Vascular abnormalities
Contents
Vascular abnormalities cover a diverse range of conditions, with regard to the type of lesions and their extent and location(s). However, allowing for some variations, the management and treatment options for these diverse conditions fall into similar categories:
- wait & watch and other conservative approaches;
- sclerotherapy (and related);
- surgical interventions, including laser applications.
Below we describe each of these modalities in more detail. The discussion includes brief summaries of vascular abnormalities and where relevant the respective treatment modalities.
Wait & watch and other conservative approaches
Modalities involved
Apart from regular surveillance by means of various imaging techniques, a range of non-invasive treatments, mostly involving drugs, characterise this approach to the management of various vascular abnormalities. This approach may be the only one necessary for the majority of haemangiomas, until these lesions resolve by themselves. It may also be the only approach necessary for some small and asymptomatic vascular malformations, at least for some extended periods of time.
A common issue to deal with is the control of pain which, for example may occur during the proliferation phase of haemangioma, or there may be painful episodes associated with localised intra-lesion thrombosis in venous malformations. For the most part, adequate pain control is achieved by readily available over the counter analgesics such as nonsteroidal anti-inflammatories, (NSAIDs) and/or paracetamol. Pain management in conjunction with arteriovenous malformations can be more complicated and may require referral to a pain specialist.
The expansion of venous malformations in the head and neck region may be slowed by preventing extended periods of increased (hydrostatic) pressure on the lesion. This can be achieved by elevating the head of the bed. The management of venous malformations may further include the use of anticoagulants (heparin) in order to prevent intra-lesion thromboses. Such medication will also be indicated in conjunction with invasive treatment schemes (see below). Where relevant, it may be advisable to avoid oral contraceptives. Recurrence of thromboses in venous malformations is an indication for surgical intervention to block the connection between the malformation and nearby draining veins (see below).
Conservative management of lymphatic malformations may require the use of antibacterial agents for the prevention and/or treatment of infections. Recurrent infections are an indication for invasive intervention (see below), surgical or sclerotherapy. Recently, some initial promising results have been reported in the treatment of lymphatic malformations (less promising for venous and arteriovenous malformations) with the mTOR inhibitor sirolimus. The mTOR enzyme complex is the one of the key regulating mechanisms in the cell metabolism of mammals. mTOR is essential in the cellular synthesis of proteins and it activates a number of growth factors, including the growth factor for vascular endothelial cells. Sirolimus hinders this enzymatic pathway. It also has immunosuppressing properties and its most common medical applications are in the prevention of transplant rejection after renal (kidney) transplants, and as an antiangiogenic agent in the treatment of some advanced malignancies. Sirolimus has been reported to have positive effects on some complicated lymphatic malformations that had previously not been successfully treated by other conventional means and where surgical resection is not possible. No complete response of lymphatic malformations to sirolimus treatment has been reported, though. Furthermore, there is no information yet about optimum administration schemes (duration and dosage) or any long-term results and potential adverse effects. However, no opportunistic infections under sirolimus treatment have been reported to date.
Conservative management schemes for haemangioma depend on the phase of the haemangioma development (infantile haemangioma - absent or small at birth; congenital haemangioma - large at birth), and whether it is about to resolve itself over time (which most of these lesions do). A small haemangioma in an uncomplicated location may not require any intervention initially (or later on). In fact, it may take several months after birth for an infantile haemangioma to be identified.
It is important to realise that 30 to 50 % of haemangioma have a precursor which within weeks of birth becomes obvious and proliferates faster than the growth of the infant, reaching around 80 % of its maximum size by five months. This is the early proliferation phase which is followed by a slower late proliferation phase. Involution usually begins around one year of age. Awareness of this natural history is essential to the conservative management of these lesions.
Complications that mandate interventions are haemorrhage and ulcerations. Ulcerations that typically require treatment with antibacterial agents are common with haemangiomas of the lip, ear and neck. Where haemangioma involves the airway, eye or oral cavity, treatment needs to ensure that vital functions are not impaired. The traditional approach to managing such lesions (that is to attempt shrinkage) was the use of systemic and/or local (injected into the lesion) corticosteroids. In particular large lesions may require systemic application of these agents which, despite their adverse effects, have been successful. In some other cases of haemangioma in the facial region, early attempts to shrink the lesion may be necessary to prevent massive disfigurement. In many cases, after involution (shrinkage) of a haemangioma, surgical resection of, for example remaining scar tissue is necessary or desirable, for functional and cosmetic reasons (see below).
The past 10 years have seen changes in the management of haemangiomas, after the accidental discovery that propranolol (a beta-blocker, used in the treatment of high blood pressure and other cardiovascular and pulmonary conditions) given to infants to treat cardiac conditions, leads to rapid regression of haemangiomas. In nearly all cases there is an improvement of haemangioma under propranolol treatment, with only moderate adverse effects reported to date. Propranolol has rapidly replaced corticosteroids as the first-line treatment of haemangiomas. The mechanism by which propranolol causes regression of haemangioma is essentially unknown (but it is speculated that the drug triggers apoptosis (cell death) of vascular endothelial cells).
Sclerotherapy
Modalities involved
Sclerotherapy aims to damage the endothelium (lining) of a vascular malformation. The locally inflicted damage then results in inflammation, thrombosis (formation of a blood clot) and eventually leads to sclerosis / fibrosis (scarring), and shrinkage of the lesion. The sclerosing agent, effectively a potent local irritant, is injected percutaneously (through the skin) directly into the lesion(s), either with a syringe or through a catheter. This mode of application usually requires monitoring by some imaging methodology, for example real-time ultrasound screening in order to ensure that the sclerosing agent is safely delivered to the lesion and not to any surrounding vessels and tissues.
A number of different chemicals, with different modes of action, are in use for sclerotherapy of vascular malformations in the head and neck region. Commonly used sclerosing agents are:
- absolute ethanol: a highly effective sclerosing agent causing damage to the endothelium (lining of vessels) by denaturation of cell proteins; high rate of complications including skin necrosis and ulcerations, nerve damage, excessive swelling, pain. Recent recommendations discourage its use for the treatment of vascular malformations in the head and neck region;
- ethanol gels: an alternative ethanol preparation, reducing adverse effects and making it easier to keep the agent in the malformation;
- polidocanol: a detergent that absorbs onto the cell membrane of the endothelium cells, causing disintegration of the endothelium and fibrosis inside the vessel and obliteration; may be prepared and applied as foam, with reported improved effectiveness;
-
- ethanolamine oleate: an emulsion of a fatty acid salt, causing irritation and an inflammatory response, followed by fibrosis and obliteration of the vessel. In addition, it is thought that ethanolamine oleate may also activate coagulation by triggering the release of clotting factors.
- bleomycin : a substance isolated from a bacterial strand, originally intended as an antibacterial agent but found to be too toxic for this use, owing to its cytotoxic properties. Used in chemotherapy of some malignancies but systemic use carries a substantial burden of adverse (pulmonary fibrosis) effects. Non-systemic use as a sclerosing agent by direct injection into venous or lymphatic malformations seems less prone to severe adverse effects (at least in the short term). This has become the most common application of bleomycin;
- sodium tetradecyl sulfate: a surfactant that acts on lipid molecules of the endothelium cells, stripping the lining of the vessel and causing a strong inflammatory response and inducing enhanced clotting / thrombosis; more effective in the treatment of venous malformations than lymphatic malformations;
- picibanil (OK-432) : the general immuno-stimulant properties of picibanil cause local inflammation by activating a number of cytokines (messenger molecules), sufficient to damage the endothelium enough to cause fibrosis. Picibanil has become a standard agent for the sclerotherapy of a range of lymphatic malformations. The production of picibanil involves a stage of treatment of the sample with a penicillin derivative, making picibanil an unsuitable medicinal drug for people with penicillin allergy;
- doxycycline: an antibacterial agent belonging to the class of tetracyclines, known to hinder bacterial protein synthesis. It is not yet clear how doxycycline acts as a sclerosing agent but is thought that the mechanism follows similar principles to its properties as an antibacterial agent, by impairing the growth of endothelial cells. Doxycycline causes fibrin and collagen deposits in the vessel, leading to fibrosis and obliteration;
- n-butyl cyanoacrylate (NBCA): strictly speaking, NBCA is not a sclerosing agent but acts by creating essentially a plug to block pathological communication between arteries and veins in arteriovenous malformations (sometimes referred to as embolotherapy). NBCA is a strong and fast-acting adhesive with favourable mechanical properties (tensile strength). It is otherwise used as a medicinal glue to close surgical wounds and other skin lacerations, and to stop bleeding (haemostasis). At room temperature NBCA is a low-viscosity monomer which rapidly and irreversibly polymerises on contact with moisture and negatively charged ions. Thus, injection into a blood vessel and exposure to blood will immediately produce a polymeric plug at the site of release, the injected liquid will follow the blood flow. The main drawbacks of NBCA application hence are a lack of control over the exact site(s) of delivery, and an inherent risk that the catheter tip used to deliver the chemical to the lesion may get accidentally glued to the vessel wall.
- ethylene-vinyl-alcohol copolymer (EVOH): another polymeric embolising agent used to treat arteriovenous malformations. EVOH is not an adhesive but still forms a plug when injected into a blood vessel. EVOH is a liquid at room temperature as long as it is saturated with the organic solvents dimethyl sulfoxide (DMSO). When injected into a blood vessel, the local DMSO concentration is reduced and solid polymeric EVOH forms. The polymerisation rate is slower than with NBCA, thus allowing better control over delivery site(s) and penetration into deeper areas of malformations. Disadvantages of the use of EVOH as an embolising agent are the yet unknown long-term stability and effects of the plugs. In addition, EVOH injection is very painful and will usually have to be carried out under general anaesthesia. EVOH is, however, the current favourite for intra-arterial embolisation.
Table 1 gives a summary of sclerosing and embolising agents used in
the treatment of head & neck vascular malformations
Table 1 Sclerosing agents
| Agent | Use * | Advantages | Disadvantages |
|---|---|---|---|
| Ethanol, absolute | VM LM AVM | effective sclerosant | increased risk of complications (VM, LM), some serious; risk for tissue necrosis and nerve damage (AVM) |
| Ethanol, gel | VM LM AVM | better safety profile, compared with absolute ethanol | |
| Bleomycin | VM LM | fewer adverse effects than for ethanol, but less effective for deep lesions | risk of pulmonary fibrosis; repeated injections necessary; use in children to be considered with caution |
| Policedanol | VM LM | fewer adverse effects than ethanol | effectiveness poorly documented |
| Ethanolamine oleate | VM | mild sclerosant with few adverse effects | good response to treatment overall, but variable rates of complete response reported; causes extra-vascular inflammation |
| Sodium tetradecyl sulfate | VM LM | effective sclerosant with few adverse effects | less effective for LM |
| Picibanil (OK-432) | LM | only few treatment cycles necessary; generally well tolerated | unsuitable for people with penicillin allergy |
| Doxycycline | LM | very low complication rates | unclear mechanism as a sclerosant; better response for macrocystic than for microcystic lesions reported |
| n-Butyl-cyano acrylate, NBCA | AVM | rapid plug formation and good mechanical properties of polymer | lack of ability to deliver to deep areas of lesions; risk of accidental adhesion of catheter tip to vessel wall |
| Ethylene- vinyl-alcohol copolymer, EVOH | AVM VM | adjustable polymerisation rate and good control over delivery sites | long-term effects not yet known; injection very painful |
* VM: venous malformation; LM: lymphatic malformation; AVM: arteriovenous malformation
Typical situations of head & neck vascular abnormalities managed by sclerotherapy / embolotherapy
Arteriovenous malformations are one of the classical lesions where obliteration of the ‘nidus’ (the main shunt between the arterial pressure side and the venous side) by embolisation has revolutionised treatment. This is followed by complete excision where possible.
Surgical interventions
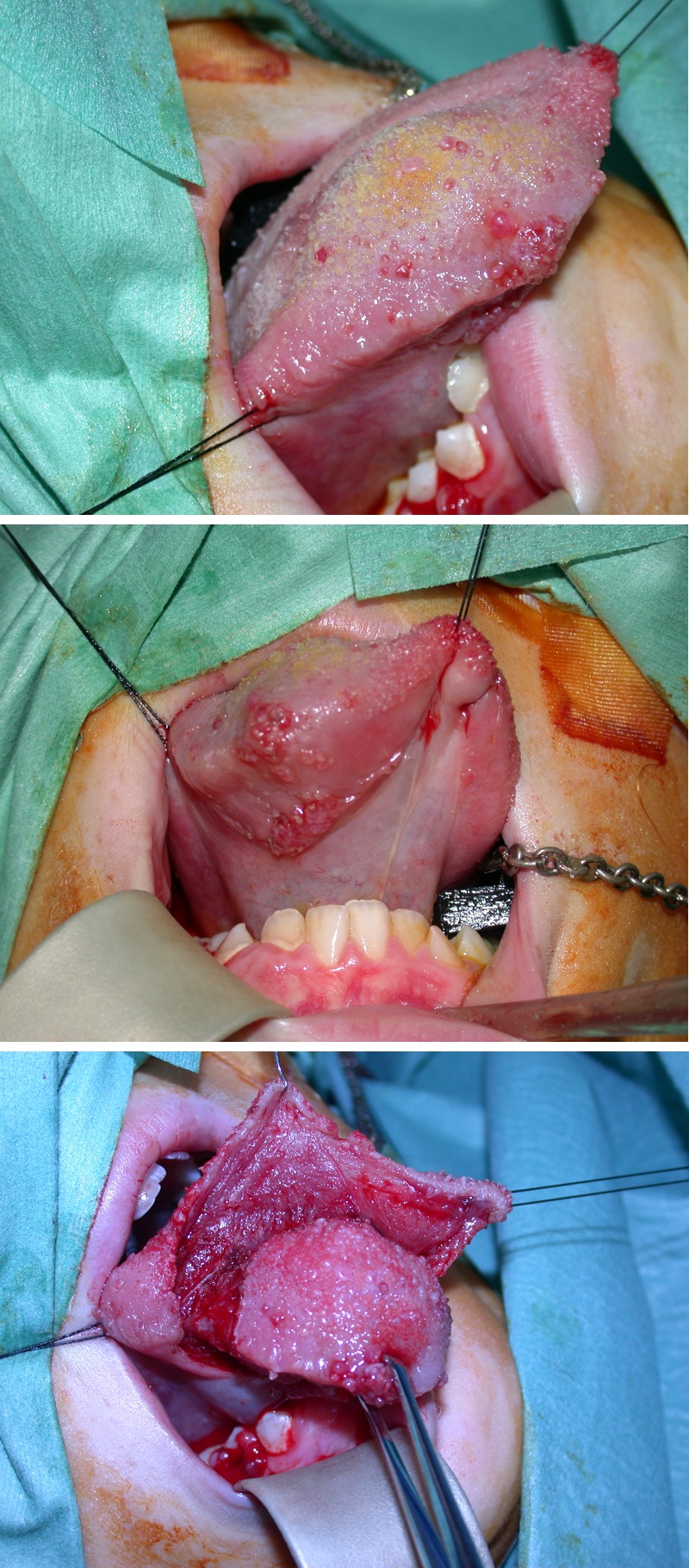
Surgical excision of these lesions is required in up to half of haemagiomata (Figure 1) and most other vascular abnormalities (usually after embolisation).
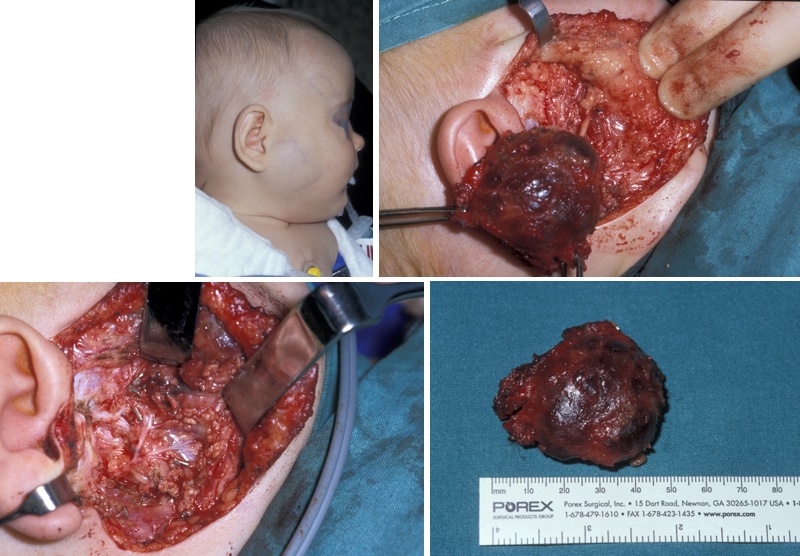
The surgery follows standard site-specific anatomical dissection with preservation of vital structures (Figure 2).
In haemagioma, lesions are very rarely interfered with during the proliferative or involuting phase for obvious reasons. Excision of the final involuted lesion is relatively straightforward and follows standard facial aesthetic techniques.
Laser photocoagulation (usually with a 595 mm pulsed dye laser) is usually done in the later stages and aims to reduce or eliminate residual staining.
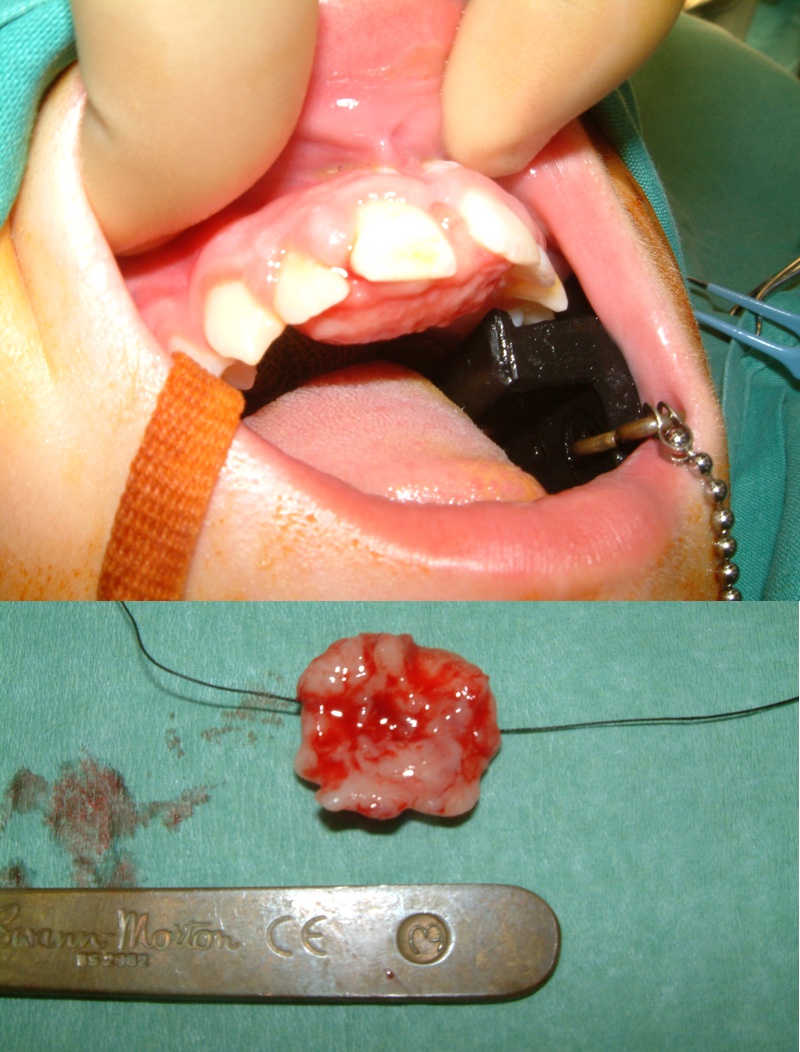
Examples of surgical treatment of macrocystic (Figure 3 and Figure 4) and microcystic lymphangiomata (Figure 5) highlight the importance of preserving functional anatomical structures where possible.
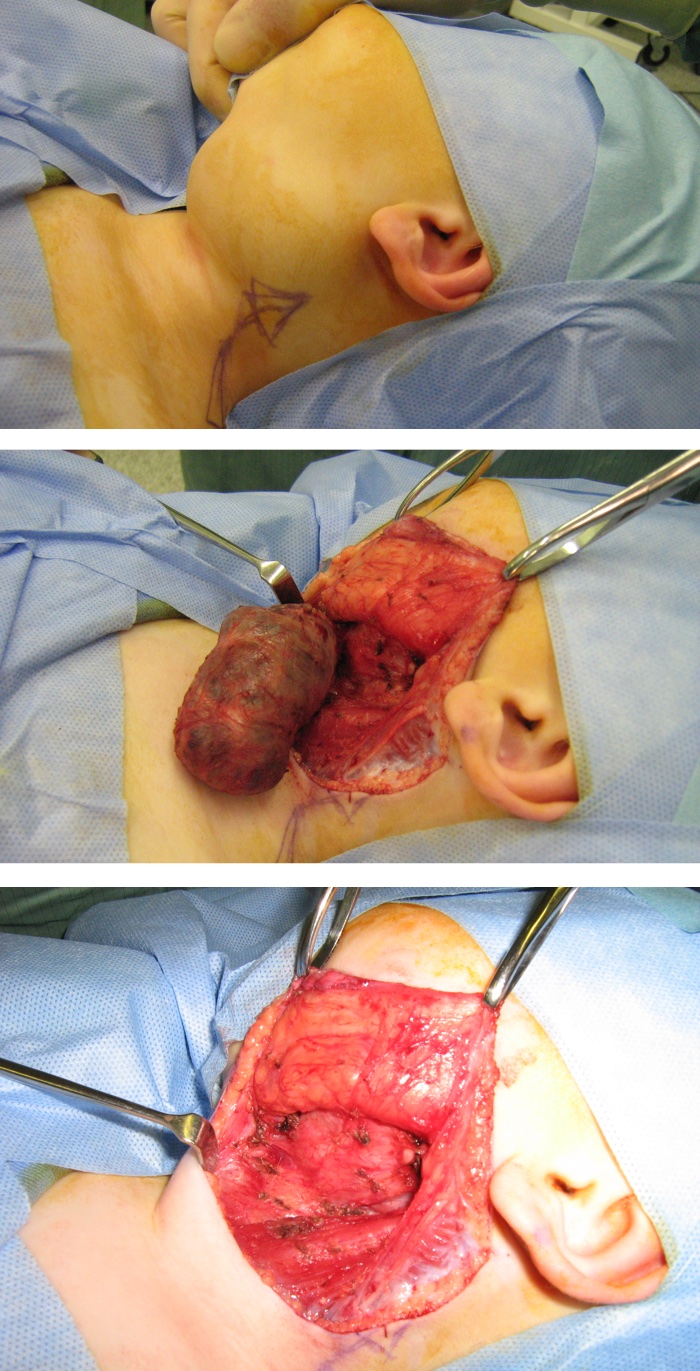
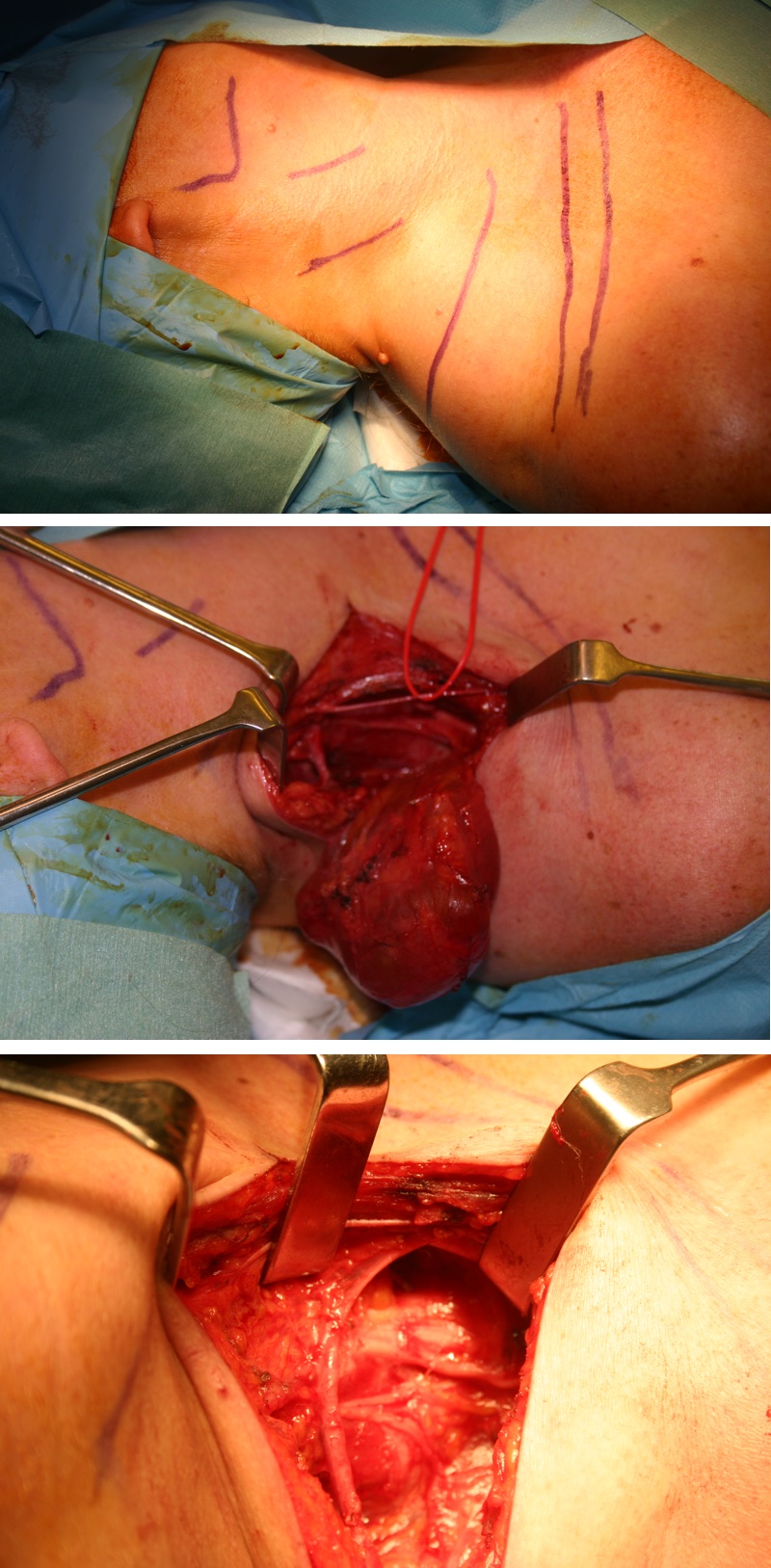
Significant surgery may be required to completely resect arteriovenous malformations and large high- and low-flow venous malformations. The general aim is to limit destruction caused by the continuous growth of lesions. Early operation on well-localised lesions which have not been previously interfered with have the highest chance of recurrence-free complete excision, minimal complications and overall success.