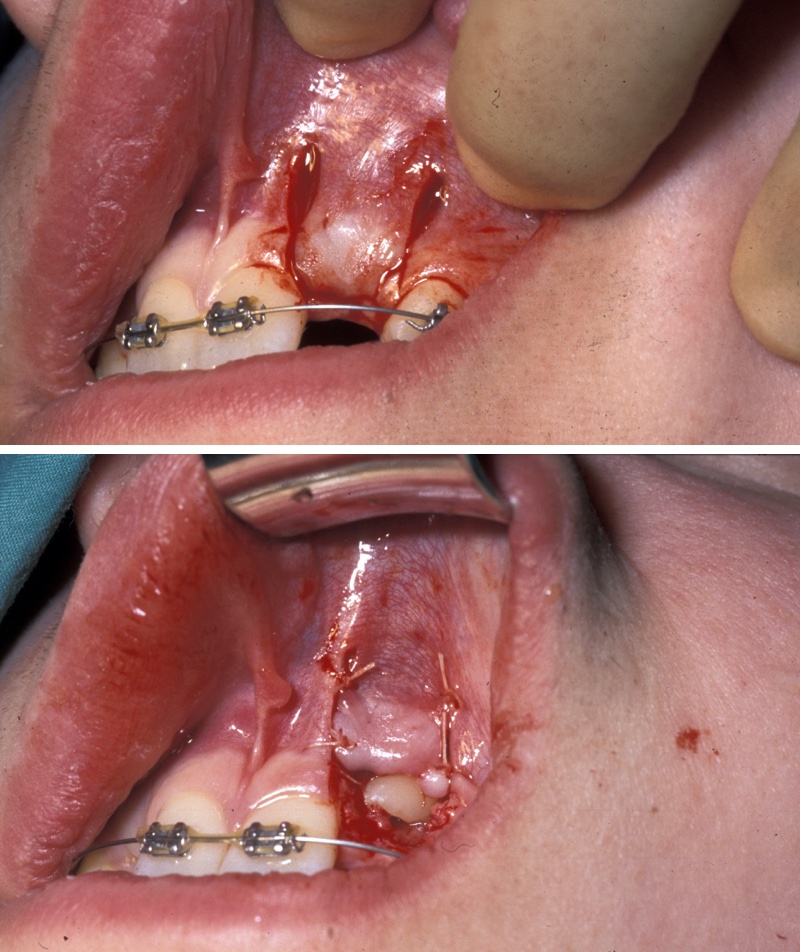
- Buccally placed canines - the most important principle here is to ensure that the tooth erupts through keratinized gingivae and this means that care has to be taken with flap design.This can effectively be achieved if an apically repositioned flap technique is utilised. A flap is raised either from the keratinized gingivae of the alveolar ridge if the area the tooth is to erupt into is edentulous, or from the gingival cuff of the deciduous predecessor which should be extracted at the same time as the surgery is undertaken. The design and direction of the relieving incisions allows the tooth to be exposed and the flap to be sutured into position, exposing an adequate amount of the crown of the canine (Figure 18).
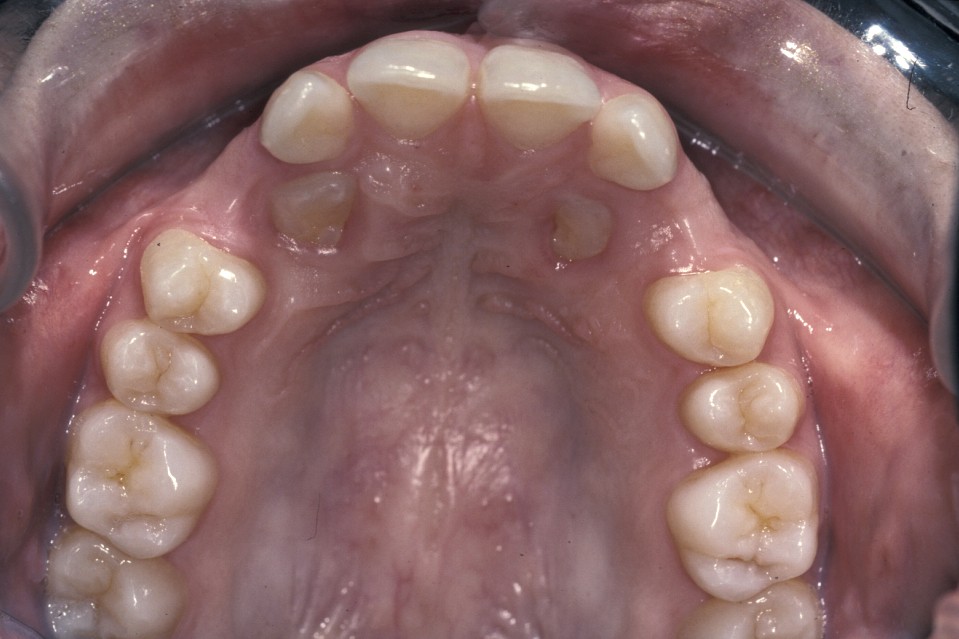
- Palatally placed canines - open eruption can also be used in the treatment of palatally ectopic canines, especially when they are relatively superficial. As the palatal mucosa is all keratinized, the problem of ensuring that the tooth erupts through here is to ensure adequate crown is exposed to ensure that there is no chance of the crown becoming recovered during the healing phase. If necessary, a bracket can be attached at the time of surgery in the same manner as for closed eruption. Care must be taken to ensure that the cementum is not damaged during surgery and that keratinized mucosa is left overlying the cementum - enamel junction. Interestingly even if large areas of bone are left denuded after surgery healing is usually excellent and uneventful. Packs can be placed over the exposed tooth to aid haemostasis, comfort and to prevent the tooth becoming covered again. This has historically involved the placing of ribbon gauze soaked in varnish and secured in place with mattress type sutures. Periodontal dressing can also be used. The pack should be removed after 7 to 14 days, from when on vigorous oral hygiene measures are vital to encourage healing, prevent gingival overgrowth and encourage eruption (Figure 19 and Figure 20).

Surgical repositioning is an alternative in some (rare) cases when fixed-appliance therapy is not acceptable. The most common indication would be for somebody who is unwilling to accept fixed-appliance therapy, has sufficient space for the tooth to be repositioned, and where it is felt possible to temporarily remove the tooth surgically without damaging it or adjacent teeth. This procedure is synonymous with tooth transplantation (see below). If space needs to be created for the tooth prior to implantation, then it can be ‘parked’ by placing it underneath the mucosa in the buccal sulcus until it is required. This maintains the vitality of the cells of the cementum and periodontal ligament.
Supernumerary teeth
Surgery is usually best undertaken under a general anaesthetic as treatment is often on relatively young patients and good access is required. If an unerupted incisor is relatively superficial, then an open eruption technique should be used. If the tooth is deep, then a closed eruption technique is probably better. In the past, some have advocated simple removal of the supernumerary teeth alone to allow eruption of the incisor teeth. Others have advocated concurrent bonding of an attachment in case orthodontic traction is subsequently required.
There is evidence that a significant proportion of incisors subsequently fail to erupt and there is then need for re-operation if supernumerary tooth removal alone has been undertaken in order to bond an attachment to allow orthodontic traction. Therefore, a decision to undertake supernumerary tooth removal alone may mean a further operation and for some placing an attachment has become the ‘default’ position. This decision will be influenced by how ectopic the incisor is, the age of the patient, the relative stage of root development and the space available. If it is felt that there is a possibility that the tooth will not erupt, then it is appropriate to attach a bracket to the tooth/teeth to allow orthodontic traction at a later date if there is no evidence of subsequent spontaneous eruption.
A bracket and gold chain is usually the attachment of choice and this allows orthodontic traction to be placed on the tooth, either using a sectional fixed appliance or removable appliance.
Surgery
A full thickness mucoperiosteal flap is raised palatally. If possible, the nasopalatine structures should be preserved, although there are few reported adverse consequences if for reasons of access they need to be transected. These structures have a tendency to bleed. The primary teeth and any overlying bone should be carefully removed in order to expose the supernumerary tooth/teeth. Only enough bone should be removed to adequately expose the tooth as excessive bone removal has no advantage and may lead to poor periodontal support. Care should be taken not to involve the exposed tooth below the cemento-enamel junction as damage to this structure can lead to ankylosis. Care should also be taken not to disturb or damage adjacent incisors. Prior to wound closure an attachment should be placed if clinically necessary.
Miscellaneous surgical techniques
Miscellaneous methods and surgical approaches that are of relevance in the context of ectopic and impacted teeth include
- tooth transplantation;
- circumferential supracrestal fibrotomy (pericision);
- single-tooth osteotomy.
Tooth transplantation is a useful technique in a small number of clinical situations. For example, transplantation has been advocated to reposition ectopic canines, to replace developmentally absent teeth or to replace a tooth lost following trauma or pathology. In most of these scenarios there are other, often more appropriate treatments but in recent years there has been renewed interest in tooth transplantation to replace upper incisors lost following trauma. The most commonly affected are the upper anterior segment incisors, lost either due to root fracture, periapical infection, ankyloses, or external/internal root resorption (Figure 21).

Premolar transplantation to replace lost central incisors does not really work as they do not have adequate mesiodistal width for this to be a good aesthetic alternative. They can substitute for lateral incisors. This is an especially useful treatment choice if teeth are crowded and would require premolar extractions as part of a course of comprehensive orthodontic treatment anyway.
The technique can be used for any ectopic teeth, such as canines, where a decision has been made to undertake transplantation rather than orthodontic alignment. Teeth should be transplanted just prior to, or on the completion of, root formation, ideally when there is still an open apex. In these situations, there is the possibility of revascularization and possibly re-innervation of the transplanted tooth.
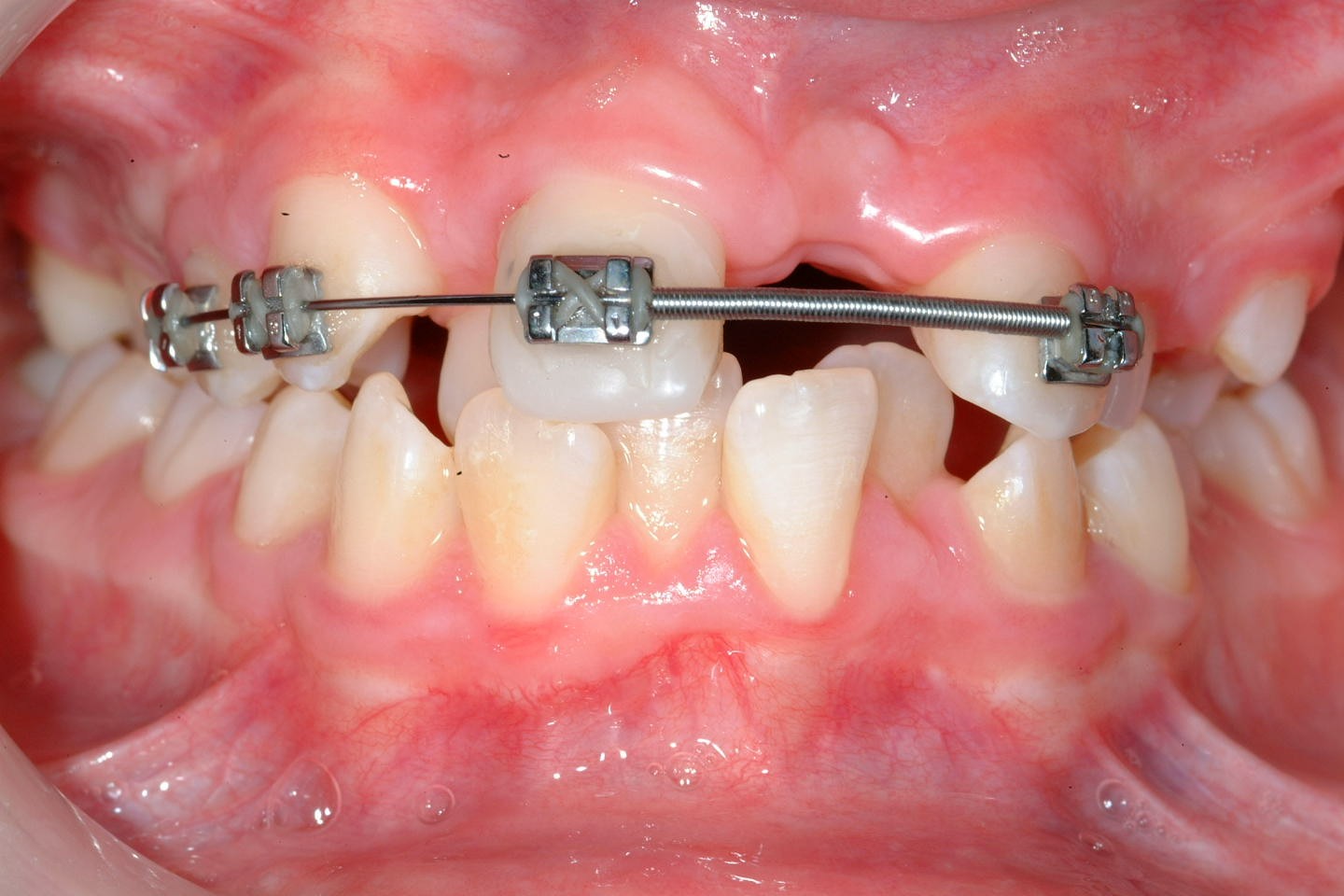
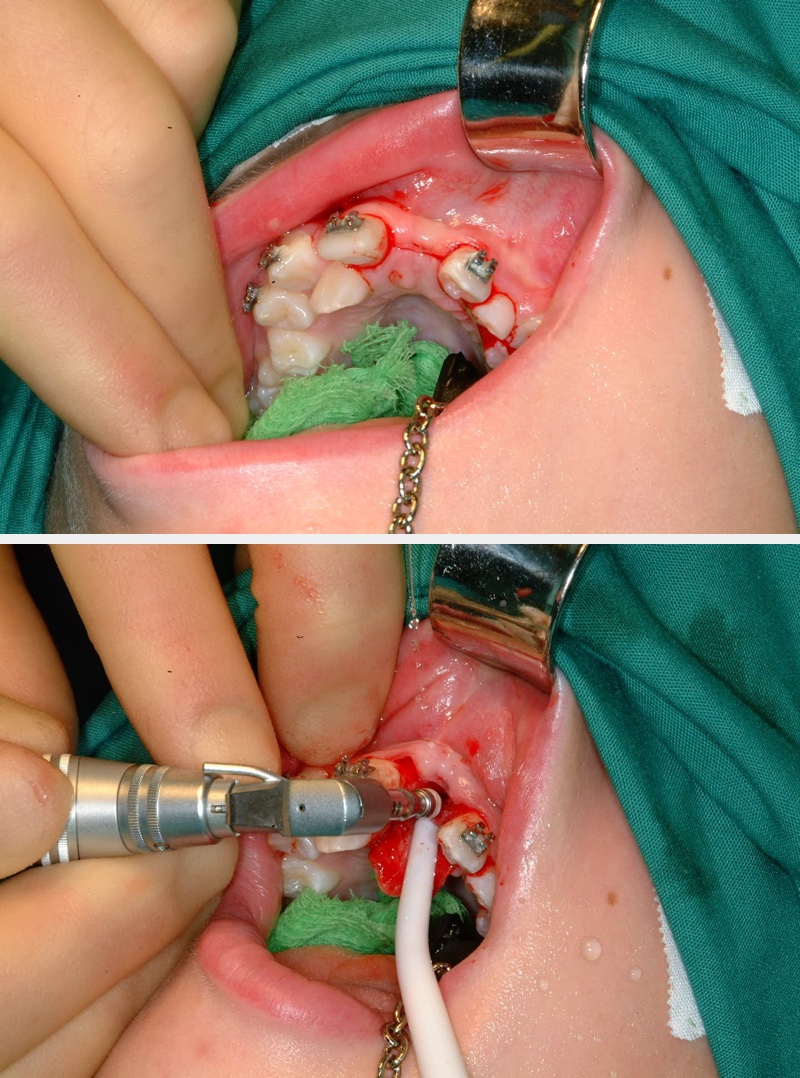
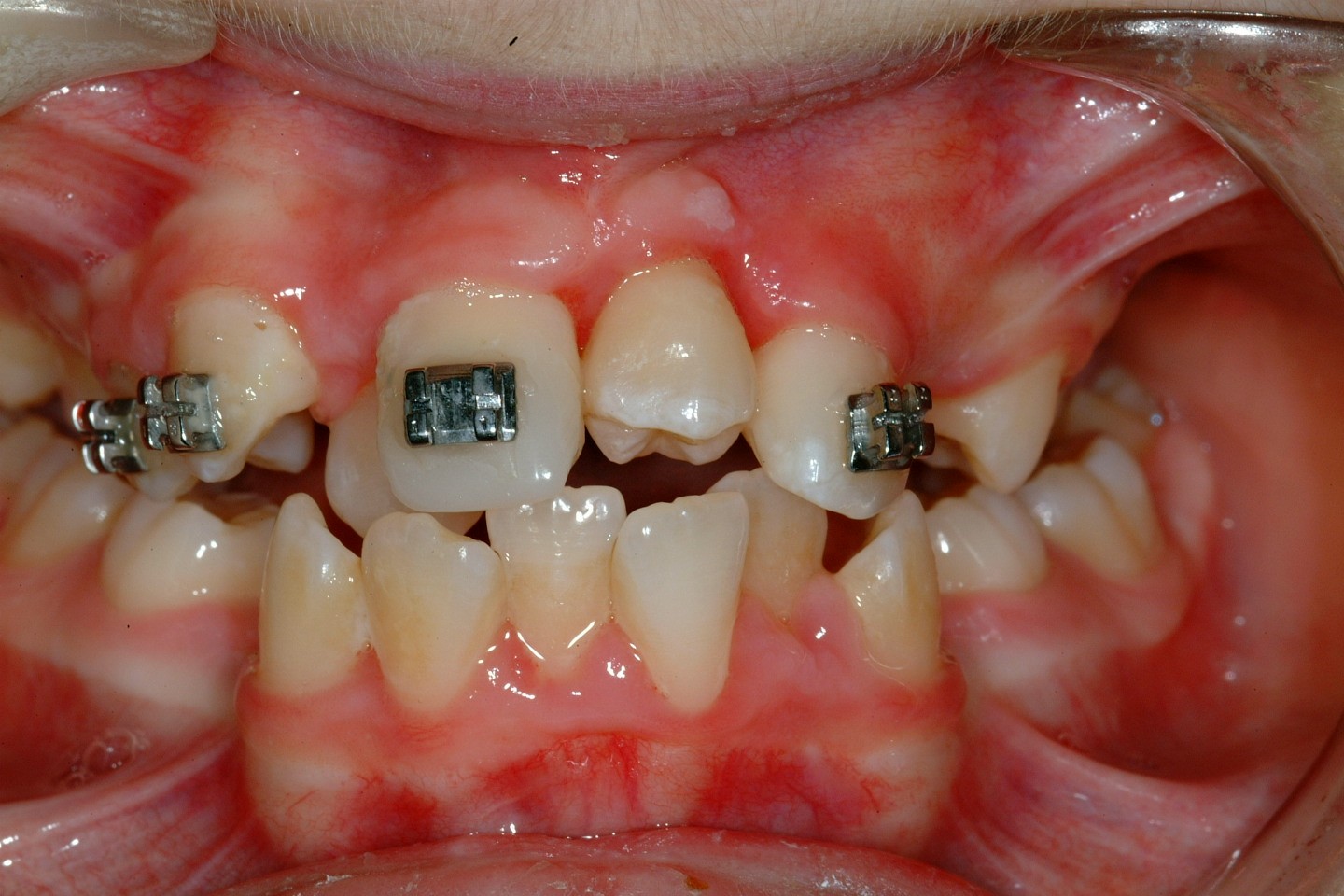
Preoperatively space is created orthodontically (Figure 22). A socket is prepared to accept the tooth using burrs with water irrigation to prevent the bone overheating and subsequent necrosis (Figure 23). If further future eruption would be beneficial (for example in a growing patient) then again, care should be taken to prevent damage to the cementum, otherwise ankylosis may occur which would prevent further eruption.
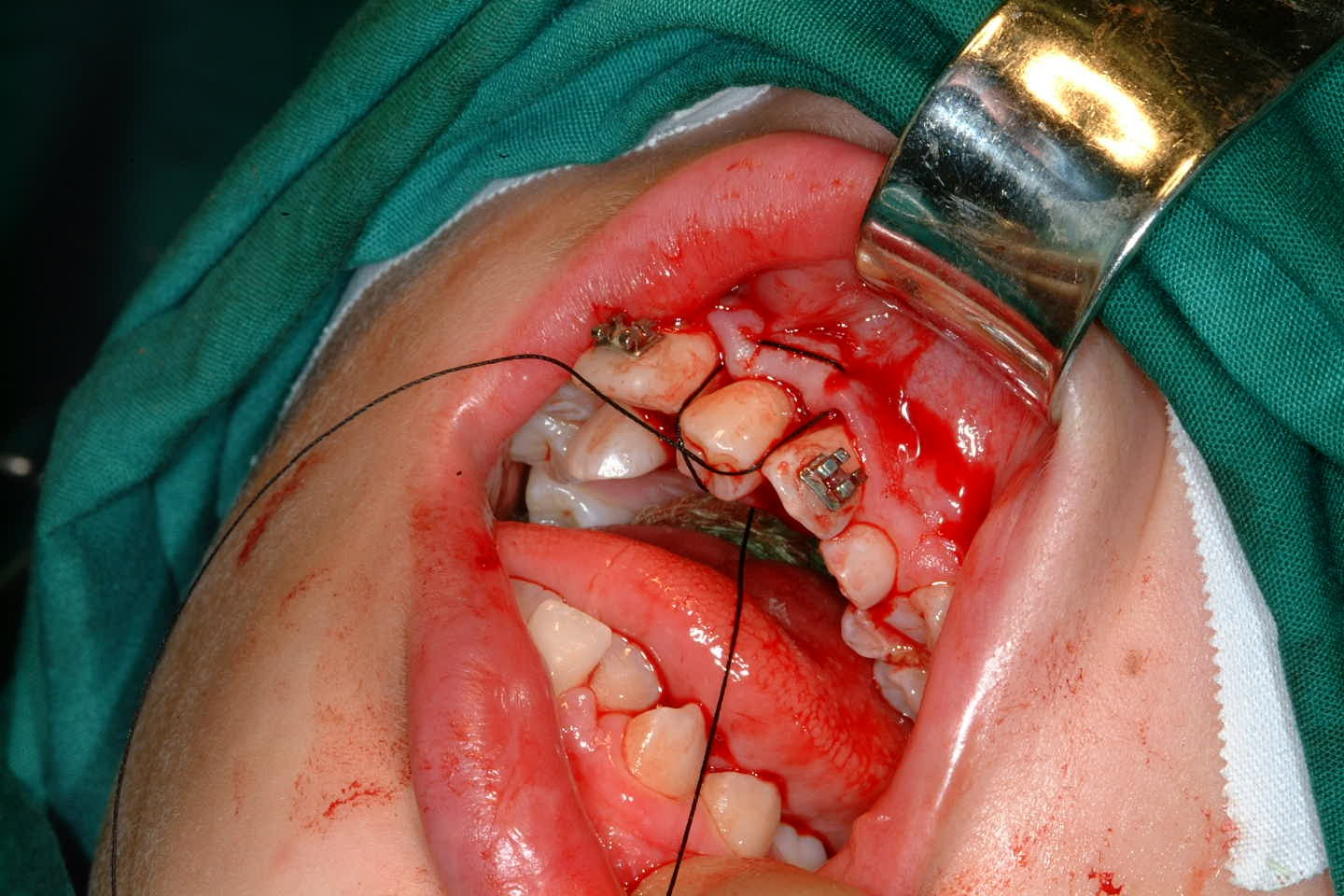
Once the tooth has been transplanted it should be splinted for between 7 and 14 days. This may be with a preformed splint cemented with a luting material or even with appropriately placed sutures (Figure 24). The area should not be disturbed during the healing phase to allow optimal healing of the periodontal ligament.
If the apex of the tooth was closed prior to transplantation then a root filling should be placed immediately. If however the apex was open at transplantation then there is still the possibility of revascularisation of the pulpal tissue. In this situation, the tooth should be reviewed using the same protocol as would be used for an avulsed (knocked out) incisor. This involves the assessment of the tooth’s colour, colour when viewed with trans-illumination, pulpal vitality (response to electrical or thermal testing) and radiographic appearance. Obviously if there is evidence of pulpal necrosis, then the pulpal tissue should be extirpated and root canal therapy instigated (Figure 25). Once good healing of the periodontal ligament has occurred and the tooth is quiescent then appropriate restorative treatment can be undertaken to improve aesthetics.
The long term success of tooth transplantation appears excellent in experienced hands and it is definitely an option to be considered in certain appropriately selected cases. There does however need to be good multidisciplinary support from other specialties, such as paediatric and restorative dentistry, in order that optimal results can be achieved (Figure 26, Figure 27).


Circumferential supracrestal fibrotomy (or pericision) is a technique used to prevent or reduce relapse of rotated or severely ectopic teeth. Following orthodontic treatment the majority of fibres in the periodontal ligament rearrange within 4 to 6 months. The supracrestal fibres (collagen fibres of the gingiva) however do not and remain displaced in the long term. The exact mechanism of how these fibres cause relapse is poorly understood. Collagen fibres have no contractile properties which could explain relapse of tooth position towards pre-treatment position, although fibres are seen to be stretched following tooth movement. It may be the recovery of these fibres to their normal length that is responsible for the relapse seen.
Pericision involves the sectioning of these fibres in order that they reattach to the tooth in its new position. Unfortunately many studies have shown that there is not complete prevention of relapse and therefore other adjunctive retention techniques are still required if alignment is to be maintained. The sectioning of the fibres should be undertaken under local anaesthesia. A scalpel blade is passed down the periodontal ligament to the alveolar crest around the whole circumference of the tooth (Figure 28). In the lower incisor region where the gingivae is thinner and more friable, if a complete pericision is undertaken then there is the danger of gingival recession labially. In these areas therefore sectioning of the interdental papilla alone should be undertaken. This involves passing of a scalpel blade directly through the interdental papillae to the alveolar crest.

Single tooth osteotomy is very occasionally necessary undertaken to reposition a single tooth which has, for whatever reason, been impossible to align orthodontically.
This is usually a treatment of last resort and may be due to ankylosis (secondary to trauma/infection/replacement/resorption) or primary failure of eruption. Prior to the osteotomy being undertaken adequate space must be available to allow correct tooth positioning. It also has to be realised that there will be no further tooth movement or development following surgery. So, if there is significant further growth expected, then there will be relative re-establishment of the problem after treatment.
A palatal flap is raised to allow mesial and distal cuts to be undertaken through to the buccal cortex. A superior cut is also made, although due to the angle of access this cut will not pass through to the buccal side. This cut is completed via a vertical incision in the buccal sulcus above the attached keratinised mucosa. This ensures that the keratinized mucosa on the buccal side is not disrupted and the blood supply to the osteotomised segment is maintained (Figure 29). Osteotomy is made simpler by piezosurgery which minimises bone removal. Once the segment has been gently mobilised it is possible to either, reposition it immediately and immobilise it using an arch wire (Figure 30), or to undertake gentle alignment of the segment orthodontically over a period of days and weeks in a manner analogous to distraction osteogenesis. This second method is useful if the tooth is a significant distance from its desired position.